Translate this page into:
How to Improve Adherence to Medication and Follow-up in Chronic Mental Illnesses: Stakeholder Views
Address for correspondence: Dr. Siddharth Sarkar, Department of Psychiatry, National Drug Dependence Treatment Centre, All India Institute of Medical Sciences, Ansari Nagar, New Delhi - 110 029, India. E-mail: sidsarkar22@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Adherence to treatment of psychotropic medication remains poor overall despite the availability of effective medications.[1] Many factors have been implicated for the poor adherence to treatment. These have included poor insight, negative attitude, or subjective response toward medication, previous nonadherence, substance abuse, shorter illness duration, and poorer therapeutic alliance.[234] Regional and ethnic variations may exist in the adherence to treatment with psychotropic medications.[5] Medication adherence and the methods to improve it is thus pragmatically ingrained within the context of service provision. Studies from India on measures to improve medication adherence in psychiatrically ill are few. Hence, this study aimed at ascertaining the problems faced in adherence and regular follow-up and the ways of addressing such problems from the perspective of patients and their caregivers.
This qualitative observational study was conducted in the psychiatry services outpatient of a tertiary care government-funded teaching hospital in South India. The hospital caters to patients with a variety of psychiatric disorders. Treatment is provided in the form of pharmacotherapy and psychotherapy. Patients with chronic psychiatric illnesses are dispensed medication from the hospital every 3 weeks. The present study included patients or caregivers aged 18–65 years; patients having the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition current diagnosis of schizophrenia, unspecified psychosis, bipolar disorder, or major depressive disorder with duration of illness of at least 1 year; and being under treatment for a period of at least 6 months. Information was gathered from the patients only if they were not in an affective episode and had no active psychotic symptoms. A caregiver was considered as a person staying with the patient for at least 1 year and accompanying the patient to the treatment facility. Patients and caregivers were interviewed by one of the researchers using a semi-structured questionnaire. Opinion was gathered from the patients and their caregivers regarding the major problems related to failure of regular medication intake and poor regular follow-up. Their opinion was also taken regarding the measures they thought would be helpful in improving the regular medication intake and regular follow-ups. The study had obtained the institutional ethics committee approval, and data collection spanned from January 2014 to December 2015.
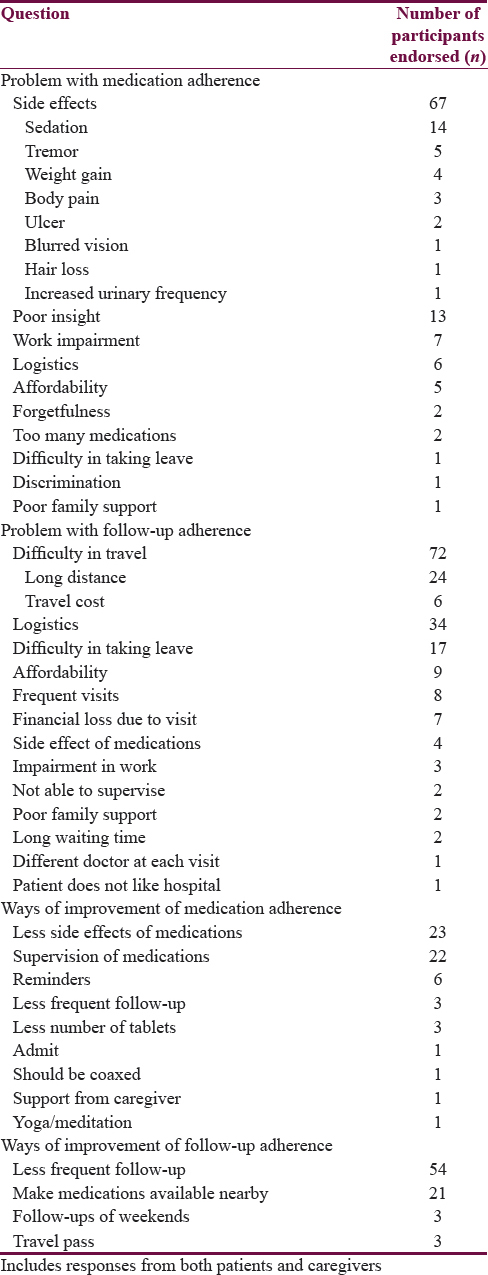
The present study included 126 patients with psychiatric disorders and 108 caregivers. The mean age of the patients was 40.0 years, while that of caregivers was 44.6 years. While 55.6% of the patients were male, 53.7% of caregivers were male. The themes about problems associated with medication adherence and regular follow-ups are summarized in Table 1. Side effects were the most common problems related to medication adherence, followed by poor insight of the patient into the need for treatment. Difficulty in travel, other logistic issues, and difficulty in taking leave from work were reported as the most common problems with follow-up adherence. Utilization of medications with less side effects and supervision of medications were the most common reported ways of improving medication adherence, while less frequent follow-ups and medications being available from nearby places (including dispensaries) were the most common reported ways of improving follow-up adherence.
The finding of the present study puts forth the perspectives of the service users who are on stable doses of medications and need long-term treatment. The issues and concerns raised are similar to that reported previously in literature.[6] Clinicians need to be cognizant of monitoring the side effect of medications, especially when the patient is on maintenance treatment. Patients and/or their caregivers need to be apprised of the potentially serious adverse events. The solutions to improving medication adherence included prescribing medications with less side effects and supervision of medications. In India, the family provides an important support, whose help can be sought for ensuring medication adherence. In addition, some patients and/or caregivers found it inconvenient to visit the hospital regularly. Difficulty in getting frequent leave for getting medications from the hospital or loss of pay for the day of hospital visit are other concerns. The suggested solutions primarily were spacing out follow-up period giving medications for longer durations and making the medications available nearby (including the primary health centers). In this regard, the objective of the National Mental Health Program to make psychiatric care easily accessible at the primary care level is commendable. This requires further concerted efforts for implementation.
The findings of the study are constrained in the limitations, including a single center experience, limited designation of themes, inclusion of selected psychiatric disorders, and focus on patients who were on “stable” treatment. Furthermore, those patients who had “dropped out” of treatment were not included and their reasons of nonadherence might be different. Despite these limitations, the study provides unique insights into the problems of adherence and solutions to cater to them from the viewpoint of the Indian service users. This stakeholder perspective would be helpful in planning services, implementing incremental quality improvement measures, and engaging in constructive dialogue for improving treatment process and satisfaction. Although all the concerns cannot be completely addressed, being aware of them might help in better service delivery. Continued and responsive attention toward concerns of the service users would help fulfill the mandate of the providing competent psychiatric treatment services to all.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Non-adherence with psychotropic medications in the general population. Soc Psychiatry Psychiatr Epidemiol. 2010;45:47-56.
- [Google Scholar]
- Prevalence of and risk factors for medication nonadherence in patients with schizophrenia: A comprehensive review of recent literature. J Clin Psychiatry. 2002;63:892-909.
- [Google Scholar]
- Psychotropic medication nonadherence among United States Latinos: A comprehensive literature review. Psychiatr Serv. 2009;60:157-74.
- [Google Scholar]
- Treatment non-adherence in affective disorders. Acta Psychiatr Scand. 2002;105:164-72.
- [Google Scholar]
- The relationship of antipsychotic medication class and adherence with treatment outcomes and costs for Florida medicaid beneficiaries with schizophrenia. Adm Policy Ment Health. 2007;34:307-14.
- [Google Scholar]
- Strategies for addressing adherence problems in patients with serious and persistent mental illness: Recommendations from the expert consensus guidelines. J Psychiatr Pract. 2010;16:306-24.
- [Google Scholar]





