Translate this page into:
Abducens nerve avulsion sustained by traumatic brain injury: A lesion not to be underestimated
*Corresponding author: Rayan Fawaz, Department of Neurosurgery, Percy Military Teaching Hospital, Clamart, France. ryfawaz@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Fawaz R, Hedjoudje M, Law-Ye B. Abducens nerve avulsion sustained by traumatic brain injury: A lesion not to be underestimated. J Neurosci Rural Pract 2023;14:591-2.
Traumatic brain injury (TBI) is a major cause of morbidity and mortality. Indeed, TBI is associated with an increased risk of poor health and neurodegenerative disease and an increased need for personal care.[1] Moreover, the incidence of unilateral abducens nerve palsy (ANP) following TBI has been reported to be 1–2.7%, and ANP is mostly associated with severe TBI and/or cervical spine fracture.[2] However, ANP after TBI without a skull base fracture has not been recently documented, and its diagnosis might be challenging.
Herein, we report the case of a 70-year-old patient admitted after a mild TBI. The initial computed tomography scan revealed a subarachnoid hemorrhage in the left temporal hemisphere and pontocerebellar cistern without a skull fracture [Figure 1]. The patient presented with cephalalgia and right ANP demonstrated on a Hess chart. We performed high-resolution T2-weighted magnetic resonance imaging (MRI), which revealed blunt avulsion of the right abducens nerve at its emergence from the brainstem [Figure 2].
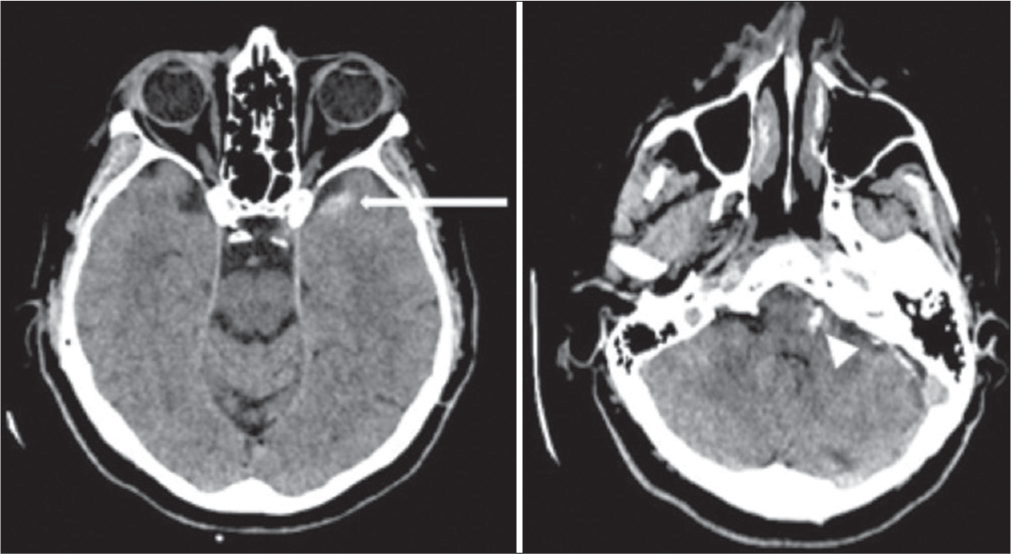
- Axial computed tomography scans showing a subarachnoid hemorrhage in the left temporal region (white arrow) and in the left pontocerebellar cistern (white head of arrow).

- High-resolution three-dimensional T2-weighted magnetic resonance imaging sequence in sagittal views centered on the left (a) and right, (b) abducens nerves, and reconstruction in the plane of the nerves (c) showing a section of the right abducens nerve (white arrows). The left abducens nerve was intact and normally continuous (white head of arrow).
The abducens nerves, arising from the nucleus beneath the fourth ventricle’s facial colliculus, emerge as a single trunk from the brain stem at the bulbopontine sulcus and become extradural at the dorsum sellae through a rigid hole. Between the emergence point and the exit point into the extradural space, the nerve lies on the petrous bone’s apex.
During TBI, the petrous bone is subject to physical constraints that may lead to contusions and lacerations of the abducens nerve, causing its avulsion.[2]
In a prospective multicenter study on ANP after TBI, the overall spontaneous recovery at 6 months post-injury was 73%, with a higher rate for unilateral palsy.[3] Moreover, functional prognosis was associated with the inability to abduct past midline at presentation.[3]
Considering the increasing incidence of head and neck injuries and the underestimated rate of abducens avulsion, many cases possibly remain undiagnosed, along with other cranial nerve injuries (such as oculomotor injury).[4] Therefore, practitioners should be particularly vigilant in the presence of ANP by performing high-resolution three-dimensional T2-weighted MRI on the posterior fossa to diagnose abducens avulsion promptly and initiate rehabilitation as soon as possible.
Ethics approval
The patient has approved the publication of the article.
Authors’ contributions
RF, MH, and BL designed the study. RF and MH performed the methodology and literature review. MH collected the patient’s data. RF, MH, and BL participated in the drafting of the manuscript. RF critically revised the manuscript. RF, MH, and BL performed the final revision of the manuscript.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- The longitudinal effects of comorbid health burden on functional outcomes for adults with moderate to severe traumatic brain injury. J Head Trauma Rehabil. 2020;35:E372-81.
- [CrossRef] [PubMed] [Google Scholar]
- Post-traumatic unilateral avulsion of the abducens nerve with damage to cranial nerves VII and VIII: Case report. NMC Case Rep J. 2016;3:81-3.
- [CrossRef] [PubMed] [Google Scholar]
- Predictors of nonrecovery in acute traumatic sixth nerve palsy and paresis. Ophthalmology. 2001;108:1457-60.
- [CrossRef] [PubMed] [Google Scholar]
- Traumatic oculomotor nerve section. J Fr Ophtalmol. 2016;39:880-1.
- [CrossRef] [PubMed] [Google Scholar]






