Translate this page into:
Flow-diverting Stent-assisted Coil Embolization of a Ruptured Internal Carotid Artery Blister Aneurysm with the Pipeline Flex Embolization Device
Address for correspondence: Dr. Dale Ding, Department of Neurosurgery, Barrow Neurological Institute, 350 W Thomas Road, Phoenix, AZ 85013, USA. E-mail: daleding1234@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Internal carotid artery (ICA) blister aneurysms are rare and challenging to successfully treat, using contemporary surgical or endovascular approaches, without partial or complete compromise of the parent vessel. We describe the use of a resheathable flow diverter, the Pipeline Flex Embolization Device (PFED) to perform stent-assisted coiling of a ruptured supraclinoid ICA blister aneurysm in a 56-year-old female who presented with a high-grade subarachnoid hemorrhage (SAH). The first PFED was deployed across the aneurysm neck to jail a microcatheter within the aneurysm dome, and then, two small coils were delivered into the aneurysm. After removing the coiling microcatheter, the second PFED was telescoped into the first PFED. There were no postprocedural complications, and follow-up magnetic resonance angiography 15 months after embolization showed complete aneurysm obliteration. Flow-diverting stent-assisted coiling should be considered as a reconstructive, vessel-preserving, endovascular treatment option for appropriately selected patients with ruptured ICA blister aneurysms. However, future studies are necessary to assess the periprocedural safety in the setting of acute SAH.
Keywords
Blister intracranial aneurysm
endovascular procedures
flow diversion
Pipeline Flex
subarachnoid hemorrhage
INTRODUCTION
Blister aneurysms of the internal carotid artery (ICA) represent <2% of ruptured intracranial aneurysms and are pathophysiologically and morphologically distinct from conventional saccular aneurysms.[1] Unlike saccular aneurysms, which represent a focal weakness in the arterial wall and incorporate all vessel wall layers, blister aneurysms are only comprised of adventitia and fibrinous tissue, due to degeneration of the internal elastic lamina, tunica intima, and tunica media.[234] The small size and structural frailty of ICA blister aneurysms render them very challenging to successfully treat using conventional microsurgical or endovascular techniques.[567] Endovascular reconstruction of the parent artery using flow-diverting stents has emerged as an effective treatment for blister aneurysms.[8] However, flow diversion alone does not immediately occlude blister aneurysms, which can rapidly enlarge and re-rupture. In this case report, we describe the endovascular treatment of a ruptured supraclinoid ICA blister aneurysm with flow-diverting stent-assisted coil embolization.
CASE REPORT
A 56-year-old female presented with a Hunt and Hess grade V, Fisher grade IV subarachnoid hemorrhage (SAH). Cerebral angiography showed a 4-mm right posterior communicating artery (PCOM) aneurysm and a left supraclinoid ICA blister aneurysm arising immediately distal to the anterior choroidal artery [Figure 1]. Although the subarachnoid blood distribution was eccentric to the left, we decided to perform endovascular intervention for both lesions. The right PCOM aneurysm was treated with coiling alone.
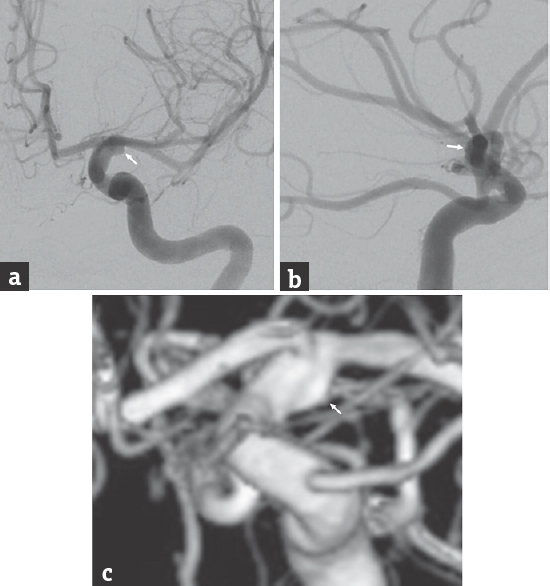
- Cerebral angiography, (a) anteroposterior projection, (b) lateral projection, and (c) three-dimensional reconstruction of a left internal carotid artery injection, shows a blister aneurysm arising from the left supraclinoid internal carotid artery immediately distal to the origin of the anterior choroidal artery (arrow)
The blister aneurysm was treated with stent-assisted coiling by navigating two microcatheters through a 6-French Flexor Shuttle guiding sheath (Cook Medical, Bloomington, Indiana, USA). A Headway 27 microcatheter (MicroVention, Tustin, California, USA) was used to deliver two telescoping Pipeline Flex Embolization Device (PFED; Medtronic Neurovascular, Irvine, California, USA) flow-diverting stents while an Excelsior SL-10 microcatheter (Stryker Neurovascular, Kalamazoo, Michigan, USA) was jailed in the aneurysm dome [Figure 2]. First, a 2.75 mm × 12 mm PFED was deployed across the aneurysm neck to jail the SL-10 microcatheter, and then, two small Target coils (Stryker Neurovascular) were deployed into the aneurysm through the jailed microcatheter. After the jailed coiling microcatheter was removed, a second 3.25 mm × 10 mm PFED was deployed within the first PFED in a telescoping configuration. The first PFED spanned from the left middle cerebral artery M1 segment to the distal supraclinoid ICA while the second PFED spanned from the distal supraclinoid ICA to the communicating segment.
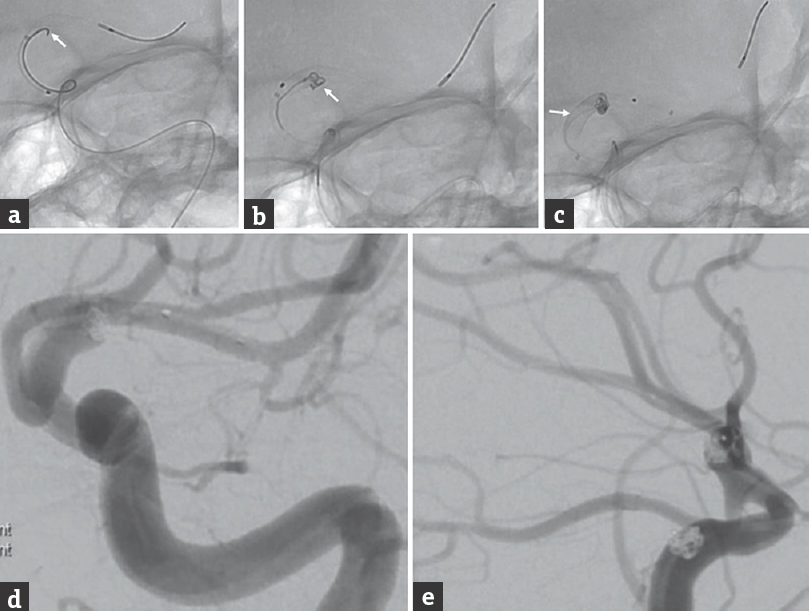
- Unsubtracted fluoroscopy, anteroposterior projection, shows (a) a 2.75 mm × 12 mm Pipeline Flex Embolization Device was partially deployed with a microcatheter jailed in the aneurysm (arrow); (b) a 1.5 mm × 4 cm Target coil (arrow) was deployed into the aneurysm, and the first Pipeline Flex Embolization Device was fully deployed; (c) a second 1.5 mm × 2 cm Target coil was deployed into the aneurysm, and a second 3.25 mm × 10 mm Pipeline Flex Embolization Device (arrow) was deployed within the first Pipeline Flex Embolization Device in a telescoping configuration. Postembolization angiography (d) anteroposterior and (e) lateral projections of a left internal carotid artery injection, shows a stable coil construct and patency of the distal branch vessels
The patient was administered 600 mg of aspirin and clopidogrel before flow diversion and maintained on a postprocedural intravenous heparin infusion for 24 h. The patient had an uneventful postoperative course and recovered to a Modified Rankin Scale of 3 at the time of transfer to the rehabilitation facility. Follow-up magnetic resonance angiography performed 15 months after endovascular treatment showed complete obliteration of both aneurysms [Figure 3].
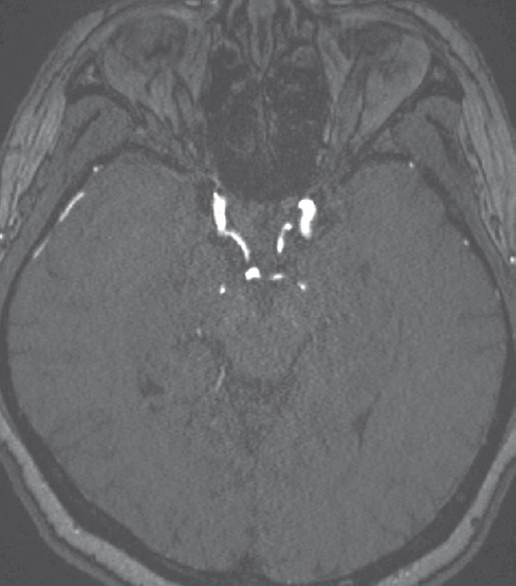
- Magnetic resonance angiography performed at 15 months postembolization follow-up, axial view, shows complete obliteration of both aneurysms
DISCUSSION
ICA blister aneurysms present unique and considerable challenges to both cerebrovascular surgeon and neurointerventionalists alike. Numerous treatment strategies have been proposed, but an optimal solution has yet to be devised for patients with ruptured blister aneurysms.[178] The standard surgical treatment for ruptured aneurysms is clipping. However, due to their pervasive fragility, direct clipping of blister aneurysms is fraught with danger. The specter of intraoperative rupture looms substantially larger during clipping of blister aneurysms, with reported rates approaching 50%, compared to the 5%–10% risk of intraoperative rupture associated with clipping of saccular aneurysms.[1]
Clipping alone may be inadequate to treat blister aneurysms since the vessel segments from which these aneurysm arise are frequently circumferentially diseased, rendering them unfit for clip application. Even when direct clipping is feasible, a portion of the parent artery is frequently incorporated into the clip configuration, causing iatrogenic stenosis of the ICA, which can result in flow-limiting cerebral ischemia and eventual infarction. In addition, intraoperative rupture of blister aneurysms may be exacerbated by attempts to clip reconstruct the aneurysm neck, which is poorly defined in these lesions, thereby culminating in an ICA laceration. These ICA tears are typically unsalvageable and require parent vessel occlusion. Given the technical difficulties associated with clipping of blister aneurysms, Meling et al. proposed the use of a high-flow bypass with ICA trapping for the surgical treatment of these lesions.[1] However, high-flow bypasses are technically demanding and expose the cortex to temporary ischemia during the anastomosis procedure. Another, simpler alternative to direct clipping is clip-wrapping although this external reconstruction of the ICA also runs the risk of causing iatrogenic stenosis and hemodynamic insufficiency.[7]
The small size and lack of a true neck generally precludes the endovascular treatment of blister aneurysms with coiling alone, due to the risk of coil prolapse or migration into the parent artery.[9] Overlapping stent constructs were previously employed to alter the local hemodynamic environment of blister aneurysms, but the advent of flow-diverting stents has led to a decrease in the usage of overlapping conventional stents.[810] However, flow diversion has not yet been proven to be the ideal solution for blister aneurysms. Specifically, blister aneurysms can enlarge in a relatively short period after endovascular therapy and re-rupture whereas remodeling of the parent vessel following flow diversion occurs over the course of months. To promote interval aneurysm thrombosis while arterial remodeling occurs, we propose the treatment of blister aneurysms using flow-diverting stent-assisted coil embolization. We believe that the ability of the newer generation PFED to be resheathed after partial deployment greatly improves the ease of this technique, compared to the first-generation Pipeline Embolization Device, which could not be resheathed.
Neither surgical nor endovascular approaches have been shown to be superior in the literature.[8] In addition, data from randomized controlled trials of intervention for ruptured saccular aneurysms cannot be extrapolated to blister aneurysms. Therefore, future studies of multicenter, prospective registries of patients undergoing treatment for blister aneurysms are necessary to ascertain the therapeutic strategy with the most favorable risk-to-benefit ratio. The implications of using antiplatelet therapy to prevent thromboembolic complications associated with flow-diverting stents in the overall management of SAH also need to be evaluated.
CONCLUSIONS
The resheathability feature of the PFED facilitates flow-diverting stent-assisted coiling of ruptured ICA blister aneurysms. This treatment paradigm may be employed for appropriately selected patients with blister aneurysms; its comparative effectiveness to flow diversion alone has yet to be analyzed. Future studies are also necessary validate the safety of flow-diverting stents in the acute setting of SAH.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Blood blister-like aneurysms of the internal carotid artery trunk causing subarachnoid hemorrhage: Treatment and outcome. J Neurosurg. 2008;108:662-71.
- [Google Scholar]
- Pathological consideration of a “blister-like” aneurysm at the superior wall of the internal carotid artery: Case report. Neurosurgery. 1997;40:403-5.
- [Google Scholar]
- Vascular smooth muscle cells in cerebral aneurysm pathogenesis. Transl Stroke Res. 2014;5:338-46.
- [Google Scholar]
- Tumor necrosis factor-α modulates cerebral aneurysm formation and rupture. Transl Stroke Res. 2014;5:269-77.
- [Google Scholar]
- Perforator aneurysms of the posterior circulation: Case series and review of the literature. J Neurointerv Surg. 2013;5:546-51.
- [Google Scholar]
- Posterior circulation perforator aneurysms: A proposed management algorithm. J Neurointerv Surg 2017 pii: neurintsurg-2016-012891
- [Google Scholar]
- Long-term follow-up of blister aneurysms of the internal carotid artery. Neurosurgery. 2013;73:1026-33.
- [Google Scholar]
- Towards a new treatment paradigm for ruptured blood blister-like aneurysms of the internal carotid artery. A rapid systematic review? J Neurointerv Surg. 2016;8:488-94.
- [Google Scholar]
- Management strategies for intraprocedural coil migration during endovascular treatment of intracranial aneurysms. J Neurointerv Surg. 2014;6:428-31.
- [Google Scholar]
- Cavernous carotid aneurysms: A new treatment paradigm in the era of flow diversion. Expert Rev Neurother. 2017;17:155-63.
- [Google Scholar]






