Translate this page into:
Dentate Hyperintensities-The Imaging Signature of Metronidazole Induced Encephalopathy
Address for correspondence: Dr. Sachin Sureshbabu, Department of Neurology, St. Stephen's Hospital, New Delhi, India. E-mail: drsachins1@rediffmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Specific neuroimaging features are uncommonly observed in toxic- or drug-induced encephalopathies. We present a case of metronidazole-induced encephalopathy (MIE) revealing a fairly diagnostic appearance of symmetric dentate hyperintensities. Metronidazole is a nitroimidazole antimicrobial drug used commonly to treat infections caused by anaerobic bacteria and protozoa. Neurological manifestations of toxicity include cerebellar syndrome, seizures, autonomic neuropathy, optic neuropathy, peripheral neuropathy, and rarely encephalopathy.
A 60-year-old male who had received a cumulative dose of 60 g metronidazole for 25 days for amebic liver abscess, developed acute onset encephalopathy in the form of decreased interaction with family members, keeping to himself, and prominent gait ataxia. Within 2 days of the onset of the symptoms, patient's condition further deteriorated and the patient became stuporous. 1.5 Tesla magnetic resonance imaging (MRI) of the brain showed symmetric T2 hyperintensities over bilateral dentate nuclei [Figure 1]. The investigative work up comprising of complete blood counts, electrolytes, glucose, renal and liver function tests, serum ammonia, thyroid function tests, anti-thyroid antibodies and cerebrospinal fluid (CSF) examination was normal. Electroencephalogram showed generalized symmetric slowing with no epileptiform activity. With the characteristic brain MRI findings consistent with MIE, metronidazole was immediately stopped. Remarkable recovery was observed over next 2 weeks.
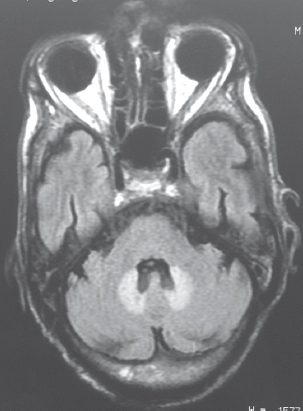
- Symmetrical dentate hyperintensities best seen on fluid attenuation inversion recovery images
The exact incidence of MIE is still not established. Most brain lesions induced by metronidazole toxicity are reversible, but irreversible nature of the lesions has also been reported. T2 and fluid attenuation inversion recovery hyperintensities of the cerebellar dentate nuclei with or without diffusion restriction are the most common neuroimaging abnormality seen in MIE.[123] The signal changes can involve the brainstem (dorsal pons and medulla), corpus callosum, and the cerebral white matter as well.[3]
The clinicoradiological syndrome epitomizes a category of disorders eloquently described as energy deprivation syndromes which also includes entities such as Leigh disease, maple syrup urine disease (MSUD), Wernicke encephalopathy, methyl bromide intoxication, posterior reversible encephalopathy syndrome (PRES), and multiple sclerosis (MS).[4] The disruption of metabolic energy pathways selectively affects the posterior fossa elements and the periventricular white region. The brunt of insult in Leigh's is usually in the basal ganglia but the entire brainstem can be involved while Wernicke targets the mamillary bodies, inferior colliculi, and periaqueductal gray matter. Branched chain amino acid accumulation in the acute phase of MSUD causes failure of the Na-K pump leading to intramyelinic edema manifesting a similar radiological picture. Recurrent episodes and occurrence in the pediatric age group would suggest this diagnosis. Biochemical assay during the episode along with MR spectroscopy is helpful for diagnosis.[5] Nonexposure to organic solvents rules out methyl bromide toxicity.[6] MS can present with predominantly infratentorial lesions, but isolated involvement of these structures is rare. Careful search for other neuraxial involvement should be made when the clinical setting is suggestive. Patchy involvement of cerebellum and brainstem can occur in PRES although the typical distribution is parieto-occipital.
The temporal relationship to metronidazole use, the characteristic findings in the brain MRI, normal laboratory parameters, and remarkable recovery after discontinuing metronidazole helped us establish the diagnosis of MIE. Free radical injury, mitochondrial toxicity, and interference with GABAergic neurotransmission in the cerebellum and brainstem are the proposed mechanisms that lead to localized axonal swelling with increased water content.[7]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We acknowledge the Director of St. Stephen's Hospital and the hospital management for allowing us to publish this Neuroimage.
REFERENCES
- Reversible metronidazole-induced lesions of the cerebellar dentate nuclei. N Engl J Med. 2002;346:68-9.
- [Google Scholar]
- Reversible magnetic resonance imaging findings in metronidazole-induced encephalopathy. Neurology. 1995;45(3 Pt 1):588-9.
- [Google Scholar]
- MR imaging of metronidazole-induced encephalopathy: Lesion distribution and diffusion-weighted imaging findings. AJNR Am J Neuroradiol. 2007;28:1652-8.
- [Google Scholar]
- Clinical and neuroradiological spectrum of metronidazole induced encephalopathy: Our experience and the review of literature. J Clin Diagn Res. 2016;10:OE01-9.
- [Google Scholar]
- Neurological manifestation of methyl bromide intoxication. J Med Assoc Thai. 2008;91:421-6.
- [Google Scholar]





