Translate this page into:
Epidural and paraspinal varices seen in inferior vena cava agenesis causing lumbar radiculopathy
*Corresponding author: Krishnan Nagarajan, Department of Radio-Diagnosis, Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry, India. lknagarajan1@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Nagarajan K, Amuthabharathi M, Sathiaprabhu A. Epidural and paraspinal varices seen in inferior vena cava agenesis causing lumbar radiculopathy. J Neurosci Rural Pract 2023;14:184-6.
Dear Editor,
Spinal epidural venous dilatation causing nerve root compression is uncommon. Spinal venous anatomy is relatively understudied with many classification schemes. Recent case reports with review of the literature showed the paucity of understanding the etiology of these cases and underlying venous anatomy. Wong et al.[1] referred to 20 cases of epidural venous engorgement causing radicular symptoms and found five patients with cauda equina syndrome. Another review of 55 patients in 25 reports by Hassan et al.[2] included post-operative patients of spinal fusion developing adjacent segment disease. They found that three had inferior vena cava (IVC) thrombosis, one IVC agenesis, and another seven with iliac venous thrombosis including a case of Leiden factor V deficiency.
A 30-year-old man presented with the complaints of low backache with radiating pain to the right lower limb for 2 months. There was no history of trauma or fever. Clinical examination did not reveal any sensory or motor deficit. The patient was referred for magnetic resonance imaging (MRI) lumbosacral spine for the evaluation of low backache. MRI showed epidural and paravertebral multiple serpiginous flow voids (dilated vessels) along the neural foramina of the thoracolumbar region [Figure 1]. Flow voids were seen in foraminal and adjacent paraspinal regions extending from the T10 level to inferiorly extending to the level of S2. No intradural or perimedullary (conus) flow voids were noted. No obvious cord signal changes or edema noted. Broad-based disk protrusions were noted at L4-L5 and L5-S1 levels causing mild anterior thecal sac indentation. Contrast CT showed absent inferior vena cava in the abdomen, replaced by multiple dilated tortuous collaterals of paravertebral venous plexus, ascending lumbar veins in the para-aortic region [Figure 2]. The collaterals were seen draining into the dilated azygos-hemiazygos venous system. Multiple epidural venous collaterals noted in the dorsolumbar region and sacral region. The common iliac vein was seen communicating with the paravertebral venous collaterals. The left renal vein appears prominent, both renal veins communicating with the collaterals. Few collaterals were seen draining into the superior mesenteric vein. The dilated azygos vein was draining into the right atrium.
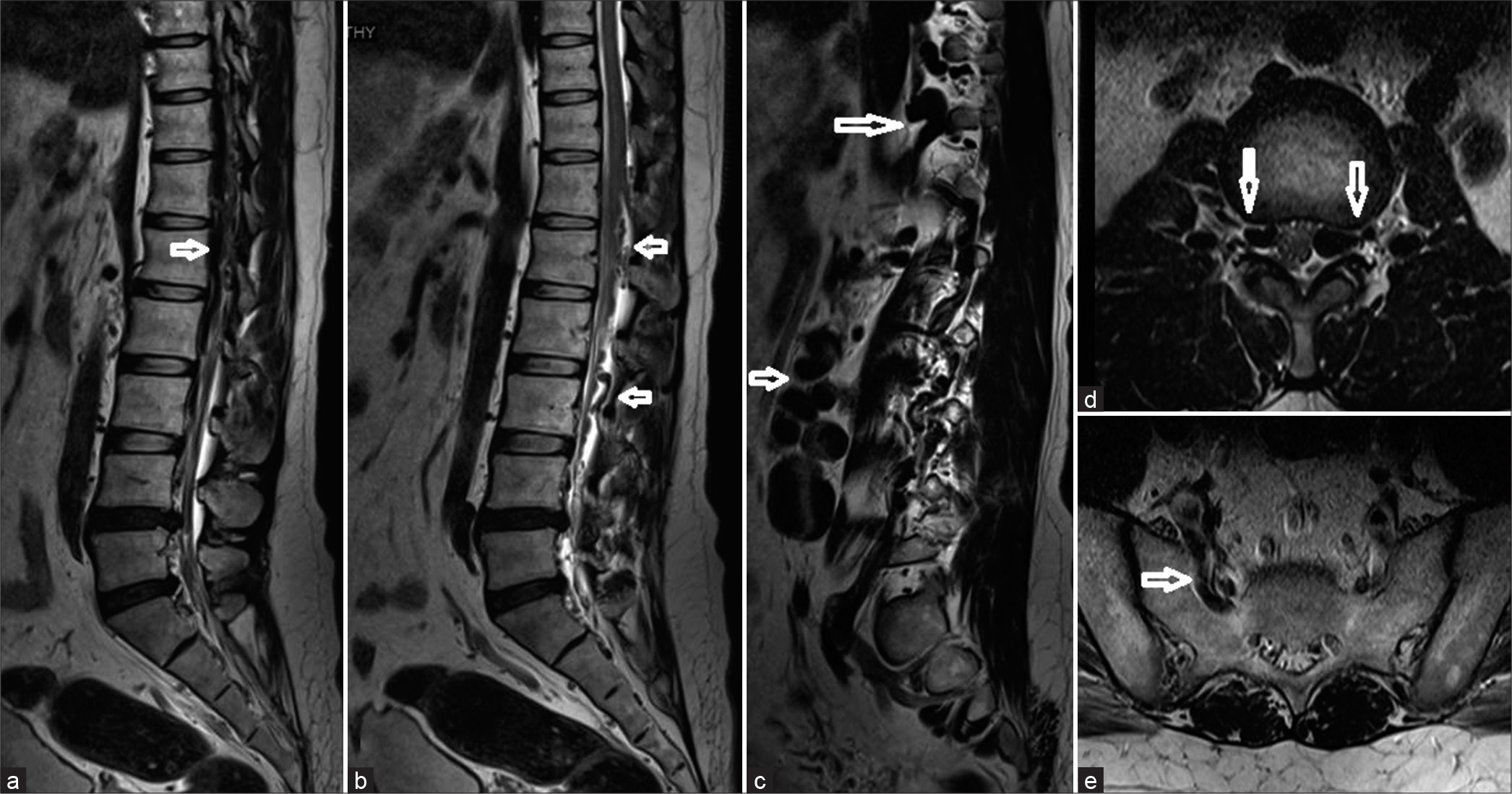
- Magnetic resonance imaging sagittal (a-c) and axial (d and e) sections showing multiple .(anterior and posterior) epidural and paraspinal varices (arrows in a to c)causing neural foraminal indentation (arrows in d) and also seen is the right lateral sacral vein (arrow in e).
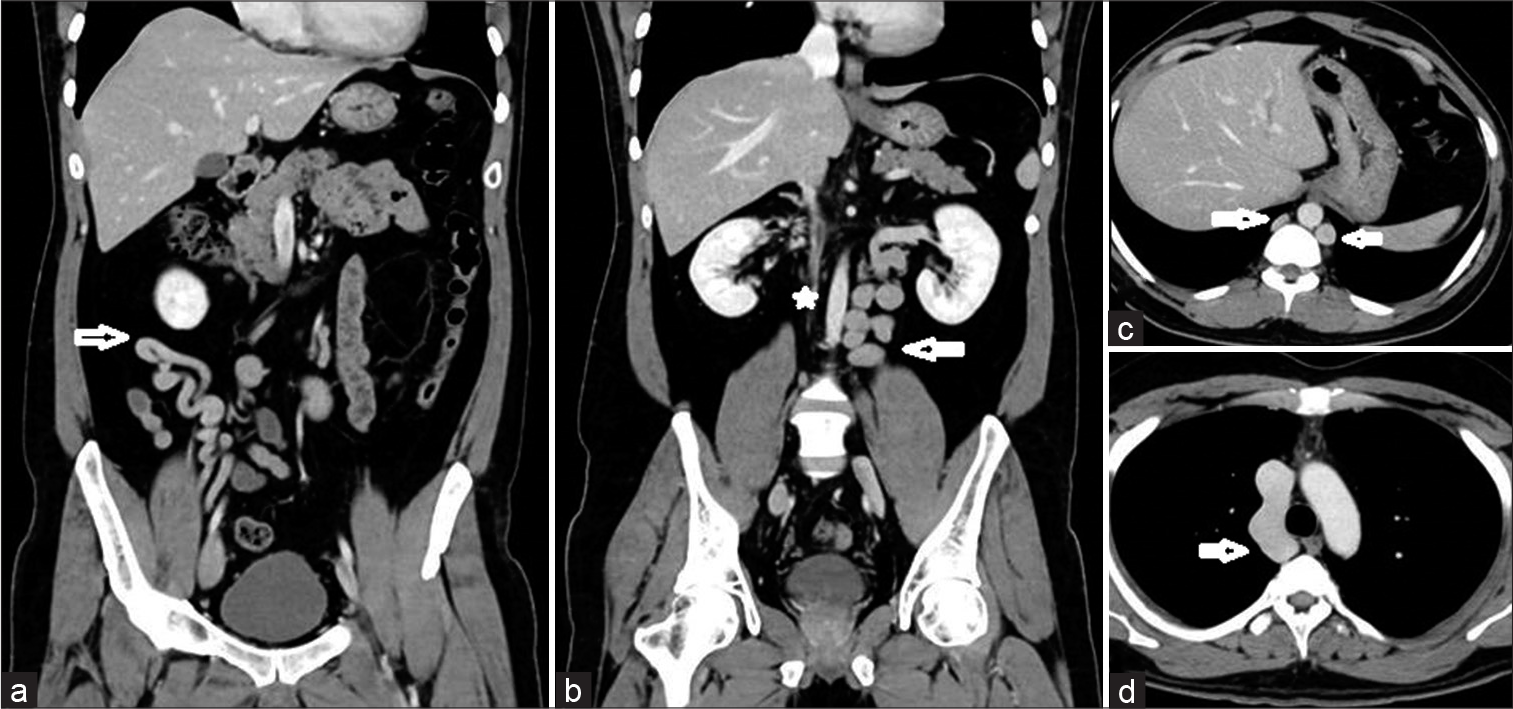
- Contrast CT coronal reformations (a and b) and axial sections (c and d) showing mesenteric (arrow in a), ilio-lumbar and reno-lumbar collaterals (arrow in b). IVC is not seen in its normal location (* in b). Prominent azygos and hemiazygos (arrows in c) are noted which join and drain into the superior venecava (arrow in d).
Zimmerman et al.[3] reported one of the earliest descriptions of epidural venous channels causing lumbar radiculopathy. Similar to few isolated reports before them, they thought the disk herniation predisposes to epidural varix formation and accentuates radicular symptoms. In fact, disk herniation was diagnosed based on epidural venographic findings of compression or occlusion of anterior internal vertebral veins or the radicular veins apart from other findings of collateral flow and focal venous dilatation. Hanley et al.[4] classified epidural venous structures causing radicular symptoms into three types – thrombosed vein, dilated nonthrombosed vein, and epidural hematoma and considered trauma or disk herniation as the cause of epidural venous changes. Subsequent reports have shown that epidural varix formation can occur without any disk bulge or herniation and in particular, varices in those with thrombosis or non-development of IVC presenting with radiculopathy. However, the osteophyte-disk indentation or related fibrosis may perhaps still have a role in those without IVC thrombosis or agenesis.[5]
Inferior vena cava obstruction has been shown to recruit three types of collateral pathways – vertebrolumbar, anterior abdominal wall, and portocaval (transumbilical) – with vertebro-lumbar being the predominant type.[6] The external vertebral plexus forms the vertebro-lumbar collateral pathway of ascending lumbar, lateral sacral, intersegmental, and other paraspinal veins to reach the azygos-hemiazygos system bypassing the IVC.[3,7] IVC agenesis itself is being thought of a sequel to neonatal thrombotic process of usually the infrarenal IVC but which if extends above the level of renal veins, can be associated with iliolumbar and renolumbar collaterals through the hemiazygos-azygos system similar to our case.[8] Similar cervical epidural venous engorgement has been reported with internal jugular thrombosis and superior vena cava obstruction.[9]
The neurological symptoms and signs in IVC agenesis patients may be due to two causes. First, dilated anterior internal vertebral veins causing direct mechanical irritation or compression of cauda equina nerve roots in the spinal canal and/or foramen. Second, stasis of the blood flow in the radicular veins might lead to ischemia of the cauda equina roots. The patient with IVC agenesis also has a higher rate of DVT (10%) because of inadequate collateral venous return.[10] Inadequate flow in collateral vessels results in chronic venous hypertension and venous stasis leads to the formation of further venous collaterals and precipitate thrombosis. Some of these patients may also show postural changes or exercise predisposing the onset of symptoms.[11] In the erect posture, spinal phlebography studies have shown that intracranial venous return reaches the internal vertebral plexus and hence headache due to raise intracranial venous pressure may be noted in some patients. Hence, MRI done in regular supine position may possibly be underestimating the epidural venous dilatation.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Epidural venous plexus engorgement due to inferior vena cava thrombosis resulting in cauda equina syndrome: Case report and literature review. Surg Neurol Int. 2018;9:129.
- [CrossRef] [PubMed] [Google Scholar]
- Engorged venous plexus mimicking adjacent segment disease: Case report and review of the literature. Surg Neurol Int. 2020;11:104.
- [CrossRef] [PubMed] [Google Scholar]
- Symptomatic lumbar epidural varices. Report of two cases. J Neurosurg. 1994;80:914-8.
- [CrossRef] [PubMed] [Google Scholar]
- Lumbar epidural varix as a cause of radiculopathy. Spine (Phila Pa 1976). 1994;19:2122-6.
- [CrossRef] [PubMed] [Google Scholar]
- Inferior vena cava thrombosis presenting as lumbar radiculopathy. Am J Phys Med Rehabil. 2007;86:952-5.
- [CrossRef] [PubMed] [Google Scholar]
- Collateral pathways in inferior vena caval obstruction in children, including the cavo-portal route. Pediatr Radiol. 1981;10:225-8.
- [CrossRef] [PubMed] [Google Scholar]
- Epidural venous plexus enlargements presenting with radiculopathy and back pain in patients with inferior vena cava obstruction or occlusion. Spine (Phila Pa 1976). 2004;29:2419-24.
- [CrossRef] [PubMed] [Google Scholar]
- A very rare cause of low-back pain and sciatica: Deep vein thrombosis due to absence of the inferior vena cava mimicking the clinical and radiological signs of lumbar disc herniation. J Neurosurg Spine. 2011;15:164-7.
- [CrossRef] [PubMed] [Google Scholar]
- Cervical myelopathy from dilated epidural veins: Case report of intracranial outflow obstruction treated with a sigmoid sinus to internal jugular vein bypass. BNI Q. 1998;14:13-7.
- [Google Scholar]
- Absent inferior vena cava resulting in exercise-induced epidural venous plexus congestion and lower extremity numbness: A case report and review of the literature. Spine (Phila Pa 1976). 2010;35:E921-4.
- [CrossRef] [PubMed] [Google Scholar]
- Transient cauda equina compression syndrome and headache caused by internal vertebral venous plexus engorgement in a teenage female with vena cava inferior agenesis and iliac vein thrombosis. J Neurol Neurosurg Psych. 2007;78:1283-4.
- [CrossRef] [PubMed] [Google Scholar]





