Translate this page into:
Extensive long-segment cervicothoracic traumatic spinal epidural hematoma with avulsion of C7, C8, and T1 nerve roots
Address for correspondence: Dr. Guru Dutta Satyarthee, Department of Neurosurgery, All India Institute of Medical Sciences, New Delhi, India. E-mail: duttaguru2002@yahoo.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Traumatic spinal epidural hematoma (TSEH) is of rare clinical occurrence. We report a case of a young man with posttraumatic long-segment spinal epidural hematoma. Evacuation of the hematoma led to complete neurologic recovery in our patient. Our case highlights the importance of early diagnosis and prompt surgical intervention for the evacuation of hematoma in preservation or maximum recovery of neurologic function. Imaging findings, management options, and the relevant literature are reviewed.
Keywords
Spinal extradural hematoma
surgical decompression
trauma
Introduction
Spinal epidural hematomas (EDHs) are rare and posttraumatic spinal EDHs are even rarer. The rarity of these lesions does not decrease their importance, as they are a disabling but treatable cause of compressive myelopathy. Timely surgical intervention results in good outcome. Most described cases of spinal EDH are spontaneous, which may develop from bleeding from arteriovenous malformations, coagulation disorders, thrombolysis, or a coronary event.[1] Traumatic extradural hematomas, although commonly seen in the cranium, are relatively rare in the spine, with only a few case reports of traumatic spinal epidural hematoma (TSEH) reported in the literature.[234] Causes of TSEH may include fracture, dislocation, lumbar puncture, birth trauma, or missile injury. We report a patient with a long-segment TSEH secondary to trauma who had good neurologic recovery after surgical evacuation.
Case Report
A 33-year-old man presented to our hospital with weakness of right upper and lower limb and left lower limb, 3 days after a motor vehicle accident. He was conscious and oriented, with a Glasgow Coma Score of E4V5M6. Neurologic examination revealed hypertonia in both the lower limbs and flaccid right upper limb. Motor power was 0/5 (Medical Research Council grading) in the right upper limb and 2/5 in both the lower limbs. Power in the left upper limb was normal (5/5). Deep tendon reflexes were exaggerated in both the lower limbs and were lost in the right upper limb. There was complete loss of all sensations (pain, touch, temperature, and position sense) in the right upper limb. He had fracture of multiple ribs with bilateral hemopneumothorax along with fracture of right clavicle and scapula. Routine hematologic investigations, including coagulation profile, were within normal limits.
A non-contrast computed tomography (NCCT) of cervical spine revealed C4-C5 block vertebrae without any fracture or dislocation [Figure 1], and NCCT of head did not reveal any abnormality.

- Non-contrast computed tomography cervical spine showing C4-C5 block vertebrae without any fracture or dislocation
Magnetic resonance imaging (MRI) of the brachial plexus revealed avulsion of right C7, C8, and T1 nerve roots with a pseudomeningocele formation. MRI of the cervical spine revealed cord contusion at C6–C7 level with spinal epidural hematoma with compression of spinal cord extending from C3 to T2 level [Figures 2 and 3]. In view of maximum compression at the cervical level, C4–C7 laminoplasty and evacuation of hematoma was done. Approximately 40 mL of altered blood was evacuated from the spinal epidural space. The patient showed a remarkable recovery with improvement in power in both the lower limbs in the postoperative period. At the time of discharge from hospital, 10 days after surgery, he had a power of 4/5 in both the lower limbs. However, power in the right upper limb remained unaltered.

- Sagittal section magnetic resonance imaging showing collection anterior to the cord compressing the cord and cord contusion at C6-C7
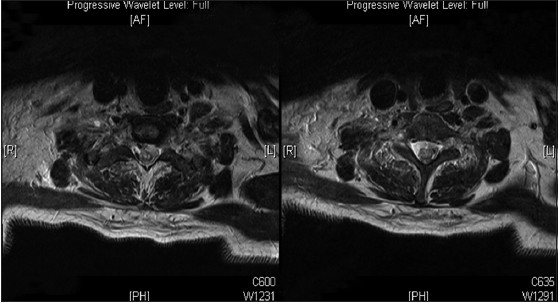
- Axial section magnetic resonance imaging showing hyperintense collection on T2 anterior to the cord and causing cord compression
At 3 months follow up, the patient had a power of 5/5 in both the lower limbs, although he had persistent weakness in the right upper limb. Electromyography and nerve conduction studies at the same time (3 months after surgery) revealed preganglionic type of brachial plexus injury in the right upper limb.
Discussion
Posttraumatic spinal epidural hematomas are rare, with the reported incidence being less than 1% of all spinal injuries.[3] Spontaneous spinal epidural hematoma may be caused by rupture of arteriovenous malformations, thrombolytic therapy following coronary ischemic events, or hemophilia coagulation disorders.[1] Causes of TSEHs include vertebral fractures, obstetrical birth trauma, lumbar punctures, postsurgical bleeding, epidural anesthesia, and missile injuries.[5] Cervical spondylosis, rheumatoid arthritis, Paget's disease, and ankylosing spondylitis have been implicated as risk factors for posttraumatic spinal epidural hematoma.
Foo and Rossier studied 38 patients of TSEH and divided them into two groups: Those associated with vertebral fracture and those without fracture. Overall, cervical region (36.8%) was the most commonly affected region, followed by cervicothoracic (23.7%) and thoracic (18.4%), in this sequence.[6] Narayan et al. have reported two cases of TSEH. In one patient, the hematoma was in thoracic region and in the second patient, it was in the cervicothoracic region. Mechanical compression due to hematoma was anterior to the cord in the first patient and posterior to the cord in the second patient.[2]
TSEHs are probably venous in origin.[27] The rich epidural venous plexus, being thin walled and valveless, is prone to bleeding following sudden brief increase in intravenous pressure.[8] The same is the most probable cause of bleed in our patient.
Symptomatology of TSEHs vary from clinically silent to life threatening, with the rate of life risk reported to be as high as 23% in one study.[5] Common presenting features of TSEHs include neck pain/backache, weakness, and respiratory difficulty.
MRI remains the best investigation for early detection of spinal EDH. Chang et al.[9] studied 20 patients with TSEH and reported that most hematomas were homogeneously isointense on T1-weighted images and homogeneously hyperintense on T2-weighted images relative to the spinal cord, when examined within 36 h of traumatic event. However, beyond 36 h of their onset they appear as heterogeneously isointense or hyperintense lesion on T1-weighted images, and as mixed high- and low-signal change on T2-weighted images.[9]
Contrary to cranial EDHs, osseous injury rarely coexists with spinal EDHs, with a reported incidence of as low as 0.5%-7.5%.[5] This has clinical implication, with better recovery rates reported after surgical intervention in patients with TSEHs without spinal fracture according to Foo and Rossier[6] Spinal EDHs rarely surround the spinal cord, they rather compress it from one side. According to Groen and Ponssen, most of sudden spinal EDH tends to occur in posterior epidural space.[10]
Computed tomography scan of our patient showed fracture of both transverse processes of C5, C6, and C7. MRI study of brachial plexus of the current case showed avulsion of C7, C8, and T1 nerve roots on the right side and associated edema of paraspinal muscles.
TSEHs are considered neurosurgical emergencies because progressive cord compression may result in permanent deficits. Management depends on the clinical condition of the patient and the degree of cord compression.[3811] Conservative management has been advocated especially when the patient's neurologic status is stable or improving. Proponents of conservative management proposed that TSEHs in a number of patients might resolve spontaneously, with the patient making a complete neurologic recovery. Few such cases have been reported.[31213]
Emergency surgical evacuation in the presence of significant cord compression gives the best chance for a good functional outcome.[14] Our case was managed with a laminoplasty and evacuation of the epidural hematoma. Rohde et al. observed better prognosis in TSEH compared with spontaneous spinal EDH. They ascribed their findings to the earlier medical surveillance with early pick up in posttraumatic cases, smaller size of the hematoma, and early management.[15] The assessment of coagulation parameters is also important before planning evacuation of the hematoma, as coagulopathy is an important cause of epidural hematoma.
The level of preoperative neurologic deficit, severity of the neurologic deficit, and time to operative intervention are the most critical factors affecting recovery. It is very important to be vigilant for the possibility of development of TSEH, especially in patients who develop signs and symptoms of compressive myelopathy following motor vehicle accident. Urgent MRI scan should be carried out to look for TSEH and further timely neurosurgical intervention is important in order to achieve recovery of the neurologic function.
Our patient had cervicothoracic TSEH and especially it was a very long segment. Our case was unique in the way that there was associated brachial plexus involvement as well, which is a very rare associated finding.
Conclusion
TSEHs are rare compared with cranial EDH and spontaneous spinal EDH. They are usually venous in origin and may not be associated with any osseous injury. The need for immediate neurosurgical intervention has been stressed in the literature; however, a few authors have reported good recovery with conservative management as well. Hence, the key to good neurologic outcome is high index of suspicion, early imaging studies (MRI) to make a diagnosis, and timely intervention, which needs to individualized based on the severity of symptoms.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Spontaneous spinal epidural hematoma: Analysis of 23 cases. Surg Neurol. 2008;69:253-60.
- [Google Scholar]
- Two children with traumatic thoracic spinal epidural hematoma. J Clin Neurosci. 2009;16:1356-8.
- [Google Scholar]
- Delayed traumatic spinal epidural hematoma with spontaneous resolution of symptoms. J Emerg Med. 2004;27:37-41.
- [Google Scholar]
- Delayed traumatic thoracic spinal epidural hematoma: A case report and literature review. Am J Emerg Med. 2007;25:69-71.
- [Google Scholar]
- Spinal extraepidural haematoma. In: Vinken P J, Bruyn G W, eds. Handbook of Clinical Neurology. Injuries of the Spine and Spinal Cord, Part 11. Vol Vol. 26. Amsterdam: North-Holland; 1976. p. :1-30.
- [Google Scholar]
- Traumatic spinal epidural hematoma of a 10-month-old male: A clinical note. Pediatr Neurol. 2000;23:88-9.
- [Google Scholar]
- Traumatic epidural hematoma of the cervical spine: Diagnosis with magnetic resonance imaging. Case report. J Neurosurg. 1988;68:798-801.
- [Google Scholar]
- Evaluation of clinical and MR findings for the prognosis of spinal epidural haematomas. Clin Radiol. 2005;60:762-70.
- [Google Scholar]
- The spontaneous spinal epidural hematoma. A study of the etiology. J Neurol Sci. 1990;98:121-38.
- [Google Scholar]
- Cervical epidural hematoma in children: A rare clinical entity. Case report and review of the literature. Neurosurg Focus. 2006;20:E6.
- [Google Scholar]
- Spontaneous resolution of symptomatic post-traumatic cervical epidural hematoma. A case report. J Bone Joint Surg Am. 2001;83-A:255-8.
- [Google Scholar]
- Resolution of spontaneous spinal epidural hematoma without surgery: Report of two cases. Spine (Phila Pa 1976). 2001;26:E525-7.
- [Google Scholar]
- Non-operative treatment of spontaneous spinal epidural hematomas: A review of the literature and a comparison with operative cases. Acta Neurochir (Wien). 2004;146:103-10.
- [Google Scholar]
- Microsurgical treatment of spontaneous and non-spontaneous spinal epidural haematomas: Neurological outcome in relation to aetiology. Acta Neurochir (Wien). 2000;142:787-93.
- [Google Scholar]






