Translate this page into:
Factors Determining the Clinical Spectrum, Course and Response to Treatment, and Complications in Seronegative Patients with Central Nervous System Tuberculosis
Address for correspondence: Dr. Sadanandavalli Retnaswami Chandra, Faculty Block, Neurocentre, National Institute of Mental Health and Neurosciences, Bengaluru - 560 029, Karnataka, India. E-mail: drchandrasasi@yahoo.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Tuberculous meningitis remains a major health issue in the community affecting young adults of both genders predominantly from rural background. In India, the disease continues to kill 2 people every 3 min or nearly 1000 daily, according to the Tuberculosis Control Society India. Tuberculosis (TB) of central nervous system (CNS) is the most devastating form of TB. As this disease is associated with very high prevalence in young adults and will ultimately contribute to great workforce loss, we decided to assess the factors deciding the disease and its course in our patients.
Patients and Methods:
Seronegative patients with probable CNS TB and attending our outpatient department were included and followed up for 2 years.
Results:
Low body mass index, low proteins, albumin, and low CD3 and CD4, pulmonary TB appears to be a common denominator in a vast majority of these patients. Delay in diagnosis and hyponatremia contributes to morbidity. The location of exudates causes morbidity when they are seen in optochiasmal region. Bacille Calmette–Guerin (BCG) vaccination status in the community appears to be very small.
Conclusion:
CNS TB causes considerable morbidity and mortality in rural young adults resulting in severe manpower loss. Awareness into the possible role of BCG in reducing the complications of TB, role of nutrition and immunity even in seronegative patients and high-degree suspicion in medical professionals can bring down the burden of this deadly disease in the society.
Keywords
Bacille Calmette–Guerin
CD3 and CD4
central nervous system tuberculosis
onset to treatment
seronegative patients
INTRODUCTION
Tuberculosis (TB) is the one of the oldest infections known in humans since ancient times. Its history dates back to 5000 B.C. of Neolithic period. In Vedas, it is called as “Rajayakshma” (meaning “wasting disease”). In 460 BC Hippocrates called it as a fatal disease associated with coughing and weight loss. Robert Koch, a German physician, first isolated Mycobacterium tuberculosis, the bacteria that caused TB, in 1882. It is estimated that between 2002 and 2020, approximately 1000 million people will be newly infected, over 150 million people will get sick, and 36 million will die of TB.[1] In India, the disease continues to kill 2 people every 3 min or nearly 1000 daily, according to Tuberculosis Control-India.[2] TB of central nervous system (CNS) is the most devastating form of TB associated with >30% mortality and disabling neurological sequelae in >25% of survivors. In India, CNS TB accounts for approximately 5% of extrapulmonary cases or about 0.7% of all clinical TB cases,[3] and TB is the most common coinfection in immune compromised patients.[4] Other risk factors are alcoholism, malnutrition, diabetes mellitus, malignancy, corticosteroid use, over-crowding in the urban population, appearance of drug-resistant strains of TB is often related to poor compliance and an increase in migration from countries where TB is prevalent.[5] Polymorphisms in the human NRAMP1 gene may affect susceptibility to pulmonary TB in West Africans.[67] Whether genetic factors influence the prevalence of tuberculous meningitis (TBM) within a population is unknown.[8] The protective role of Bacille Calmette–Guerin (BCG) vaccination is still debated.
M. tuberculosis is an aerobic, nonmotile, nonspore-forming, and acid-fast bacillus that infects primarily humans, infection occurs through inhalation of droplet nuclei containing the bacilli, leading to deposition in the lung alveoli, interact with alveolar macrophages through a multitude of different receptors then spreads to the draining lymph nodes forming primary Ghon's complex, there exists a low-level but significant bacteremia, in which M. tuberculosis disseminates to distant sites of the body that are highly oxygenated, including the brain. In CNS, the disease begins with the development of small TB foci called Rich foci in the brain, spinal cord, or meninges, rupture of a Rich focus into the subarachnoid space heralds the onset of meningitis and less commonly as tubercular encephalitis, intracranial tuberculoma, or a tuberculous brain abscess. Tumor necrosis factor alpha (TNF-α) is essential for breaking the blood–brain barrier, microglial cells are infected and are the principal target in the CNS.[910] Production of γ-interferon from T-lymphocytes specific for mycobacterial peptides, activates microglia enabling more efficient intracellular killing of tubercle bacilli. M. tuberculosis-infected microglia also produce robust amounts of several cytokines and chemokines in vitro, including TNF-α, interleukin-6 (IL-6), IL-1 β, CCL2, CCL5, and CXCL10. Subsequent complications are related to adhesion formation, an obliterative vasculitis, and an encephalitis or myelitis.[11]
Clinical features are characterized by vague ill health lasting for 2-8 weeks before the onset of features of meningeal irritation. The non specific symptoms include malaise, anorexia, fatigue, fever, myalgia and headache. Fever was seen in 60-95% patients, headache in 50-80%, vomiting in 30-60%, neck stiffness in 25% meningism in 40-80% and confusion in 10-30% patients. Cranial nerve involvement 30–50% of patients, and sixth nerve is the most commonly affected.[12] Optochiasmatic arachnoiditis, third ventricular compression of optic chiasma, optic nerve granuloma, and ethambutol toxicity are possible factors for vision loss in these patients. Ophthalmoscopic examination may reveal papilledema, choroid tubercles, yellow lesions with indistinct borders present either singly or in clusters. Mono- or hemi-plegia appears to be the most common focal deficit. Hemiparesis is noted in 10–20% and paraparesis in 5–10% patients.[13] Diagnostic criteria are as follows.
Although delay in initiating treatment, poor compliance to medication, use of suboptimal dose, and inadequate combinations can lead to complications, it is often seen even well-compliant patients on ideal drugs face several complications. Hence, we decided to study the factors affecting the course of disease in seronegative patients.
PATIENTS AND METHODS
This was a prospective, cross-sectional, hospital-based study which included patients with probable TBM as per consensus criteria 2010 for the diagnosis of TBM. Patients admitted to neurology services at the National Institute of Mental Health and Neurosciences (NIMHANS) from February 2011 till December 2012 were included in the study. The study was performed after obtaining informed consent in patient's native language. Detailed clinical and neurological examination and various laboratory tests, including hematological, biochemical, lumbar puncture, neuroimaging computed tomography (CT) scan, and/or magnetic resonance imaging (MRI) scan. CD3 and CD4 count were also done in all cases. Seropositive patients were excluded from the study.
Observations
The results of the 43 patients with probable TBM as per consensus criteria 2010 evaluated at NIMHANS during the period of October 2011 to December 2012 were as follows [Table 1] age-wise distribution Figure 1.
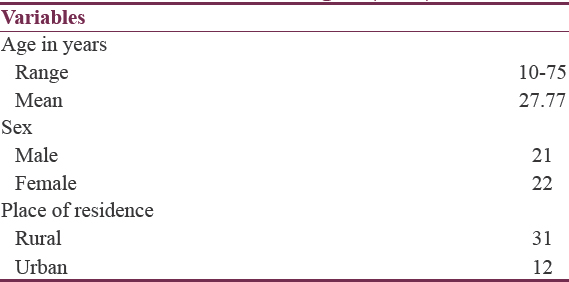
- Demonstrates age distribution of the study population
Demographic profile
Majority of the patient group 38 were from Hindu community (88.4%), and 5 patients were from Muslim community (11.6%).
Occupation
Five (11.6%) patients were farmers, 9 (20.9%) patients were manual laborer, 11 (22.9%) patients were students, 10 (20.8%) were house makers, and 8 (18.6%) patients were unemployed.
Neurological symptoms
The majority of our study group subjects presented with fever (100%), headache (100%), vomiting (55.8%), and altered sensorium (53.5%). Median duration for fever was 30 days with range from 10 to 180 days, for headache, it was 20 days with range from 1 to 179 days, and for altered duration, it was 5 days with a range of 1–29 days.
In addition to above symptoms, 6 (14%) patients had convulsions, and 3 (6.2%) had vision loss on presentation. Motor deficits in the form of hemiparesis 5 (11.6%) and paraparesis 3 (6.2%) was also noted during the presentation.
Constitutional symptoms in the form of malaise, loss of appetite, myalgia, and fatigue was present in 39 (90.7%) of patients. Past history of TB was present in 5 (11.6%) patients. Out of these 5 patients, 4 had pulmonary TB, and 1 patient had abdominal TB.
History of DM was present in 2 (4.7%) patients.
History of contact with a case TB in the family was present in 1 patient. History of chronic alcohol consumption and smoking was present in 8 (16.7%) patients, and oral tobacco intake was present in 10 (23.3%) patients.
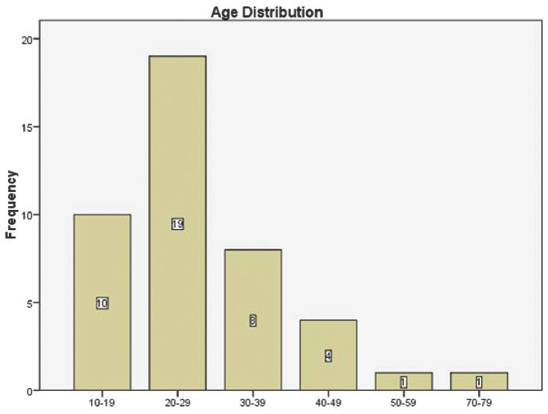
Neurological findings
On admission, 18 (41.9%) patients were febrile, pallor was present in 10 (23.3%) patients, clubbing and lymphadenopathy were present in 1 patient each.
Out of 43 patients, 20 patients were in altered sensorium on examination with 11 (25.6%) in drowsy state and 9 (20.9%) disoriented to time, place, and person.
Most of the patients had signs of meningeal irritation (97.7%) at the time of presentation. Hemiparesis was present in 5 patients (2.1%) and paraparesis in 3 patients (1.3%).
Cranial nerve involvement in the form of optic nerve involvement was present in 8 patients (18 6%), oculomotor in 6 patients (14%), trochlear in 4 patients (9.3%), and abducent nerve involvement in 9 patients (20.9%) [Table 2].
Investigations
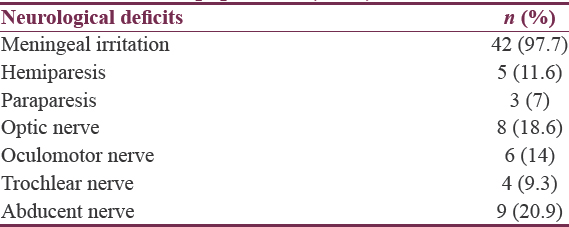
Hematological parameters
Hematological parameters in the patients revealed mean hemoglobin 12.45 ± 1.84 g%, mean erythrocyte sedimentation rate (ESR) was found to be on the higher side at 38.19 ± 0.45 mm/h [Table 3].
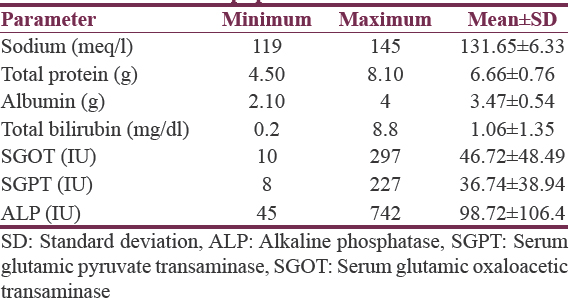
Biochemical parameters
The biochemical profile of study population revealed that mean serum sodium was 131.65 ± 6.33 meq/l, mean total protein of 6.66 ± 0.76 g, and mean total bilirubin of 1.06 ± 1.35 mg/dl [Table 4].
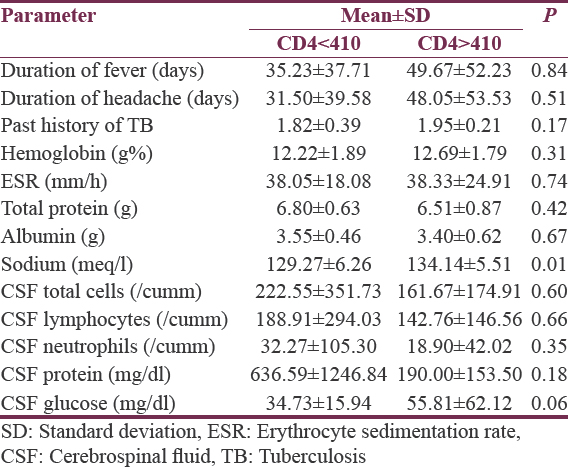
CD3 and CD4 count in patients
CD3 and CD4 were done for all patients, the normal values at our institute for CD3 ranges between 692 and 2540, CD4 count ranges between 410 and 1590, and normal CD4 percentage is 31–60%. Eighteen patients (41.9%) had abnormal CD3 count, 22 patients (51.2%) had abnormal CD4 count, and CD4 percentage was abnormal in 16 patients (37.2%). We compared the patients with low CD4 count to the patients with normal CD 4 count [Table 5].
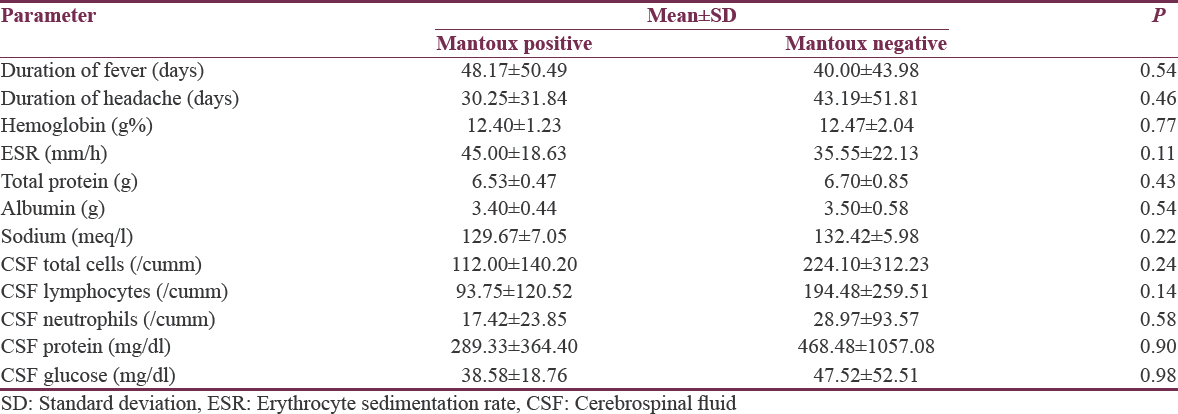
Mantoux test
The test was done in all patients, and it was read at 72 h after intradermal injection of purified protein derivative, more than 10 mm × 10 mm induration and redness was taken as positive, and it was found that 12 patients (27.9%) had positive result. We compared the patients with Mantoux positive versus Mantoux negative [Table 6].
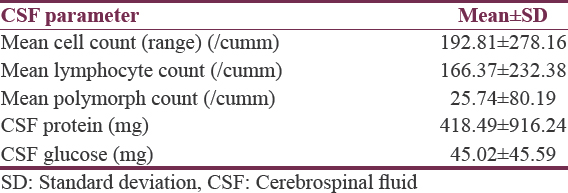
Cerebrospinal fluid analysis in study population
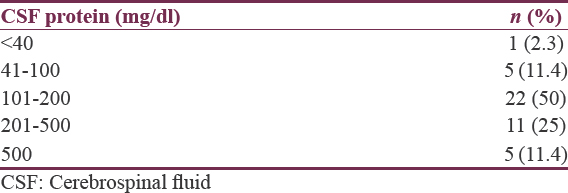
Following were the results of cerebrospinal fluid (CSF) parameters in the study population: Mean total cell count of 192.81 ± 278.16 was found with mean lymphocyte count of 166.37 ± 232.38 and mean neutrophil count of 25.74 ± 80.19. Mean CSF protein was 418.49 ± 916.27, and mean CSF glucose of 45.02 ± 45.59 [Tables 7–10]. The majority of the patients had CSF protein in between 100 and 200 mg, and five patients were culture positive.
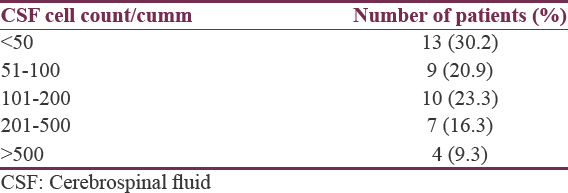
Cerebrospinal fluid cells in tuberculous meningitis patients
Enclosed in Table no. 5.
Cerebrospinal fluid proteins in study population
Enclosed in Table no. 5.
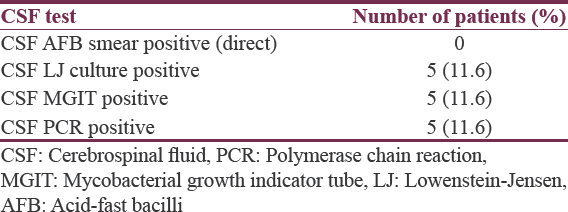
Evidence of tubercular bacilli in cerebrospinal fluid
All conventional culture positive cases were positive by mycobacterial growth indicator tube (MGIT) and polymerase chain reaction. Culture positive samples were subjected to testing of drug resistance testing by MGIT and HAIN MTB DR107+, and it was found 2 patients were sensitive for all first-line drugs, and the rest 3 patients were showing resistance pattern with 1 patient resistance to rifampicin and ethambutol and the other 2 patients showing resistance to isoniazid evidence of associated pulmonary involvement was found in 46.6% patients. Pulmonary involvement was found in 46.6% [Tables 11 and 12].

Neuroimaging
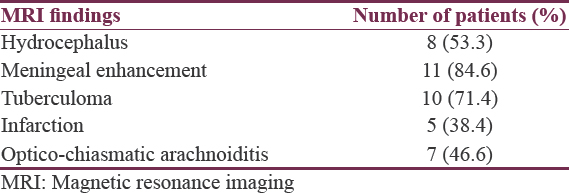
All patients underwent CT scan of the brain, and 15 patients underwent MRI brain in this study [Tables 13 and 14].
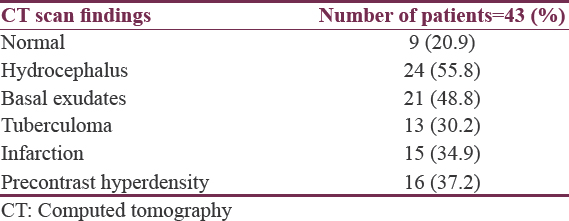
In this study, abnormal CT scan was found in 34 patients (79.1%), of which 24 patients were having hydrocephalus (55.8%), 21 had basal exudates (48.8%), 13 patients had tuberculoma (30.2%), 15 patients had evidence of infarction (34.9%), and 16 patients had precontrast hyperdensity (37.2%).
Magnetic resonance imaging brain findings
Cranial MRI was done in 15 patients who were having complicated CNS TB, 8 patients (53.3%) had hydrocephalus, 11 had meningeal enhancement (84.6%), 10 patients had tuberculoma (71.4%), 5 had evidence of infarction (38.4%), and 7 patients had evidence of opticochiasmatic arachnoiditis (46.6%) who had presented in addition with visual symptoms [Figures 2–5].
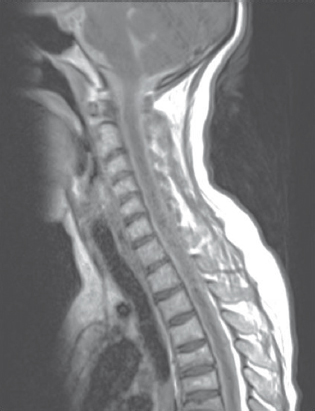
- Extensive spinal arachnoiditis in contrast sagittal images
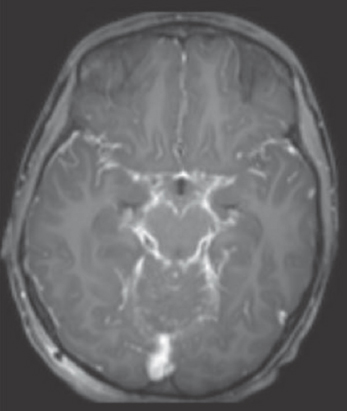
- T1 axial contrast images show extensive basal exudatesn
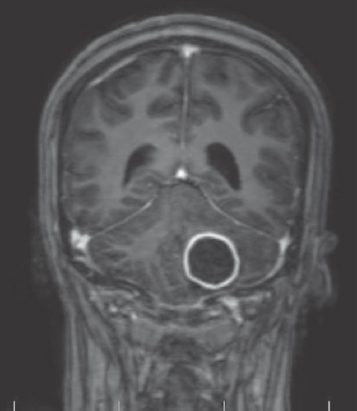
- Histopathology confirmed tuberculoma in T1 contrast images
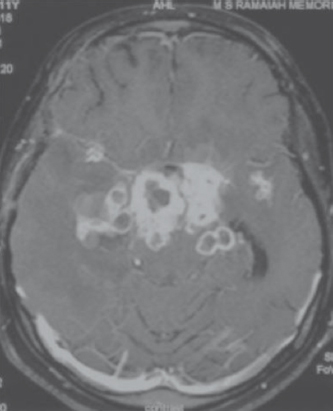
- T1 axial post contrast multiple tuberculomas in basal cisterns
RESULTS
Demographic profile of the patients
Females are slightly more than males with CNS TB and reverse with pulmonary involvement in this study and results in literature are variable.[1415] The majority were from rural areas. 22.9% were students, and 20.8% were homemakers and 11.6% farmers and 20.9% manual laborers indicating near equidistribution among all groups of people and young adults most affected. Fever, headache, and altered sensorium were the most common presenting symptoms.[1416] Visual impairment was seen in 18.6%. Literature reports available are from 27% to 32%.[1517] Motor disability in our patients is similar to what is reported in literature.[14] Constitutional symptoms in the form of malaise, loss of appetite, myalgia, fatigue were present in 39 (90.7%) of patients. History of TB was present in 5 (11.6%) patients which is in accordance with the previous studies. Of these patients, 4 had pulmonary TB, and 1 patient had abdominal TB. Raised ESR and positive Mantoux test are common. Hypoalbuminemia and hypoproteinemia were found in44.2% and 27.9%, respectively suggesting a possible role of malnutrition. Body mass index (BMI) of patients revealed <15 in 3 (7%) patients, 15–16 in 3 (7%) patients, 16–18.5 in 23 (53.5%), 18.5–25 in 13 (30.2%) patients, and more than 25 in 1 patient which again indicate increase risk of TB in underweight individuals. Serum sodium was found to be below 135 in 24 (55.8%) patients. Median CD3 count was 854, median CD4 count was 385, and median CD4 percentage was 33. It was found that 24 (55.8%) patients were having CD3 count which was less than the lowest limit of normal range, 21 (48.8%) patients were having CD4 count below the lowest limit of normal range, and 16 (37.2%) patients were having CD4 percentage below the lower limit of normal and these patients had a shorter prodrome and more incidences of hyponatremia. CSF parameters were comparable to other studies in literature. One of the patients who showed resistance to isoniazid expired and possibly predicts poor prognosis.
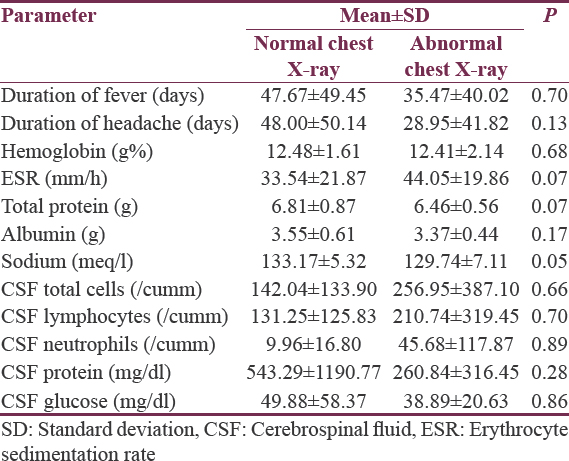
Imaging features
ESR was higher, and hyponatremia was more common in those with chest X-ray changes, and it parallels with inappropriate antidiuretic hormone secretion in patients with lung disease. Patients who had complications such as infarcts, hydrocephalus had more morbidity. Only 8 patients had taken BCG vaccine and probably had a role complicated TB in unvaccinated patients.
Outcome
Out of 43 patients, 3 patients passed away, of which 1 patient had evidence of resistance to isoniazid and 2 several weeks delay in initiating treatment and were showing features of sepsis at admission. 26 patients recovered well, 14 patients left with cognitive, motor, and visual morbidity.
DISCUSSION
TBM in this study seems to be common in young adults of rural background. The possibility of referral bias to our institution cannot be excluded. Vague symptoms are often the presenting symptoms, therefore, high degree of suspicion is needed and when in doubt should be investigated. ESR more than 50 mm was found in 12 patients which collaborates with information in literature.[14] The role of nutritional deficiency is suggested by low proteins in patients and low BMI. Hyponatremia seems to be a common complication associated with altered sensorium.
The common reasons reported for vision involvement in TBM are optic nerve involvement, optico-chiasmatic arachnoiditis, and third ventricular compression of optic chiasm, optic nerve granuloma, and ethambutol toxicity. The 2nd, 3rd, 4th, and 6th cranial nerves were the cranial nerves involved in our study in that order of preference. We found 7 out of 8 people visual symptoms having optico-chiasmatic arachnoiditis by MRI. Diabetes, family contact with TB and alcohol did not contribute to the cases in a major way. Some studies report 6th nerve as most commonly involved.[18] Culture positive cases were only 16%; however, they were smear negative, and both conventional techniques and newer methods showed same degree of sensitivity in detecting culture positivity. Of the cultural positive cases, 60% were resistant one drug or other and possibly predicts poor prognosis. The Mantoux test was positive in 12 (27.9%) which is in concordance with literature.[19] Those positive cases in this study mean duration of fever and ESR values were higher in patients who had positive Mantoux test compared to negative cases. Some studies have reported negative test in patients with TBM.[20] The role of nutritional deficiency is suggested by low proteins in patients.[21] Low BMI and albumin lead to low immunity, and hence, higher chances of acquiring TB. As CD3 and CD4 are required for T cell activation, it can be inferred that decrease in in these cell count can predispose to the development of TBM even in seronegative people.[22] Excessive secretion of atrial natriuretic peptide and brain natriuretic peptide, and a direct neural influence on renal function is involved in the pathogenesis of hyponatremia. The cerebral salt wasting syndrome should be treated with volume and salt replacement. Fludrocortisone may be beneficial. Hyponatremia also can be caused by adrenal failure in cases with adrenal involvement with TB. Patients having pulmonary TB are more prone for metabolic complications, and therefore, it is a poor prognostic marker. Cisternal lesions, hydrocephalus, and infarcts leave more morbidity.
CONCLUSION
This prospective study reveals very poor BCG immunization status in those patients who presented to us with TBM. Patients were from all classes of people and were young adults from rural background. They had low BMI, hypoproteinemia, low CD4 and CD3 counts inspite of being seronegative. Direct Arachnoiditis at optic chiasm is the most common cause of blindness in this series of patients. Pulmonary involvement is common, and those with low CD4, CD3 counts, and pulmonary involvement have more incidence of hyponatremia and hence more morbidity. Conventional tests are as sensitive as modern tests in detecting culture positive cases. Drug resistance is common in culture-positive patients. Late initiation of treatment and drug resistance contribute to mortality.
Suggestions
BCG vaccination status should improve in the community in addition to nutritional factors. High degree of suspicion and investigations will lead to early diagnosis in patients who show vague symptomatology. There is high prevalence of seronegative patients with low CD4 and CD3 who have more risk of disease and its morbidity. Nutritional status of rural adults needs to be addressed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Global Tuberculosis Report 2013. Geneva, Switzerland: World Health Organization; 2013.
- Improving tuberculosis control through public-private collaboration in India: Literature review. BMJ. 2006;332:574-8.
- [Google Scholar]
- Miliary tuberculosis: New insights into an old disease. Lancet Infect Dis. 2005;5:415-30.
- [Google Scholar]
- Linico-radiological spectrum of tuberculosis among HIV sero-positives – A Tambaram study. Cough. 2001;1367:85-43.
- [Google Scholar]
- Tuberculosis as a complex trait: Impact of genetic epidemiological study design. Mamm Genome. 2011;22:91-9.
- [Google Scholar]
- Mycobacterium fortuitum-chelonae complex infection in a child with complete interleukin-12 receptor beta 1 deficiency. Pediatr Infect Dis J. 2001;20:551-3.
- [Google Scholar]
- A polymorphism in human TLR2 is associated with increased susceptibility to tuberculous meningitis. Genes Immun. 2007;8:422-8.
- [Google Scholar]
- The pathogenesis of tuberculosis meningitis 1933
- IFNgamma response to Mycobacterium tuberculosis, risk of infection and disease in household contacts of tuberculosis patients in Colombia. PLoS One. 2009;4:e8257.
- [Google Scholar]
- Pathology and pathogenetic mechanisms in neurotuberculosis. Radiol Clin North Am. 1995;33:733-52.
- [Google Scholar]
- Tuberculous meningitis in adults: An eleven-year review. Int J Tuberc Lung Dis. 1998;2:553-7.
- [Google Scholar]
- Tuberculous meningitis: Many questions, too few answers. Lancet Neurol. 2005;4:160-70.
- [Google Scholar]
- Tuberculous meningitis in adults: A review of 160 cases. ScientificWorldJournal. 2012;2012:169028.
- [Google Scholar]
- Tuberculous meningitis in adults: Review of 48 cases. Clin Infect Dis. 1996;22:982-8.
- [Google Scholar]
- Tuberculosis among health care workers in a short working period. Am J Infect Control. 2005;33:23-6.
- [Google Scholar]
- Paradoxical vision loss associated with optochiasmatic tuberculoma in tuberculous meningitis: A report of 8 patients. J Infect. 2010;60:458-66.
- [Google Scholar]
- Molecular genetic analysis of nucleotide polymorphisms associated with ethambutol resistance in human isolates of Mycobacterium tuberculosis. Antimicrob Agents Chemother. 2000;44:326-36.
- [Google Scholar]
- Tuberculosis of the central nervous system in children: A 20-year survey. J Infect. 2000;41:61-8.
- [Google Scholar]
- Impact of immunosuppression on radiographic features of HIV related pulmonary tuberculosis among. Nigerians Turk Thorac J 2009:112-7.
- [Google Scholar]
- The influence of host and bacterial genotype on the development of disseminated disease with Mycobacterium tuberculosis. PLoS Pathog. 2008;4:e1000034.
- [Google Scholar]






