Translate this page into:
Mild Encephalitis with a Reversible Splenial Lesion: A Clinical Benign Condition, often Underrecognized – Clinical Case and Literature Review
Address for correspondence: Dr. Michele Pistacchi, Santorso Hospital, Garziere Street 73, 36014, Santorso, Italy. E-mail: michelepistacchi@yahoo.it
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Mild encephalitis with reversible lesion in the splenium is a clinicoradiological syndrome characterized by a variegated symptomatology with a solitary mass in the central portion of the splenium of the corpus callosum. Complete spontaneous resolution is the hallmark of this syndrome, though its pathogenesis is still unknown. We describe the clinical picture of a 51-year-old woman who developed a partial sensitive seizure, with MRI evidence of a lesion localized in the posterior portion of the corpus callosum. The patient made a full recovery thanks to the administration of antiepileptic drugs. Acquiring knowledge of this syndrome, in the wide diagnostic panel which includes vertebrobasilar diseases besides the broad range of metabolic and electrolyte disorders, is crucial to a prompt clinical diagnosis and in establishing a reliable prognosis at an early stage.
Keywords
Clinicoradiological syndrome
mild encephalitis
mild encephalitis with reversible lesion in the splenium
INTRODUCTION
Mild encephalitis with reversible lesion in the splenium (MERS) is an acute clinico-neuroradiological syndrome presenting as a solitary mass in the central portion of the splenium of the corpus callosum. MERS is characterized by mild encephalitis or encephalopathy.[1] Clinically, it may show nonspecific prodromal symptoms including cough, rhinorrhea, vomiting, headache, and sore throat. Later symptoms, such as speech difficulties, drowsiness, decreased consciousness, delirium, seizures, irritability, agitation, and disorientation, are consistent with encephalopathy.[2] This condition has also been reported in patients with epilepsy receiving antiepileptic drugs with a radiological finding of restricted diffusion and low apparent diffusion coefficient values.[34]
Complete lesion resolution in the follow-up imaging process and full clinical recovery are the hallmarks of this condition. Treatment consists only of supportive therapy. Encephalitis is defined as an acute onset of brain dysfunction in association with inflammatory changes in the cerebrospinal fluid (CSF); otherwise, it is called encephalopathy. MERS is usually associated with normal CSF findings. The reason for the transient reduced diffusion in MERS is unknown; however, transient intramyelinic edema has been postulated as a possible mechanism.[1] The pathogenesis of these lesions, however, is still uncertain, and it remains obscure whether influenza viruses or other infections cause encephalitis or encephalopathy. Its precise frequency is unknown, but it is likely underreported, since brain magnetic resonance imaging (MRI) may not be routinely performed in reversible disorders.
We describe the clinical picture of a woman with MERS so as to better figure out the clinical and neuroradiological profile of this peculiar – sometimes underrecognized – clinico-neuroradiological syndrome, including a literature review and any findings in daily clinical practice.
CASE REPORT
A 51-year-old woman with previous history of endometrial cancer surgically treated 4 years before, and arterial hypertension in pharmacological treatment, suddenly developed paresthesias in her left lower limb with a Jacksonian progression to the left upper limb lasting about 5 min. Some days later, she reported impairment of the right visual hemifield, followed by paresthesias to the left side of the body associated with headache for about 15 min. Electroencephalogram showed sharp waves in frontal derivations. Treatment with levetiracetam was proposed with prompt resolution of the crisis. MRI [Figure 1] revealed a lesion measuring 15 mm in length on the axial plane, localized in the posterior portion of the corpus callosum, hyperintense in T2 and fluid-attenuated inversion recovery sequences, hypointense in T1 sequences, without gadolinium enhancement and with high restriction in diffusion-weighted imaging sequences. Edema was absolutely absent. The neurological examination was perfectly normal.
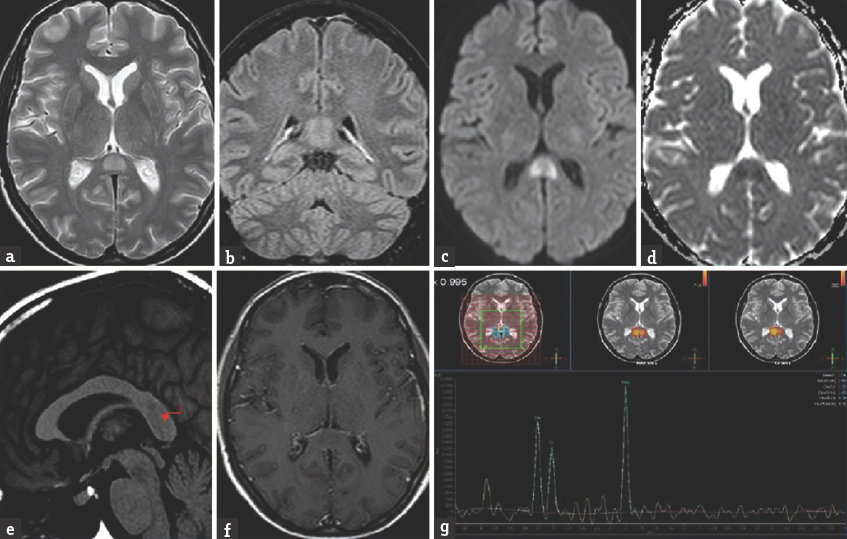
- MRI shows the lesion of 15 mm in the posterior portion of the corpus callosum on T2-immaging (a). Flair (b). diffusion weighted imaging (c and d). T1-immaging (e and f). and MRI-spectroscopy (g)
Multiple MRI follow-up [Figure 2] showed a progressive lesion reduction within 3 months without corticosteroid therapy or any other treatment, except levetiracetam.
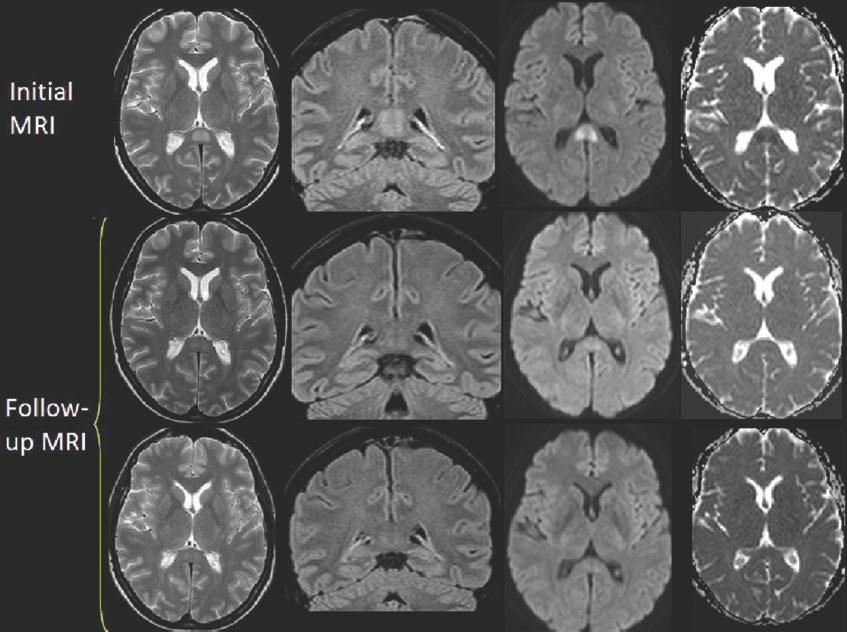
- Follow-up brain images
DISCUSSION
Transient signal abnormality of the corpus callosum on MRI is occasionally encountered in clinical practice. It has been reported in several conditions: epilepsy, multiple sclerosis, Marchiafava Bignami disease, tumors, ischemia, leukodystrophy, HIV-related encephalopathy, tick-borne and H1N1 encephalitis,[56] and damage to the blood–brain barrier (BBB); all of them can produce a transient focal edema resulting in seizures.[7] Some authors postulated that a possible antiepileptic drug toxicity could be the cause of reversible demyelination.[3] Tada speculated that viral antigens or receptors on the antibodies induced by the antigens might share affinities for specific receptors on splenial axons, inducing an inflammatory response leading up to splenium inflammation.[1] Another explanation for the pathogenetic mechanism is BBB alteration consequent to a cerebral capillary hydrostatic pressure increase, which is commonly seen in hypertensive encephalopathy, preeclampsia, posterior reversible encephalopathy, and toxic effects of cyclosporine. Oster suggested that changes in the splenium could be a consequence of energy metabolism failure in ionic transport, whose neuropathological substrate consists of reversible myelin vacuolization or intramyelinic edema resulting from excessive activity of commissural projections during seizure propagation.[345678] Finally, the fibers in the splenium, characterized by unique anatomical and physiological properties, were considered susceptible for transient signal alterations on MRI after seizure propagation, probably due to the blood supply to this anatomical area. Based on signal changes, involvement of the splenium can be divided into two types according to its shape and extent: oval and circumscribed with well-defined borders, usually located in the middle; or wider, with less regular borders and involving the entire splenium (”Boomerang sign”).[79] Involvement of the entire splenium is occasionally reported, mainly due to hypoxic injury of the corpus callosum.
Acquiring knowledge of this syndrome, particularly of morphological MRI features, is critical for the neurologist to establish a prompt and reliable pathological and functional prognosis with sufficient certainty. The differential diagnoses of splenial lesions include ischemia, posterior reversible encephalopathy syndrome, diffuse axonal injury, multiple sclerosis, Marchiafava–Bignami disease, lymphoma, and extrapontine myelinolysis. CSF examination may play a role if an infectious process is concomitant or in any causal relationship to the acute illness. In other situations, both diagnosis and prognosis can be made with sufficient accuracy thanks to clinical and neuroimaging findings. The patient we described presented a single episode with fast resolution, with no previous history of epilepsy. In the medical history of this patient, we found a gynecological disease treated without sequelae. Although it cannot be demonstrated certainly, such a monophasic pattern suggests a minor, isolated, inflammatory, or metabolic disorder, characterized by a selective tropism for the splenius fibers. The crucial element remains the correct and prompt recognizement of the peculiar radiological finding, to establish the diagnosis and prognosis with enough certainty.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors declared that they acted in accordance with ethical standards laid in the 1964 Declaration of Helsinki.
Acknowledgments
The authors would like to thank Maria Grazia Pavei, English teacher, for providing English language assistance on this manuscript.
REFERENCES
- Clinically mild encephalitis/encephalopathy with a reversible splenial lesion. Neurology. 2004;63:1854-8.
- [Google Scholar]
- Expanding the spectrum of MERS type 2 lesions, a particular form of encephalitis. Pediatr Neurol. 2013;48:135-8.
- [Google Scholar]
- Focal lesion in the splenium of the corpus callosum in epileptic patients: Antiepileptic drug toxicity? AJNR Am J Neuroradiol. 1999;20:125-9.
- [Google Scholar]
- Transient lesion in the splenium of the corpus callosum in an epileptic patient. Neurology. 2003;60:1838-41.
- [Google Scholar]
- Isolated reversible splenial lesion in tick-borne encephalitis: A case report and literature review. Clin Neurol Neurosurg. 2011;113:430-3.
- [Google Scholar]
- Transient splenial lesion of the corpus callosum in H1N1 influenza virus-associated encephalitis/encephalopathy. Intern Med. 2011;50:915-8.
- [Google Scholar]
- Transient postictal magnetic resonance imaging abnormality of the corpus callosum in a patient with epilepsy. Case report and review of the literature. J Neurosurg. 2002;97:714-7.
- [Google Scholar]
- Diffusion-weighted imaging abnormalities in the splenium after seizures. Epilepsia. 2003;44:852-4.
- [Google Scholar]
- Transient lesion in the splenium of the corpus callosum: Three further cases in epileptic patients and a pathophysiological hypothesis. J Neurol Neurosurg Psychiatry. 2001;70:459-63.
- [Google Scholar]






