Translate this page into:
Kümmell's disease — uncommon or underreported disease: A clinicopathological account of a case and review of literature
Address for correspondence: Dr. Manish Ranjan, Department of Neurosurgery, National Institute of Mental Health and Neurosciences (NIMHANS), Bangalore - 560 029, India. E-mail: drmanishranjan@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Kümmell's disease is a rare form of vertebral body osteonecrosis, which develops as a delayed post-traumatic event. It is infrequently reported in literature and to the best of our knowledge, has not been reported from India. We describe the clinical, radiological, and pathological features of a case occurring in a 60-year-old man and relevant brief review of the literature of this rare disease. Its close resemblance to more commonly occurring bony tuberculosis poses a diagnostic dilemma particularly in developing country like India, where tuberculosis is endemic. Awareness of this entity, though rare, is essential to avoid unnecessary diagnostic work up and treatment.
Keywords
Kümmell's disease
review
tuberculosis
vertebral body osteonecrosis
Introduction
Kümmell's disease (KD) is rare form of post-traumatic delayed avascular necrosis of the vertebral body. To best of authors knowledge, there is no reported case of KD from India. It's close radiological and histological resemblance to endemic tuberculosis of the vertebrae posses a diagnostic dilemma. We are reporting a case, whose clinical, radiological, and histological profile were compatible with KD and discuss the dilemma of diagnosing KD in Indian context.
Case Report
A 60-year-old gentleman, a laborer by profession, presented with the complaints of severe low back ache of 3 days duration and low grade fever for the past 2 weeks. There was no history suggestive of tuberculosis in the past. One year back, he had low backache of moderate intensity, precipitated by lifting and carrying heavy loads on his back, which resolved spontaneously. On clinical examination, there was focal tenderness over L4-5 vertebral levels with gross restriction of spinal movements and marked paraspinal spasm. No focal neurological deficits were detected. Routine hematological and biochemical parameters were normal except for high ESR of 94 mm/1 h (Westergren). Chest X-ray did not reveal any radiological abnormality. Magnetic resonance imaging (MRI) of lumbosacral spine [Figure 1] revealed collapse of L4 body with relatively preserved disc spaces. The collapsed L4 vertebral body was hypointense on T1W image and hyperintense on T2W image [Figure 1]. There was no area of abnormal enhancement or any prevertebral or para spinal collection. Computed tomography (CT) of spine [Figures 2 and 3] revealed L4 vertebral body collapse. He underwent L4 laminectomy, L3-5 transpedicular fixation, and the biopsy of the L4 body. Histopathology revealed thin irregular osteoporotic bony lamellae and fragments of pale ischemic bony bits [Figure 5a]. The enclosed marrow spaces revealed fresh hemorrhage bordered by clusters of foamy histiocytes as response to fresh hemorrhage reflecting trauma [Figure 5b]. There was abundant fibrin and early necrosis of the marrow without any osteoblastic or osteoclastic activity. There was no evidence of tuberculosis (absence of granulomatous pathology or acid fast bacilli). The possibility of post-traumatic avascular necrosis (KD) was suggested. As tuberculosis could not be conclusively excluded, he received antitubercular therapy (ATT).
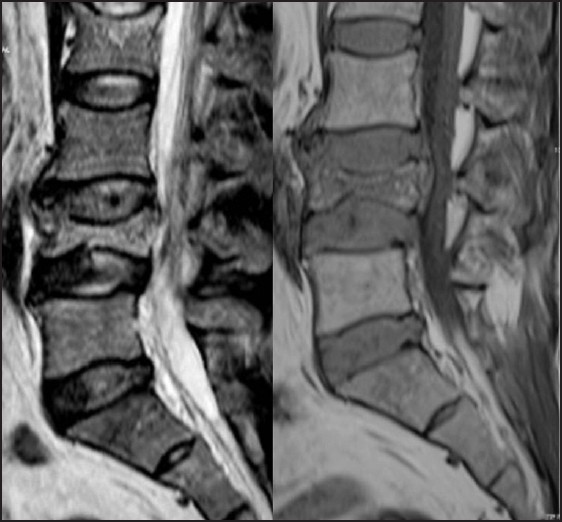
- MRI T2W and T1W images show collapse of L4 vertebra and signal changes within the collapsed body (hyperintense on T2W image and hypointense on T1W image), without pre or postvertebral collection/soft tissue and relatively preserved disc
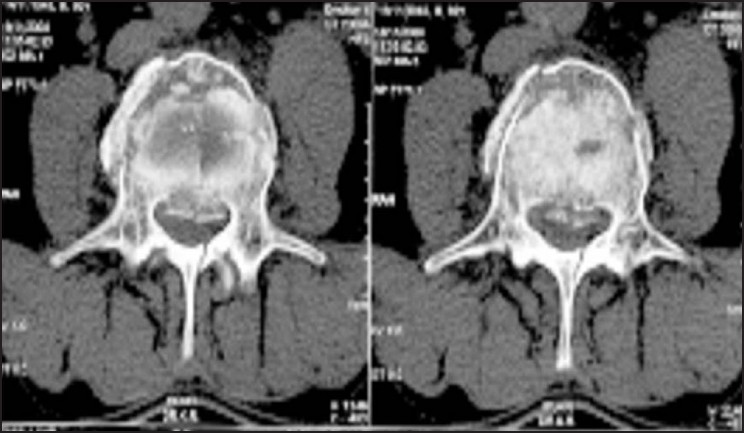
- CT axial scan through L4 vertebra show fracture of left lamina

- Sagittal reformatted CT shows collapse of vertebra with increased attenuation without evidence of bone destruction or erosion

- Coronal reformatted CT shows collapse of vertebra and presence of air within the collapsed body (Kümmell's sign)
![Histopatholgy reveal osteoporotic bony lamellae with preserved calcium lines contiguous with fragmented, ischemic bone with loss of calcium (asterix, a) closely apposing ischemic fragments, densely eosinophillic necrotic bone with remnants of osteocytes are seen. Marrow spaces showed fresh hemorrhage walled in by foamy histiocytes (b) reflecting reparative process. [a: HE×16, b: HE×240]](/content/150/2013/4/4/img/JNRP-4-439-g005.png)
- Histopatholgy reveal osteoporotic bony lamellae with preserved calcium lines contiguous with fragmented, ischemic bone with loss of calcium (asterix, a) closely apposing ischemic fragments, densely eosinophillic necrotic bone with remnants of osteocytes are seen. Marrow spaces showed fresh hemorrhage walled in by foamy histiocytes (b) reflecting reparative process. [a: HE×16, b: HE×240]
On subsequent reviewing of MRI, radiological features were not favoring tuberculosis, as the disc space was well preserved. There was no pre or paravertebral collection of inflammatory granulation tissue and the collapsed vertebral body did not have abnormal enhancement or signal changes. Review of the CT scan revealed L4 vertebral body collapse with cortical breach, linear fracture of lamina on the left side, and presence of intravertebral “vacuum cleft” on radiograph [Kümmell's sign – a retrospective observation (Figure 4)]. Clinical history was suggestive of mild trauma and delayed acute presentation, and hence, diagnosis of KD was made and ATT was stopped. Postoperatively, his pain improved significantly. At discharge, he was ambulatory without any neurological deficits. Serum ADA performed at 3 months of follow up, which was normal. At 12 months follow up, he was ambulatory and was doing well. There were no clinical signs or symptoms attributable to tuberculosis.
Discussion
KD is a rare form of delayed post-traumatic osteonecrosis, typically precipitated by mild trauma to the lower thoracic and lumbar spine. The initial pain following trauma resolves after a few days and reappear some months later.[1234] Though first described in 1895 by Hermann Kümmell, this disease is uncommon and occasionally reported in English literature,[12] possibly because of nonspecific symptomatology, difficulty in recalling trivial trauma, spontaneous resolution of initial pain, and absence of specific diagnostic tests. There is neither a consensus on the degree of initial trauma precipitating the event nor on the duration and/or degree of symptoms during the “asymptomatic” period. The term Kümmell's disease has been inappropriately applied to vertebral collapses with vacuum phenomenon, resulting in great confusion about the exact nature of cases reported as “Kümmell's syndrome”.[5] In 2002, Young et al.[2] reviewed the available English literature on KD since the 1950s and authors felt that only five cases meet the criteria set out by Kümmell. Most of reported cases are isolated case reports affecting the elderly and more frequent in males. Osteoporosis, chronic corticosteroid use, and local radiotherapy are the associated risk factor for this disorder.[126] Repetitive spinal loading in hyperflexion has been described as triggering factor for young onset KD.[7] Diagnosis usually requires exclusion of other causes of vertebral body collapse and osteonecrosis, as various disorders can cause vertebral body collapse beside trauma, which includes neoplasm, infection (especially tuberculosis), metabolic disorders, radiation, and osteoporosis. However, careful radiological review can assist in avoiding the unnecessary interventions.[6] There is no diagnostic imaging for the disease and the diagnosis remains “a diagnosis of exclusion”; however, careful review of imaging and exclusion of other common cause of vertebral body collapse on radiology is vital to avoid missing the diagnosis.
An intravertebral “vacuum cleft” on radiograph, referred to as “Kümmell sign,” is highly suggestive of ischemic necrosis and corresponds to the “double line sign” on MRI.[89] One of the most characteristic features of KD is normal radiological study immediately following trauma and subsequent development of rarefaction and loss of bone tissue leading to collapse of the vertebral body after a delay of weeks or months. Probably, the ideal investigation is serial imaging.[10] The pathophysiological basis of delayed osteonecrosis following trivial trauma is not clear. It is suggested that the initial trigger of trivial trauma results in subtle disruption in the bony spongiosa with microhemorrhages.[4] Subsequent vascular insufficiency results in impaired healing and delayed osteonecrosis.[3] The etiological contribution of vascular insufficiency is supported by finding of delayed vertebral body collapse with normal appearance on routine CT imaging but with an abnormal bone scan.[10]
In our case, though there was no histological evidence of tuberculosis, however, the diagnostic possibility of tuberculosis could not be excluded, especially in an endemic area like India and in the presence of systemic symptoms of fever and raised ESR. Histopathological review revealed osteoporotic bony lamellae, a described risk factor for Kümmell's disease in addition to the presence of necrosis, and histiocytes. Our patient was not investigated after initial trauma and we did not have the opportunity to establish the delayed radiological vertebral body collapse. However, review of the initial radiological imaging of L4 body revealed cortical breach and fracture line extending to involve whole body with presence of Kümmell's sign with conspicuous absence of features of tuberculosis. This prompted revision of diagnosis to KD and discontinuation of ATT. Reconsideration and review of the clinicoradiological and histopathology is crucial to avoid under diagnosing the KD. In one of the published cases of KD, authors could diagnose only after clinical and histopathological review, who had two biopsies at different center and even received radiation for suspected malignancy.[1]
KD in true sense is a rare disorder with no definitive diagnostic guidelines. It is really difficult not to favor the diagnosis of tuberculosis, in endemic countries like India. It is therefore possible that KD is probably overlooked/under-reported rather than nonexistent. A high degree of clinical suspicion with careful review of imaging and histopathology and clinical correlation may aid in diagnosis and avoid unnecessary work up and prolonged treatment.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Kummell's disease: A case report and literature review. Spine (Phila Pa 1976). 2008;33:E152-5.
- [Google Scholar]
- Delayed post-traumatic osteonecrosis of a vertebral body (Kummell's disease) Acta Orthop Belg. 2002;68:13-9.
- [Google Scholar]
- Delayed traumatic vertebral body compression fracture; part II: Pathologic features. Semin. Arthritis Rheum. 1981;10:271-7.
- [Google Scholar]
- “Occult” osteoporotic vertebral fractures: Vertebral body fractures without radiologic collapse. Spine (Phila Pa 1976). 2005;30:2430-5.
- [Google Scholar]
- The linear intravertebral vacuum: A sign of benign vertebral collapse. AJR Am J Roentgenol. 1998;170:1563-9.
- [Google Scholar]
- Kummell’ s disease: A rare spine entity in a young adult. Hell J Nucl Med. 2010;13:52-5.
- [Google Scholar]
- Delayed post-traumatic vertebral collapse (Kummell's disease): Case report with serial radiographs, computed tomographic scans, and bone scans. Spine (Phila Pa 1976). 1993;18:1236-41.
- [Google Scholar]






