Translate this page into:
Hypsarrhythmia and triphasic waves seem to be akin(similar) age-dependent responses of the brain to different insults
*Corresponding author: Roshan Koul, Department of Neurology, ILBS, Delhi, India. koulroshan@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Koul R. Hypsarrhythmia and triphasic waves seem to be akin(similar) age-dependent responses of the brain to different insults. J Neurosci Rural Pract. 2024;15:156-8. doi: 10.25259/JNRP_319_2023
Dear Editor,
Hypsarrhythmia (Hyps) as well as triphasic waves (TWs) is seen in patients with almost similar etiology, with the only variable being (developing) brain in Hyps and mantured (developed) brain in TWs. Hyps is exclusively reported in the first 2 years of life and TWs are rarely seen at this age.
Both Hyps and TWs were described in 1950s within a gap of 3 years.[1,2] Original description of Hyps by Gibbs was “random high voltage waves and spikes which vary from moment to moment, both in time and in location. Mostly generalized but at times originate from multiple foci”[2] [Figure 1]. On continuous video EEG monitoring, five variants of Hyps were identified.[3] These five variants include Hyps with increased interhemispheric synchronization, asymmetric Hyps, Hyps with consistent focus of abnormal discharge, Hyps with voltage attenuation, and Hyps with little spikes or sharp activity.[3]
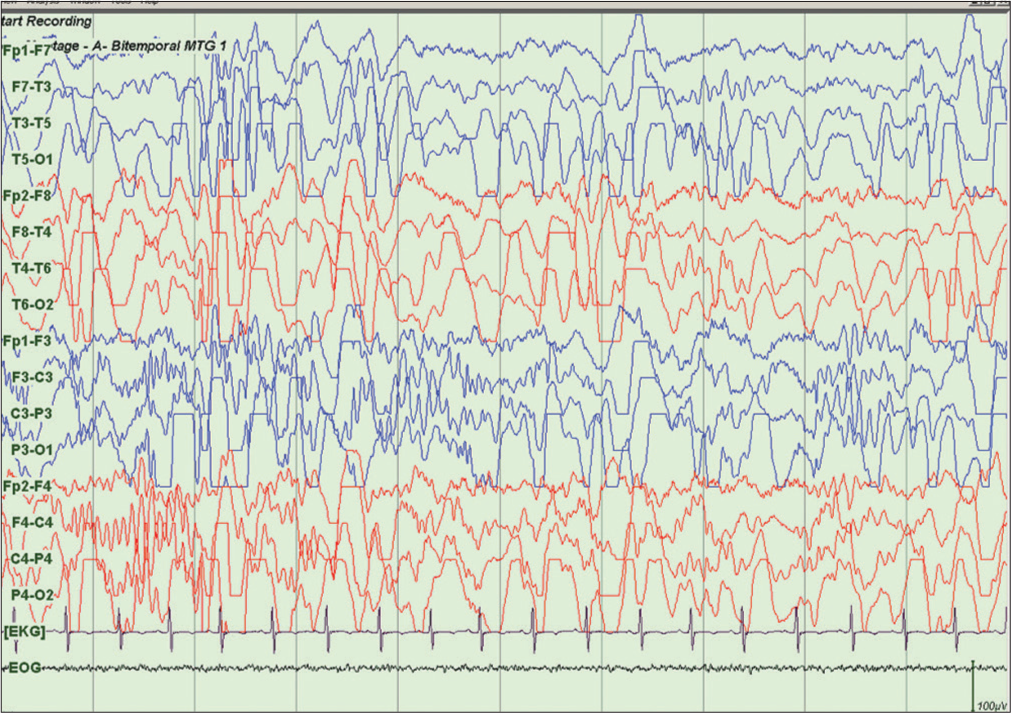
- Nine months female child with infantile spasms shows typical hypsarrhythmia pattern with sleep spindles.
TWs are three phased wave forms mostly generalized but can be atypical based on configuration.[4,5] Typical TWs are rhythmic, symmetrical, synchronous and generalized as in hepatic encephalopathy (HE) of chronic liver disease [Figure 2] and atypical are focal or asymmetric [Figure 3], seen in other metabolic, degenerative, and cerebrovascular diseases of the brain.[4,5] Raised intracranial pressure (cerebral edema) in acute liver failure modifies and attenuates the T-waves.[6]
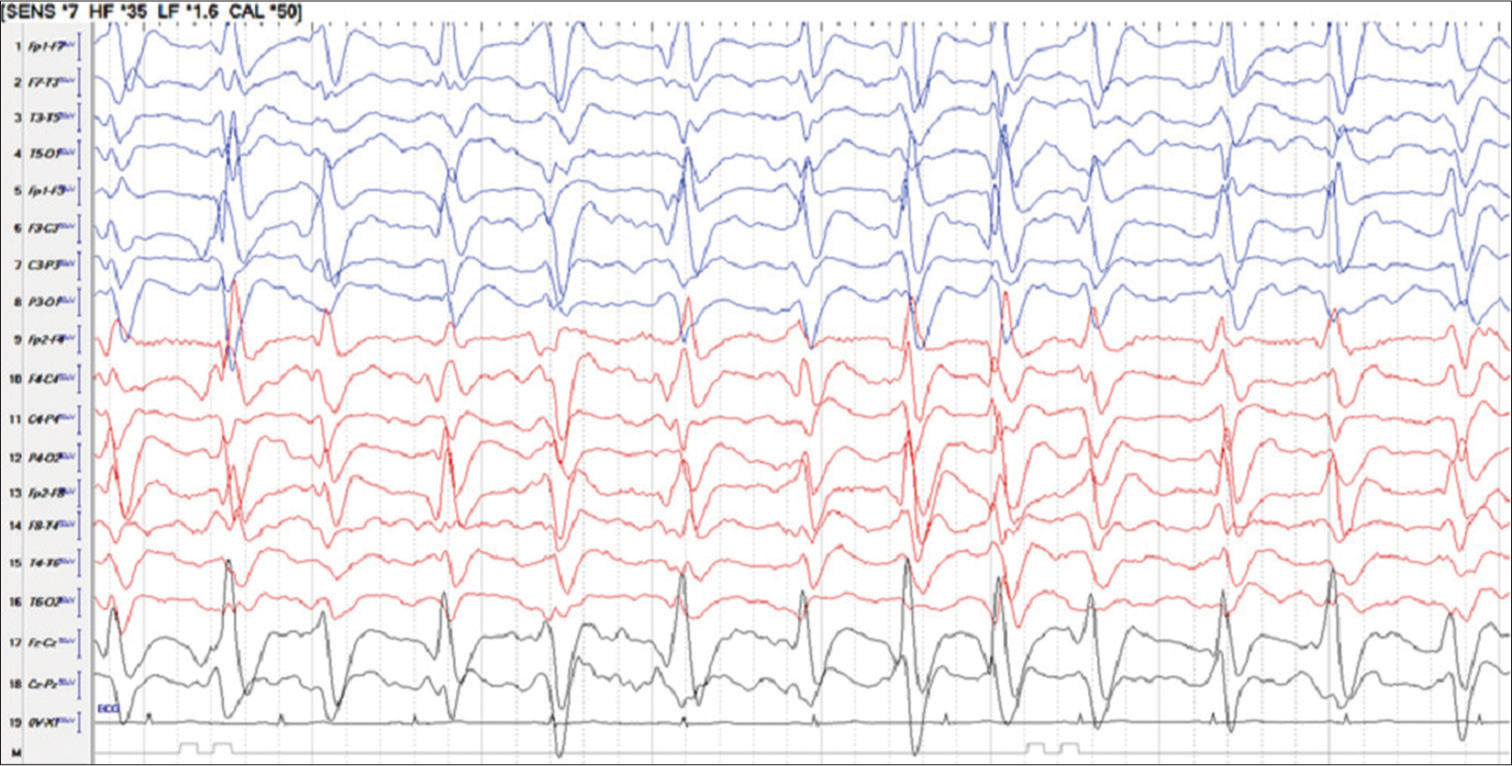
- Fifty year man with ethanol related chronic liver disease and hepatic encephalopathy shows generalized 1/s T waves.
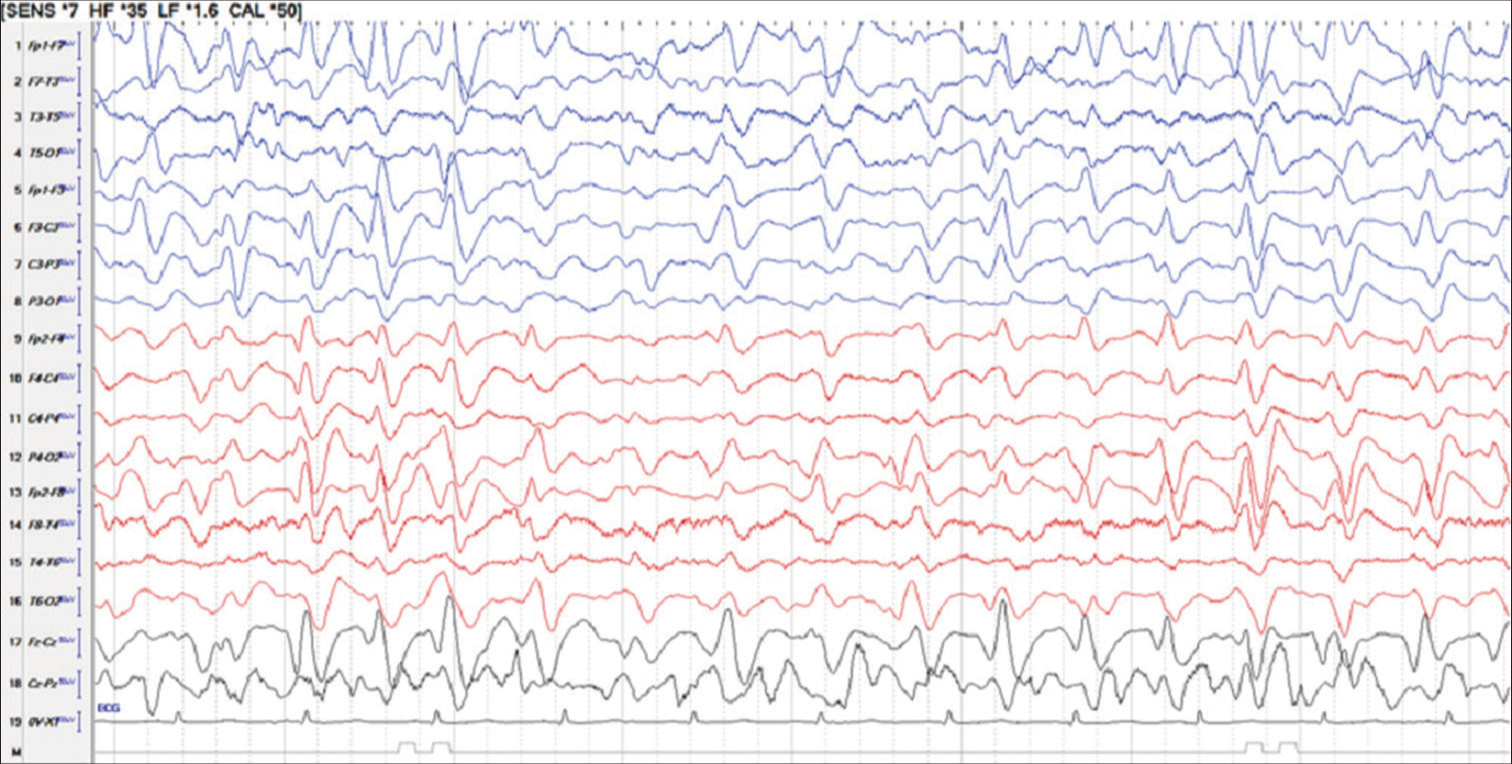
- Sixty-two year man with chronic liver disease and hepatic encephalopathy shows asymmetric T waves.
Hyps is exclusively seen in infancy, however, has also been reported in initial half of the 2nd year of life and in extreme ages of 3 months–5 years.[7] In contrast TWs are rarely seen in infancy. PubMed and Google search showed only two articles related to TWs in infancy.[8]
Little is known about pathophysiology of Hyps.[9] With limited availability of human tissues, study on various genetic animal models has revealed multifocal abnormalities of the brain.[9] Increasing number of diverse animal models available will help in future to find out pathophysiology and treatment options for Hyps and infantile spasms.[10] Hyps originates from a cortical lesion with subsequent spread to subcortical and upper brainstem structures which in turn project to lower brainstem and spinal cord resulting spasms.[10]
The origin of TWs is not well known. Even Kaplan published an article titled “what are these mysterious TWs, affair with them.”[4,5] Several locations in the brain like frontal lobes, cingulate gyrus, and thalamus have been thought to be the places of their origin.[11] Recently, TWs were reported in the white matter disease of the brain.[12] Activation of midline thalamic nuclei resulting thalamo-cortical firing similar to spindle waves may be the mechanism for production of TWs.[4] To further prove their origin, there are difficulties to produce animal models for TWs.[4]
Both Hyps and TWs indicate encephalopathy, former epileptic and later metabolic/epileptic? Hyps is seen in any brain insult during infancy and causes vary from perinatal insults including asphyxia, prematurity, intracranial hemorrhage, or hypoglycemia, neuronal migration disorders, genetic conditions, head injury, tuberous sclerosis, central nervous system infections including TORCHs, inborn errors of metabolism and immunizations.[13] The underlying etiology for Hyps is identified in about 95% cases; however, 5–15% remain cryptogenic.[13] Most children have neurocognitive delays, motor developmental delays, and refractory seizures.[13]
TWs were initially thought to be diagnostic of HE, however, have now been seen in metabolic, toxic, anoxic conditions, structural lesions, and even with drugs.[14-16] Hence, TWs are not mysterious anymore, but they represent brain response to various insults.[14] Hyps is known to be epileptic encephalopathy and responds partially to immunomodulation and antiseizure medications.[17,18] TWs indicate some form of subclinical or nonconvulsive status epilepticus.[19,20] There are several publications stating that TWs are a form of nonconvulsive seizures and have reported anti-seizure medications in them.[20] O’Rourke et al. reported response to antiseizure medications (benzodiazepines and other antiseizure medications) in 40% of their patients.[20] The authors recommend the use of antiseizure medications in all patients.[20] TWs may present as generalized periodic pattern of 1–2/s and Chong et al. too recommend anti-seizure medications.[21] Our experience too suggests trial of antiseizure medications in all patients with TWs in periodic pattern.
Hyps changes or modifies into different epileptic pattern by 2–4 years of age irrespective of underlying etiology. TWs also change depending on the underlying cause, may disappear in mild metabolic causes, and worsen in underlying severe conditions not responding to the treatment.
Mortality in both Hyps and TWs is related to the control of the underlying condition and underlying cause. A very high mortality is associated with the grade three and four HE associated with generalized periodic pattern of the TWs.[6]
TWs are not mysterious but represent brain response to various insults to the developed/mature brain while Hyps is the response of immature/developing brain to various insults.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
There are no conflict of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Atlas of electroencephalography. In: Vol. Vol 2. Cambridge, MA: Addison-Wesley; 1952.
- [Google Scholar]
- Hepatic coma: The electroencephalographic pattern. J Clin Invest. 1955;34:790-9.
- [CrossRef] [PubMed] [Google Scholar]
- Infantile epileptic encephalopathy with hypsarrhythmia. J Clin Neurophysiol. 2003;20:408-25.
- [CrossRef] [PubMed] [Google Scholar]
- Affair with triphasic waves-their striking presence, mysterious significance, and cryptic origins: What are they? J Clin Neurophysiol. 2015;32:401-5.
- [CrossRef] [PubMed] [Google Scholar]
- Typical versus atypical Triphasic waves. J Clin Neurophysiol. 2013;30:211.
- [CrossRef] [PubMed] [Google Scholar]
- Role of EEG in predicting outcome of hepatic encephalopathy patients. Electrodiagn J. 2020;60:272-88.
- [CrossRef] [PubMed] [Google Scholar]
- Chapter 13: Pediatric neurophysiologic evaluation In: Swaiman K, Ashwal S, Ferriero DM, Schor NF, Finkel RS, Gropman AL, eds. Swaiman's pediatric neurology (6th ed). Netherlands: Elsevier; 2018. p. :87-96.
- [Google Scholar]
- Maple syrup urine disease: Clinical, EEG and plasma amino acid correlation with a theoretical mechanism of acute neurotoxicity. Int J Neurosci. 1994;79:21-45.
- [CrossRef] [PubMed] [Google Scholar]
- Pathogenesis and new candidate treatments for infantile spasms and early life epileptic encephalopathies: A view from preclinical studies. Neurobiol Dis. 2015;79:135-49.
- [CrossRef] [PubMed] [Google Scholar]
- The origin of hypsarrhythmia and tonic spasms in West syndrome: Evidence from a case of porencephaly and hydrocephalus with focal hypsarrhythmia. Brain Dev. 1999;21:129-31.
- [CrossRef] [PubMed] [Google Scholar]
- Triphasic waves: Historical overview of an unresolved mystery. J Clin Neurophysiol. 2021;21:809.
- [CrossRef] [PubMed] [Google Scholar]
- White matter disease-the true source of Triphasic waves? J Clin Neurophysiol. 2021;38:359-61.
- [CrossRef] [PubMed] [Google Scholar]
- Nelson pediatric symptom based diagnosis In: Kliegman RM, Lye PS, Basel DT, eds. The hypsarrhythmia EEG pattern. Netherlands: Elsevier Inc; 2018. p. :897-929.
- [Google Scholar]
- Triphasic waves and encephalopathy in the setting of pregabalin toxicity. J Clin Neurophysiol. 2018;35:515-7.
- [CrossRef] [PubMed] [Google Scholar]
- Cefepime-induced neurotoxicity: A systematic review. Crit Care. 2017;21:276.
- [CrossRef] [PubMed] [Google Scholar]
- Summary of recommendations for the management of infantile seizures: Task Force Report for the ILAE Commission of Pediatrics Working Group. Epilepsia. 2015;56:1185-97.
- [CrossRef] [PubMed] [Google Scholar]
- Triphasic waves versus nonconvulsive status epilepticus: EEG distinction. Can J Neurol Sci. 2006;33:175-80.
- [CrossRef] [PubMed] [Google Scholar]
- Response rates to anticonvulsant trials in patients with triphasic wave EEG patterns of uncertain significance. Neurocrit Care. 2015;24:233-9.
- [CrossRef] [PubMed] [Google Scholar]
- Which EEG patterns warn treatment in the critically ill? Reviewing the evidence for treatment of periodic epileptiform discharges and related patterns. J Clin Neurophysiol. 2005;22:79-91.
- [CrossRef] [PubMed] [Google Scholar]





