Translate this page into:
Ethylene glycol toxic encephalopathy
Address for correspondence: Dr. Luciano Santana-Cabrera, Avenida Marítima del Sur s/n. Las Palmas de Gran Canaria, Canary Islands - 35016, Spain. E-mail: lsancabx@gobiernodecanarias.org
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
The neurological clinic is the most frequent and early to appear in the Ethylene Glycol (EG) intoxication. It is characterized by inebriation symptoms very early (from 30 minutes till 12 hours), from lethargy to coma. Seizures can occur and even status epilepticus. Other neurological signs are papiledema, ophtalmoplegia, nystagmus, ataxia, and tetany. In patients who died at this stage are described cerebral swelling, brain hemorrhage, aseptic meningitis, and encephalitis, and crystal formation in central neurological system (CNS).[1] The diagnosis is based on the suspicion of ingestion, the presence of visual disorders, high anion gap metabolic acidosis and an osmolar gap, and elevated levels of creatine kinase (CK). The confirmation is provided by the determination of plasma levels or in gastric juice of EG.
We present a case of a 53-year-old man, found by his neighbors at home, with low level of consciousness. He was transferred to the Emergency Department who arrived in coma (GCS 3-4) and hypotensive. Laboratory studies reveled a severe metabolic acidosis (pH of 6.96, pCO2 of 36 mm Hg, HCO3 of 8.1 mmol/L with a base deficit of -23’5), plasma osmolarity of 333 mOsm/L, anion gap of 46 mmol/L, lactate of 9.92 mmol/L, creatinine of 9.37 mg/dl, urea of 258 mg/dl, CK of 5940 U/L, thrombocytopenia of 73.000/μL, and leukocytosis of 13.600/μL. Urine analysis of drugs and blood alcohol was negative. A computed tomography (CT) scan was performed at admission, without pathological findings. For the clinical situation of unknown cause of coma, analytical data of severe high anion gap metabolic acidosis, anuric renal failure and rhabdomyolysis, methanol or EG poisoning was suspected; so, ethanol and dialysis treatment was started. We provide 10% ethanol bolus of 1 g/kg/iv for 30’ and then an infusion of 1.5 ml/kg/h for serum levels of 150 mg dl. The metabolic problem was resolved, but the renal failure persisted requiring dialysis, and also the coma status with a maximum GCS of 9 (4-1-4). The determination of toxics was held in a blood sample by gas chromatography technique attached to mass spectrometry (GC/MS), confirming the presence of EG. Estimated concentration EG was 285 mg/dl.
Six days after admission, a new CT scan was performed, and it showed multiple areas of hypodensity at the basal ganglia (head of caudate nucleus) and in bordering territories [Figure 1]. After a month, the patient didn’t suffer neurological changes, remained comatose.
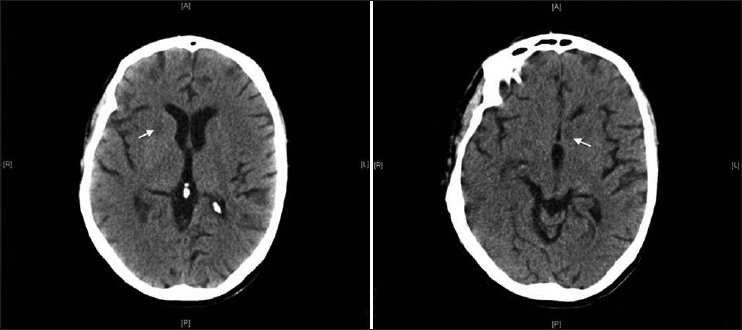
- Cerebral computed tomography show multiple areas of hypodensity at the basal ganglia
The 80% of the EG absorbed is metabolized mainly in the liver by the enzyme, alcohol dehydrogenase, and the rest is excreted unchanged by kidneys, such as calcium oxalate. The EG metabolites are glycoaldehyde, glycolic acid, glyoxylic acid, oxalic acid, and calcium oxalate. The blocking of conversion of glycolic acid to glyoxylic will induce a metabolic acidosis by the high ratio NADH/NAD.[2]
Ethanol is a competitive substrate for alcohol dehydrogenase, which has greater affinity for ethanol than for ethylene glycol. Therefore, ethanol is effective and inhibits the metabolism of ethylene glycol. Although it is difficult to dose and has sedative and behavioral effects, ethanol is inexpensive and easily obtained. An alternative is fomepizole (4-methylpyrazole). It is also a competitive inhibitor of alcohol dehydrogenase and prevents the formation of toxic acid metabolites. It is easy to dose, easy to administer, and side-effects are rare. However, it is expensive and not available in all hospitals. Hemodialysis is used to clear both EG and its toxic metabolites more quickly.
It is a characteristic finding on the CT scan, or in the postmortem examination, the presence of necrosis in areas of the optic nerve and in some areas of the cerebral white matter, which typically affects the caudate and putamen nuclei, as it was observed in our patient. The putaminal lesion seems to be a selective toxic effect and can be associated with more extensive neuronal damage of cerebral cortex and other gray nuclei, being uncommon lesions of the white matter. The lesions are correlated with the clinical findings and are similar to those observed in trichloroethane poisoning, carbon monoxide, hypoxia-anoxia, Wilson's disease, Leigh disease, Kearns-sayre syndrome, and Leber's optic atrophy striatal degeneration.[345]
References
- Ethylene glycol poisoning: Toxicokinetic and analytical factors affecting laboratory diagnosis. Clin Chem. 1998;44:168-77.
- [Google Scholar]
- CT and MR imaging findings in methanol intoxication. AJNR Am J Neuroradiol. 2006;27:452-4.
- [Google Scholar]
- Putaminal necrosis after methanol intoxication. J Neurol Neurosurg Psychiatry. 1992;55:234-5.
- [Google Scholar]





