Translate this page into:
Microsurgical Management for Aneurysm Arising from a Low-Lying Internal Carotid Artery-Posterior Communicating Artery Bifurcation through the Anterior Temporal Approach
Address for correspondence: Dr. Hiroshi Kashimura, Department of Neurosurgery, Iwate Prefectural Chubu Hospital, Kitakami, Iwate, Japan. E-mail: h-kashimura@pref.iwate.jp
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
A low-lying internal carotid artery (ICA) running closer to the skull base than in usual cases prevents use of the standard transsylvian approach (TSA) to view an aneurysm through the retrocarotid space. A 75-year-old male had a 10-day history of headache and left eyelid ptosis. Initial computed tomography (CT) showed no evidence of subarachnoid hemorrhage. Emergency three-dimensional CT angiography showed a saccular aneurysm with bleb arising from the left horizontally projecting ICA. The aneurysm was approached through the TSA but could not be visualized well. We used the anterior temporal approach (ATA) followed by the TSA, offering a more lateral line of vision and allowing the surgeon to visualize the aneurysmal neck. The aneurysm was successfully obliterated. The ATA provided a better lateral view than the standard TSA for the ICA aneurysm. We emphasize the effectiveness of ATA for aneurysm arising from a low-lying IC-posterior communicating artery bifurcation.
Keywords
Aneurysm
anterior temporal approach
internal carotid artery
low-lying
INTRODUCTION
A low-lying internal carotid artery (ICA) runs closer to the skull base than in usual cases, meaning that a standard transsylvian approach (TSA) cannot be used to view an aneurysm through the retrocarotid space, because the low-lying ICA narrows the retrocarotid space and impedes visualization of the aneurysm. A more lateral approach than the standard TSA is thus required to observe the aneurysm. We encountered a case of aneurysm arising from the low-lying IC-posterior communicating artery (PCoA) bifurcation, in which an anterior temporal approach (ATA) was applied. This paper describes some unique characteristics and the surgical management of such aneurysms.
CASE REPORT
A 75-year-old male presented with a 10-day history of headache and left eyelid ptosis. On admission, he was alert with no deficit other than left-side ptosis with a slightly dilated pupil and limited movement of the left eye during right gaze. Initial computed tomography (CT) showed no evidence of subarachnoid hemorrhage in the basal cistern. Emergency three-dimensional (3D) CT angiography (CTA) showed a saccular aneurysm with bleb arising from a low-lying left ICA in which the aneurysm fundus projected inferiorly [Figure 1].

- Preoperative three-dimensional computed tomography angiography, anterior-posterior view (a) showing the tortuous horizontally running ICA. Lateral view (b) showing the inferiorly projecting aneurysm with bleb. Superior-inferior view (c) showing that the segment of the C1 covers over the anterior clinoid process. A1: A1 segment of the anterior cerebral artery, AC: Anterior clinoid process, AN: Aneurysm, BA: Basilar artery, ICA: Internal carotid artery, M1, M1 segment of the middle cerebral artery, PCoA: Posterior communicating artery, PC: Posterior clinoid process, Rt: Right, *: Aneurysm
We speculated that the progressive oculomotor nerve palsy was attributable to a tiny enlargement or morphological change in the aneurysm. The aneurysm was managed by microsurgical clipping the day after admission. The cervical ICA was exposed for proximal control, and left interfascial pterional craniotomy was performed as described by Yasargil.[1] After the proximal Sylvian cistern was opened toward the ICA bifurcation, the ICA was exposed. The origin and course of the PCoA were confirmed through the opticocarotid space. The aneurysm was approached through the TSA but could not be well visualized even after mobilization of the tortuous M1 and the C1 segment, because the greater part of the aneurysm was hidden behind the left temporal lobe and tentorium cerebelli. The superficial Sylvian veins and the anterior temporal artery were detached from the temporal lobe. The arachnoid trabeculae between the oculomotor nerve and temporal uncus were then cut, and the temporal uncus was retracted posterolaterally. The aneurysm was approached through a more lateral line of vision than the TSA and was well visualized as touching the oculomotor nerve [Figure 2]. Furthermore, the aneurysm could be approached along the inferior wall of the ICA through the more lateral line of vision during ATA. The aneurysm was successfully obliterated using a bayonet-shaped titanium clip (Yasargil titanium clip, No. FT727T; Aesculap AG and Co., Tuttlingen, Germany). Complete aneurysm occlusion and patency of both the PCoA and the anterior choroidal artery were confirmed intraoperatively by indocyanine green angiography. Postoperative 3D CTA revealed disappearance of the aneurysm [Figure 3]. Improvement in third cranial nerve function was noted 3 days later, and the patient was discharged with no neurological deficits.
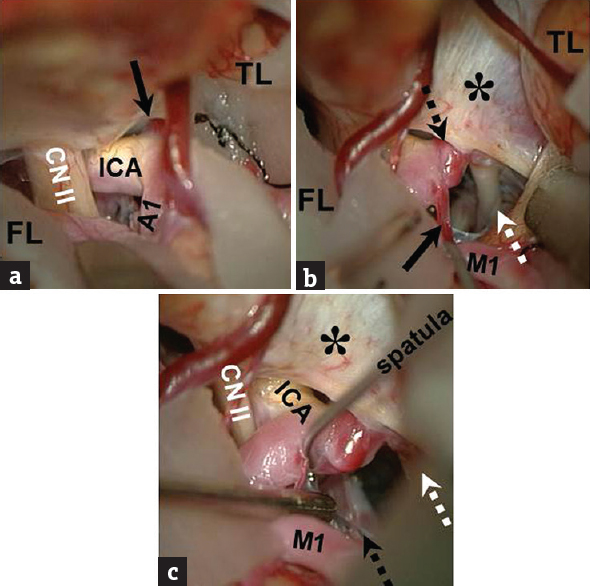
- Intraoperative photograph through the standard TSA showing that the operative corridor cannot well visualize the inferior projecting ICA aneurysm (black arrow) (a). The ATA allows to visualize the aneurysm (black dotted arrow) touching the oculomotor nerve (white dotted arrow), the anterior choroidal artery (black arrow) (b), and the PCoA (black dotted arrow). (c) CN: Cranial nerve, ICA: Internal carotid artery, A1: Segment A1 of the anterior cerebral artery, M1: Segment M2 of the middle cerebral artery, FL: Frontal lobe, TL: Temporal lobe, *: Tentorium cerebelli
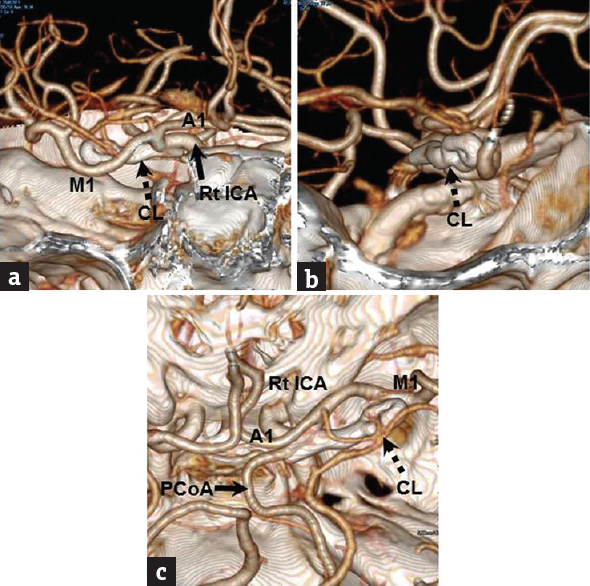
- Postoperative three-dimensional computed tomography angiography, antero-posterior view (a), lateral view (b) and supero-inferior view (c) showing disappearance of the ICA aneurysm. The direction of clip (black dotted arrow) application through the ATA is more lateral than that through the TSA. A1: A1 segment of the anterior cerebral artery, ICA: Internal carotid artery, M1: M1 segment of the middle cerebral artery, PCoA: Posterior communicating artery, Rt: Right
DISCUSSION
The ATA provided a better lateral view than the standard TSA for the ICA aneurysm and allowed better use of the retrocarotid space.[234] We emphasize the effectiveness of the ATA for an aneurysm arising from a low-lying IC-PCoA bifurcation. The term “low-lying” was based on intraoperative findings such as the short distance between the aneurysm neck and anterior clinoid process, and the anterior clinoid process impeding visualization of the aneurysm.[5] On preoperative 3D CTA, the anterior-posterior view showed horizontal projection of the low-lying ICA, while bone images revealed the ICA running closer to the skull base than in usual cases. In such situations, we recommend the ATA.
The ATA is a variation of the standard TSA but offers two major advantages compared with the standard TSA.[234] The first is the provision of a wide operative window of the retrocarotid space. The second is that the ATA allows a more lateral line of vision, eliminating the need for carotid artery retraction with the potential for aneurysmal rupture. These advantages translate to improved visualization of the aneurysmal neck arising from a low-lying ICA, despite the narrow retrocarotid space. On the other hand, the ATA shows a disadvantage in that the veins from the temporal tip to the cavernous sinus and sphenoparietal sinuses are sacrificed to retract the temporal lobe posteriorly. Katsuno et al. reported a modified ATA preserving the temporal veins.[3] Although the subtemporal approach can also provide a more lateral line of vision than standard TSA, wide exposure of lesions during the subtemporal approach often leads to excessive retraction and subsequent temporal lobe injury.[6]
Anterior petroclinoid fold resection or anterior clinoidectomy has been reported as useful to improve visualization of an aneurysmal neck arising from the low-lying ICA, through the TSA.[578] These techniques allow the surgeon to expose the proximal intracranial ICA or aneurysmal neck without changing the surgical trajectory when the retrocarotid space is narrow. However, the usefulness of these techniques may be limited to cases with an infero-posteriorly or inferiorly projecting aneurysm. In other situations such as with a posteriorly or posteromedially projecting aneurysm, adequate visualization of the aneurysmal neck for clip application might be difficult through the standard TSA. These techniques were not needed in the present case, because the lateral line of vision offered improved visualization of the aneurysmal neck.
The ATA for aneurysm arising from a low-lying ICA possesses several limitations. First, for an inferiorly projecting large aneurysm or medially projecting aneurysm, the lateral line of vision may not allow complete obliteration of the inferiorly projecting aneurysmal neck using a nonfenestrated clip and makes visualization of the medially projecting aneurysm difficult. In the former cases, fenestrated clips must be used in tandem fashion through the standard TSA, because large aneurysms have a wide neck. In the latter cases, neither the ATA nor the standard TSA would allow sufficient visualization of the aneurysmal neck. Application of a fenestrated clip through the standard TSA is thus necessary.[910]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Pathological Considerations. In: Yasargil MG, Smith RD, Young PH, Teddy PJ, eds. Microneurosurgery I. Microsurgical Anatomy of the Basal Cisterns and Vessels of the Brain, Diagnostic Studies, General Operative Techniques and Pathological Considerations of the Intracranial Aneurysms. Stuttgart: Georg-Thieme-Verlag; 1984. p. :299-301.
- [Google Scholar]
- The combined pterional/anterior temporal approach for aneurysms of the upper basilar complex: Technical report. Neurosurgery. 1993;33:244-50.
- [Google Scholar]
- A modified anterior temporal approach for low-position aneurysms of the upper basilar complex. Surg Neurol Int. 2015;6:10.
- [Google Scholar]
- Anterior temporal approach for the treatment of the posterior wall aneurysm of the internal carotid artery. Surg Cereb Stroke. 2003;31:431-5.
- [Google Scholar]
- Simple anterior petroclinoid fold resection in the treatment of low-lying internal carotid-posterior communicating artery aneurysms. Surg Neurol. 2009;72:142-5.
- [Google Scholar]
- Anterior subtemporal approach for posteriorly projecting posterior communicating artery aneurysms. Neurosurg Rev. 2007;30:203-7.
- [Google Scholar]
- Preoperative angiographical prediction of the necessity to removal of the anterior clinoid process in internal carotid-posterior communicating artery aneurysm surgery. Acta Neurochir (Wien). 1989;99:117-21.
- [Google Scholar]
- Selective extradural anterior clinoidectomy for supra- and parasellar processes. Technical note. J Neurosurg. 1997;87:636-42.
- [Google Scholar]
- Fenestrated T-bar clips in surgical management of internal carotid artery aneurysms: Technical note. World Neurosurg. 2018;117:1-3.
- [Google Scholar]
- Straight fenestrated clips in surgical management of internal carotid artery aneurysms: Technical note. World Neurosurg. 2018;116:230-3.
- [Google Scholar]






