Translate this page into:
Dihydroergotamine Complicating Reversible Cerebral Vasoconstriction Syndrome in Status Migrainosus
Address for correspondence: Dr. Naresh Mullaguri, S80, Cerebrovascular Center, 9500 Euclid Avenue, Cleveland Clinic Foundation, Cleveland, Ohio 44195, USA. E-mail: mullagn@ccf.org
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Reversible cerebral vasoconstriction syndrome (RCVS) is a clinicoradiological syndrome that occurs due to dysfunction of cerebrovascular autoregulation. It is characterized by recurrent thunderclap headache from cerebral vasoconstriction which can cause ischemic infarction, spontaneous intraparenchymal and subarachnoid hemorrhage. This syndrome can be triggered by a variety of etiologies including medications, infectious, and inflammatory conditions. The diagnosis is often delayed due to unawareness among the health-care providers and delayed neuroimaging evidence of vasoconstriction with or without ischemic and/or hemorrhagic infarction. Status migrainosus is a prevalent condition requiring emergency room visits and inpatient admission. Thus, patients with RCVS can be easily misdiagnosed with migraine. We report a patient with RCVS misdiagnosed as status migrainosus with visual aura, treated with intravenous dihydroergotamine with worsening of cerebral vasoconstriction and lead to ischemic and hemorrhagic complications. We discuss this complication and provide guidance on differentiating between migraine and RCVS.
Keywords
Dihydroergotamine
intracerebral hemorrhage
migraine
reversible cerebral vasoconstriction syndrome
vasculopathy
INTRODUCTION
Reversible cerebral vasoconstriction syndrome (RCVS) is characterized by recurrent thunderclap headache and cerebral vasoconstriction that can result in cerebral ischemia and/or various forms of cerebral hemorrhage including subarachnoid hemorrhage and spontaneous intraparenchymal hemorrhage.[12] In this condition, there is transient dysregulation of arterial tone within cerebral vessels.[3] This may be triggered by an overactive sympathetic system and endothelial dysfunction that leads to arterial vasoconstriction.[3] The diagnosis of RCVS can be challenging given that primary headache disorders are common in the general population, and patients with chronic headaches can develop acute severe headaches which warrant admission to a hospital.[4] Therefore, identifying the population at risk for the development of a secondary headache due to RCVS among those with a primary headache disorder is critical because the standard treatment of migraine headaches often includes therapies in which vasoconstriction is the primary mechanism of action, such as with intravenous dihydroergotamine (DHE). The use of these medications can worsen a headache caused by RCVS especially with concomitant drugs such as triptans, serotonergic anti-depressants, or methamphetamines.[5]
According to the Food and Drug Administration, DHE is contraindicated in patients with previous history of ischemic stroke or basilar and hemiplegic migraines due to the risk of precipitating recurrent events via cerebral vasoconstriction. Other conditions such as prior history of cerebrovascular malformation or cerebral hemorrhage are not listed as specific contraindications to the use of DHE.[6] We present a case of a patient with a history of a primary headache disorder who presented with a thunderclap headache. Neuroimaging demonstrated blooming artifact. After being treated with intravenous DHE, our patient developed focal neurological deficits and further imaging demonstrated distal vasculopathy and new intraparenchymal hemorrhages. This case demonstrates the fact that patients with RCVS should not receive intravenous DHE, even if they have an underlying history of migraine.
CASE REPORT
A 47-year-old Caucasian woman with a history of migraine headaches (last headache approximately 8 months ago), methamphetamine abuse (approximately 8 months of sobriety), and depression currently treated with sertraline presented with sudden onset of bilateral frontal-occipital headache. The headache started while playing cards with her friends 4 days before admission. She described the headache similar to her typical migraine, pulsating in character, with photophobia, and nausea. However, it was different due to severity of pain and periodic exacerbations at least 2–3 times a day up to 10/10 in intensity with gradual relief to 4/10 in the interim. The pain was worsened by neck flexion but not Valsalva maneuvers. She had two different emergency room visits in the past 4 days due to this pain and received oral opioids along with a combination of intravenous prochlorperazine, ketorolac, and diphenhydramine. These initially alleviated the pain, but the pain returned. She was admitted to our neurology floor. Her neurological examination including fundus examination was unremarkable. She had two computed tomography (CT) scans of the head that were reported by radiology as unremarkable. Magnetic resonance imaging (MRI) of her brain showed a small T2/fluid-attenuated inversion recovery hypointense nonenhancing lesion in the right occipital lobe with blooming artifact [Figure 1]. MRI venogram was negative.
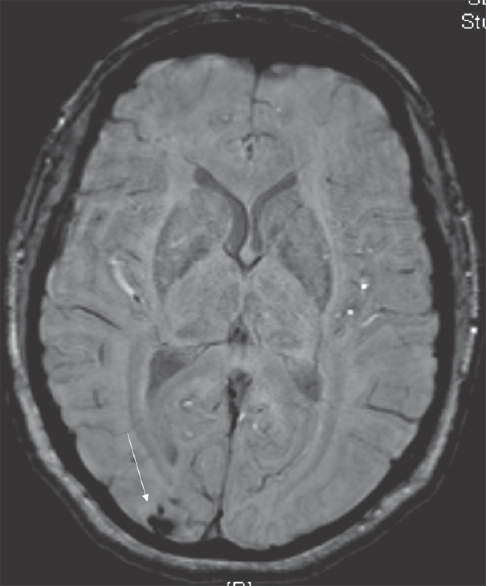
- Magnetic resonance imaging on admission. Magnetic resonance imaging shows blooming artifact (arrow) on the susceptible weighted imaging
She was treated with promethazine, ketorolac, and diphenhydramine for acute headache. She was also started on topiramate (25 mg twice a day) and valproic acid (500 mg twice a day) for chemoprophylaxis given the frequency of the headaches. Two days after admission, she began to experience visual disturbances of people and objects seeming distant and distorted suggestive of “Alice in Wonderland” phenomenon with worsening nausea and vomiting. These were thought to be a migrainous aura. She received two doses 1 mg of intravenous DHE 8 h apart. Shortly thereafter, she became somnolent and developed a new onset left-sided homonymous hemianopia. A stat CT scan of the head showed right frontoparietal and left parietooccipital parenchymal hemorrhages [Figure 2]. Digital subtraction angiography (DSA) was performed which showed moderate-to-severe vasospasm in bilateral middle cerebral artery (MCA), anterior cerebral artery (ACA), and posterior cerebral artery (PCA) territories [Figure 3].
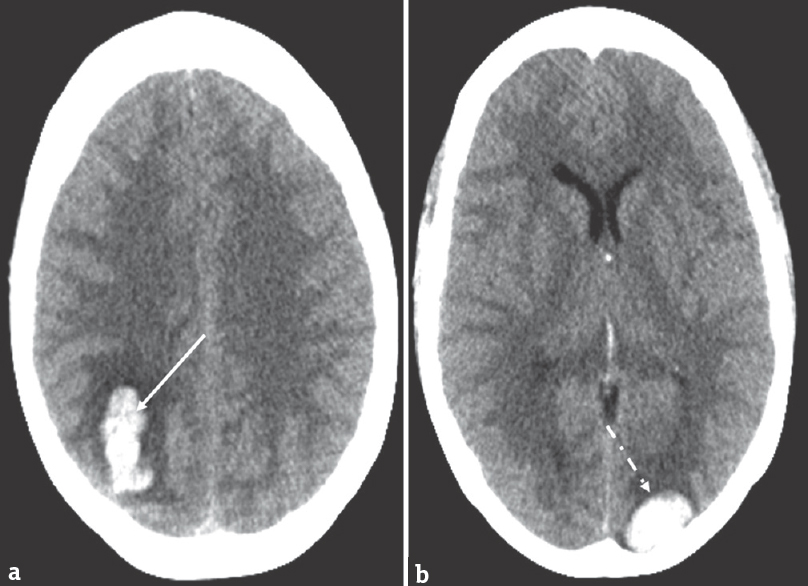
- Computed tomography of the head after dihydroergotamine. Computed tomography shows right parietal hemorrhage (a, solid arrow) and left parieto-occipital hemorrhage (b, dashed arrow)
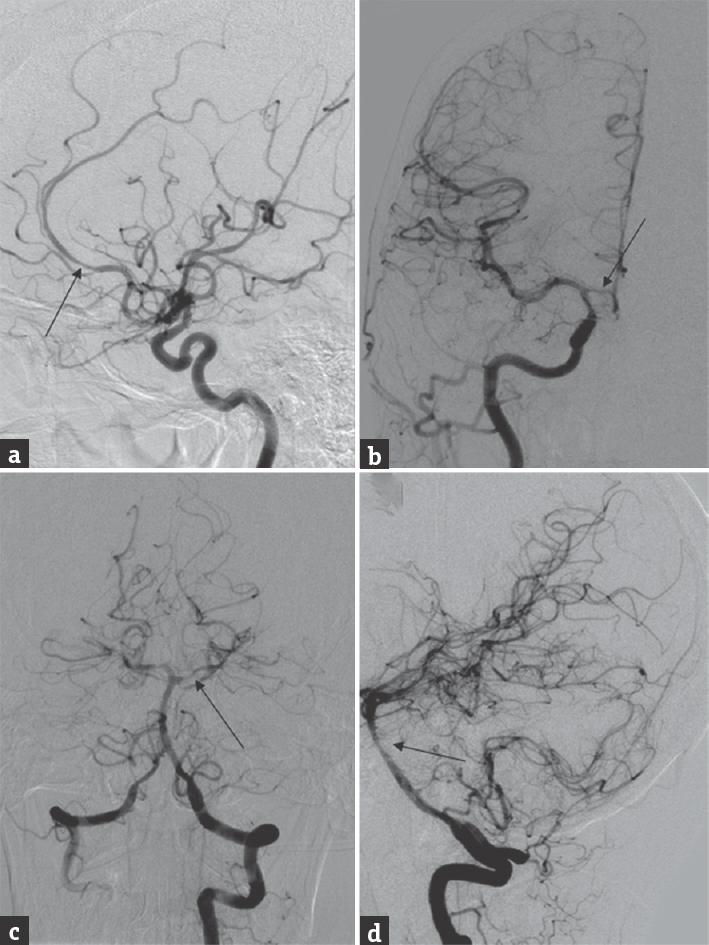
- Digital subtraction angiography. Digital subtraction angiography showing diffuse vasculopathy in the anterior circulation (a and b, arrows) and posterior circulation (c and d, arrows)
A lumbar puncture was performed to rule a vasculitic process. Cerebrospinal fluid biochemical analysis showed protein 47 mg/dl, glucose 71 mg/dl, white blood cell (WBC) 8 mcL with a lymphocytic predominance and red blood cell (RBC) 3000/mcL. Systemic markers for inflammation, vasculitis, and autoimmune panel were negative. She was suspected of having RCVS. Five days into admission, she developed new right-sided hemiparesis and ataxia. MRI brain demonstrated acute ischemic infarctions in the right cerebellum, left ACA, and bilateral PCA distributions with no change in the size of her previous hemorrhages [Figure 4]. Repeat lumbar puncture showed normalization of previously elevated protein 45 mg/dl, glucose 59 mg/dl, WBC 3/mcL, and RBC 55/mcL.
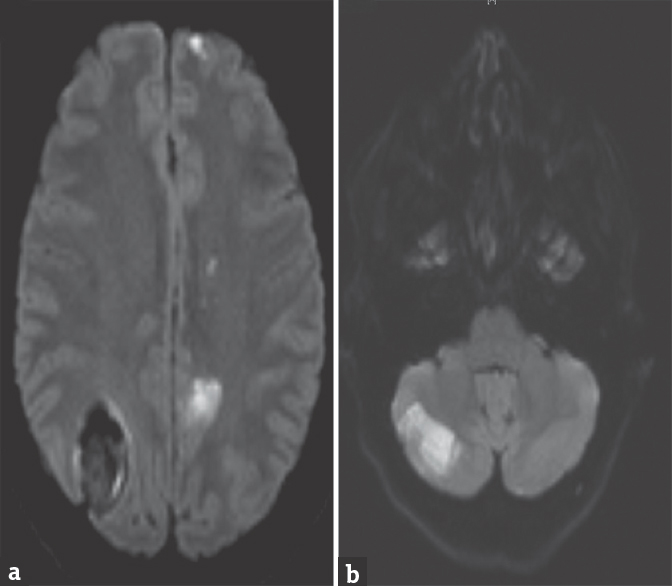
- Magnetic resonance imaging. Magnetic resonance imaging showing hyperintensity on diffusion-weighted sequence in the anterior circulation (a) and in the cerebellum (b)
A repeat DSA showed vasculopathy of bilateral PCA along with left MCA and ACA territories. Intra-arterial verapamil was administered without much improvement of vasospasm. Her RCVS management included tight regulation of systolic blood pressure between 140 and 160 mmHg along with maintaining euvolemia. She was also started on oral verapamil and initially given a short course of prednisone which was discontinued after 4 doses. She continued to improve and was eventually discharged home with outpatient rehabilitation services after 13 days.
DISCUSSION
We presented a patient presenting to the emergency department (ED) with headaches and evidence of small hemorrhage on MRI. However, she was initially treated with DHE because this hemorrhage was interpreted as benign vascular malformation and also due to the fact that she had a history of migraines. We now suspect that she had RCVS on admission based on the history of recurrent thunderclap headaches in the days preceding her admission as well as the concomitant use of vasoconstrictor agents including serotonergic antidepressants and previous methamphetamine use. The use of intravenous DHE exacerbated the cerebral vasoconstriction that was already present, and she progressed to developing multifocal cerebral hemorrhages and diffuse cerebral vasculopathy related to worsening RCVS.
We present this case to bring to attention the importance of the clinical history in headache patients and subtle findings on neuroimaging that may indicate a secondary etiology for headache. Headache, as a presenting symptom to the ED, is common, accounting for 2.4% of all ED visits in the United States.[7] Approximately 60% of the headache admissions to the hospital are for the treatment of migraine headaches. However, secondary causes of headaches are not uncommon constituting about 40% of the total headache admissions.[8]
DHE has effects at multiple receptors including dopaminergic, adrenergic, and several serotonergic receptors. The drug's action of agonism of serotonin receptors (5-HT1B, 5-HT1D) results in vasoconstriction of meningeal vessels and helps to inhibit trigeminal peptide release which assists in pain relief during headaches and has a further vasoconstrictor effect on cerebral arteries due to their sympathetic innervation.[9] Currently, the use of DHE is contraindicated in the setting of known peripheral arterial disease, prior history of ischemic stroke, history of coronary vasospasm (angina), and history of basilar and/or hemiplegic migraines.[10] The finding of blooming artifact on neuroimaging is not an absolute contraindication for the use of DHE, because history of prior cerebral hemorrhage is not listed as a contraindication to DHE although case reports have reported DHE causing intracerebral and subarachnoid hemorrhages as well as worsening vasospasm.[11]
Our patient presented with RCVS as heralded by the onset of the thunderclap headache as well as the small occipital hemorrhage seen on initial neuroimaging that was interpreted as an asymptomatic vascular malformation. Prior to the administration of DHE, our patient developed the “Alice in Wonderland phenomenon,” which is a visual distortion symptom that may have been secondary to the posterior circulation ischemia and/or evolving occipital hemorrhage. The pathophysiology of RCVS includes cerebral vasoconstriction starting in distal vessels.[12] In our patient, this vasoconstriction following DHE administration likely precipitated the initial intracerebral hemorrhage. Additionally, vasoactive drugs (triptans and ergot alkaloids) can exacerbate cerebral vasoconstriction, precipitate arterial vasospasm, and lead to complications like multi-focal intracerebral hemorrhage, infarction as described in our case.[12] Our objective is to raise awareness of the importance of screening naïve patients before using intravenous DHE for any abnormalities in imaging that may suggest a secondary cause of headache, such as RCVS rather than migraine.
CONCLUSIONS
RCVS and cerebral vascular malformations are not listed as a warning or contraindication to the use of DHE. We would suggest that patients with a suspected diagnosis of RCVS and neuroimaging evidence of blooming artifact be warned against the use of DHE and by extension other abortive migraine therapies that precipitates vasoconstriction. We conclude that a new onset headache in a patient with prior history of migraine warrants further structural and vascular neuroimaging to rule out RCVS and vascular malformations prior to initiating DHE therapy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Hemorrhagic manifestations of reversible cerebral vasoconstriction syndrome: Frequency, features, and risk factors. Stroke. 2010;41:2505-11.
- [Google Scholar]
- The typical thunderclap headache of reversible cerebral vasoconstriction syndrome and its various triggers. Headache. 2016;56:657-73.
- [Google Scholar]
- The link between migraine, reversible cerebral vasoconstriction syndrome and cervical artery dissection. Headache. 2016;56:645-56.
- [Google Scholar]
- Reversible cerebral vasoconstriction syndrome: Case report. J Headache Pain. 2009;10:295-8.
- [Google Scholar]
- A retrospective analysis of triptan and DHE use for basilar and hemiplegic migraine. Headache. 2016;56:841-8.
- [Google Scholar]
- Diagnosis and management of the primary headache disorders in the emergency department setting. Emerg Med Clin North Am. 2009;27:71-87. viii
- [Google Scholar]
- Primary headache in emergency department: Prevalence, clinical features and therapeutical approach. J Headache Pain. 2005;6:287-9.
- [Google Scholar]
- Headache, cerebral aneurysms, and the use of triptans and ergot derivatives. Headache. 2015;55:739-47.
- [Google Scholar]
- Dihydroergotamine, ergotamine, methysergide and sumatriptan – Basic science in relation to migraine treatment. Headache. 2012;52:707-14.
- [Google Scholar]
- The clinical and radiological spectrum of reversible cerebral vasoconstriction syndrome.A prospective series of 67 patients. Brain. 2007;130:3091-101.
- [Google Scholar]
- Hemorrhagic reversible cerebral vasoconstriction syndrome: Features and mechanisms. Stroke. 2016;47:1742-7.
- [Google Scholar]






