Translate this page into:
Multicystic encephalomalacia secondary to head trauma
Address for correspondence: Dr. Vivek Agarwal, Department of Radiology, SGPGIMS, Lucknow, Uttar Pradesh, India. E-mail: vivekagarwal0004@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Multicystic encephalomalacia (MCE) is a rare cerebral disorder seen predominantly in premature neonates. Perinatal cerebrovascular accident is believed to be the most common cause, and only a few case reports of MCE secondary to head trauma are present in the literature. Head trauma from child abuse has been documented as a rare cause of MCE in children.[1] We report a similar rare case of an infant who developed MCE secondary to head trauma.
A 6-month-old female child was brought to the neurology outpatient department with chief complaints of seizures and poor feeding. The patient had a history of fall from the bed 2 months back with sudden loss of consciousness for 30 min. The child was born at full-term with normal vaginal delivery and cried soon after birth. On examination, microcephaly was present. The patient was sent to us for further evaluation.
Computed tomography was performed that showed bilateral subdural hematomas along with multiseptated cysts involving bilateral cerebral hemispheres [Figure 1]. Subsequently, magnetic resonance imaging of the brain was done on a 3-T scanner which showed multiseptated cysts isointense to cerebrospinal fluid (CSF), in bilateral cerebral hemispheres with sparing of periventricular white matter. Volume loss in the form of thinning of the overlying cerebral cortex and ex vacuo dilatation of the third and lateral ventricles was seen. Sparing of the posterior fossa and deep gray matter nuclei was noted. Also noted were bilateral subdural collections [Figure 2].
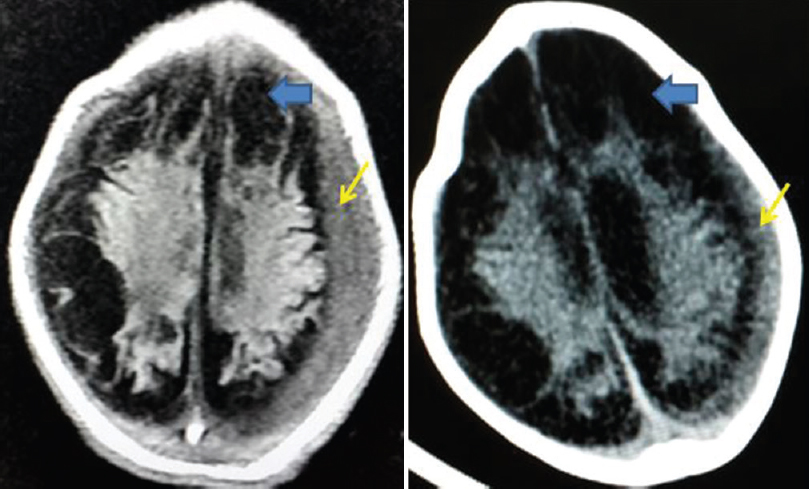
- Axial noncontrast computed tomography scan of the brain reveals extra-axial subdural hematoma (thin arrows). Also noted are multiple hypodense cysts replacing the cortex (thick arrows)
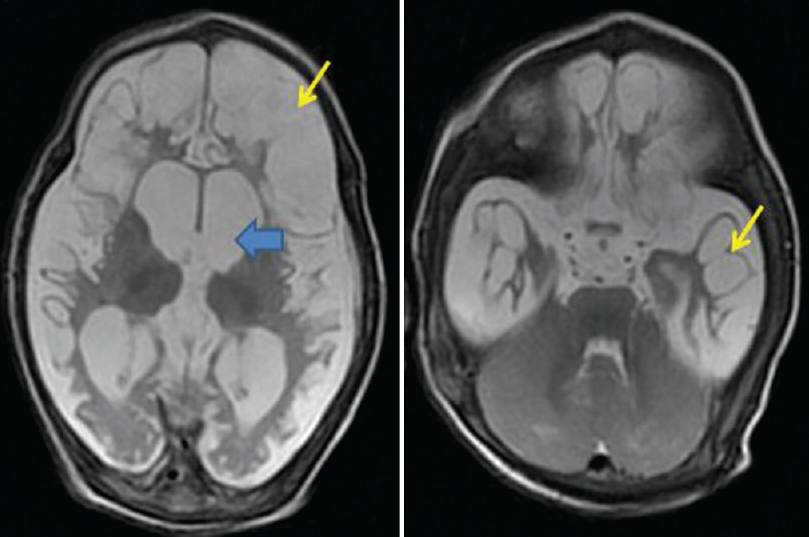
- Axial T2-weighted magnetic resonance imaging images show multiple hyperintense cysts replacing the cerebral cortex bilaterally (thin arrows). Also noted are dilated ventricles secondary to volume loss (thick arrows). Note the sparing of the cerebellum
MCE is a condition in which portions of the brain are replaced by numerous-loculated cysts in the white matter and cortex. Usually, the lesions are seen in the vascular territories of anterior cerebral artery and middle cerebral artery with sparing of temporal lobes, thalami, deep gray matter, and posterior fossa.[2] Although the distribution of the lesions suggests vascular etiology, rare causes such as trauma and intracranial infections have also been described in literature.
Neurotrauma may lead to diffuse brain edema with subsequent rise in intracranial pressure, leading to hypoperfusion of the brain.[1] Other possible mechanisms include hypoperfusion of the brain secondary to systemic hypotension due to shock or due to injury to the head and neck vasculature. Abusive head trauma may also lead to MCE. Vigorous shaking of the baby may rupture the traversing subdural veins secondary to acceleration-deceleration process leading to subdural hematomas.[3] These hematomas can eventually cause ischemic injury of the underlying gray matter secondary to mass effect leading to MCE. Proper history, skeletal survey, and fundoscopic examination for retinal hemorrhages and presence of subdural hemorrhage may help to clinch the diagnosis of MCE secondary to abusive head trauma.[4] Skeletal survey was negative for signs of a battered baby in our case.
Neonates with MCE have a poor prognosis as most of them develop severe quadriplegia and cerebral palsy since birth. Whether early surgical intervention for treatment of subdural hematomas prevents MCE is a matter of debate, and further prospective studies may be required to reach a conclusion.
Differential diagnosis includes porencephaly, glutaric aciduria Type 1, and hydranencephaly. Porencephaly presents as a smooth-walled cavity without septations unlike MCE. Glutaric aciduria is differentiated on the basis of changes in sylvian fissures and biochemical alterations. Hydranencephaly results from CSF-filled cerebral hemispheres with thinned out cortex.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Multicystic encephalomalacia as an end-stage finding in abusive head trauma. Forensic Sci Med Pathol. 2011;7:355-63.
- [Google Scholar]
- Progressive multicystic encephalopathy: Is there more than hypoxia-ischemia? J Child Neurol. 2007;22:645-9.
- [Google Scholar]
- Subdural haematomas and physical abuse in the first two years of life. Pediatr Neurosurg. 2007;43:352-7.
- [Google Scholar]
- A population-based study of inflicted traumatic brain injury in young children. JAMA. 2003;290:621-6.
- [Google Scholar]





