Translate this page into:
Delayed Visual Loss Following Transcranial Surgery for Tuberculum Sella Meningioma
Address for correspondence: Dr. Girish Menon, Department of Neurosurgery, Kasturba Medical College, Manipal - 576 104, Karnataka, India. E-mail: girish.menon@manipal.edu
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Postoperative visual loss is a dreaded complication following transcranial excision of tuberculum sella meningioma. Visual deterioration is commonly noticed immediately after surgery, and delayed deterioration after 72 h is uncommon. We report a case of delayed postoperative deterioration in a 48-year-old female and discuss the possible mechanisms.
Keywords
Transcranial
tuberculum sella meningioma
visual loss
INTRODUCTION
Postoperative visual loss is a dreaded complication following transcranial excision of tuberculum sella meningioma. Visual deterioration is commonly noticed immediately after surgery and delayed deterioration after 72 hours is uncommon. We report a case of delayed post operative deterioration in a 48years old lady and discuss the possible mechanisms.
CASE REPORT
A 48-year-old female presented with 1 year history of headache and progressive blurring of vision of the right eye. On examination, she had only perception of light in her right eye, and fundoscopy revealed primary optic nerve atrophy in the right eye. The left eye vision and fundus examination were normal. Imaging [Figure 1] revealed a suprasellar enhancing dural-based lesion suggestive of a tuberculum sella (TS) meningioma. She underwent right pterional craniotomy and Simpson's grade II excision of the meningioma along with intradural optic canal deroofing. Postoperative recovery was uneventful, and she continued to perceive light in her right eye. On the 7th day, she complained of complete blindness of her right eye. Repeat imaging was not contributory. Fundoscopy showed a pale atrophic disc. She was treated with steroids for 5 days. Her vision failed to improve, and 6 months after surgery, she remains blind in her right eye.
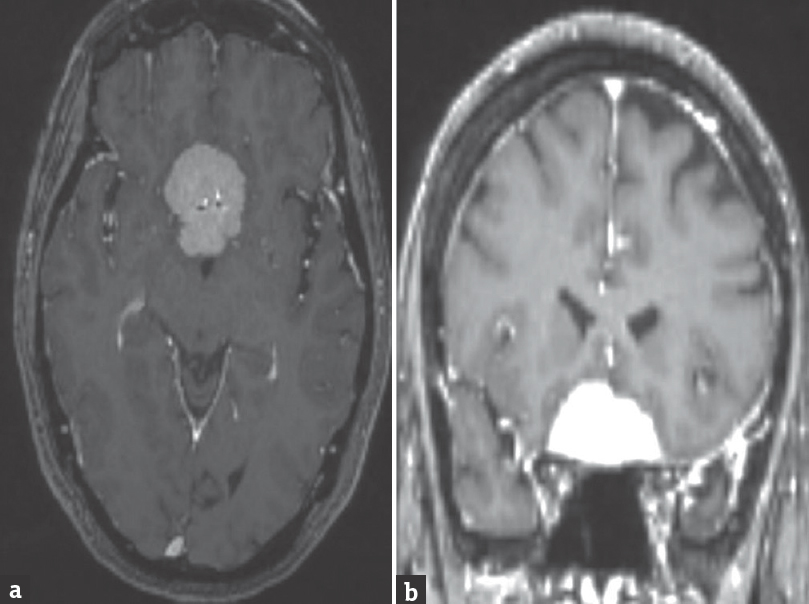
- Axial (a) and coronal (b) images showing an enhancing suprasellar mass lesion suggestive of meningioma
DISCUSSION
Suprasellar meningiomas constitute 5%–10% of all intracranial meningiomas. TS meningioma refers to tumors arising from tuberculum, limbus sphenoidale, chiasmatic sulcus, and diaphragm sella. TS meningiomas generally present with visual symptoms, and deterioration of vision is the most common indication for surgery in patients with TS meningioma. Analyzing the anatomical origin of their 100 cases of TS meningiomas, Kim et al. have proven that these tumors have their point of origin laterally near one of the optic canals in >85% of cases and then proceed toward the midline. Visual symptoms can thus be asymmetric and could be either from mechanical compression from the tumors itself or impingement of the nerve in a tight optic canal. Considerable debate exists regarding the ideal mode of approach and the extended endoscopic transsphenoidal approach seems to be increasingly becoming popular. Comparing endoscopic endonasal versus open transcranial resection of TS meningiomas, Komotar et al. observed that the visual outcome is better with an inferior approach – both in terms of improvement of existing deficits as well as in terms of postoperative deterioration.[1] In terms of extent of resection and risk of cerebrospinal fluid leak, the transcranial approach has an edge and still remains the most common surgical approach for TS meningiomas.[1]
Different studies have shown a 58.4% of improvement and 12.9% risk of postoperative deterioration following transcranial surgery.[12] Visual deterioration is commonly noticed immediately after surgery and is linked to multiple reasons. These include intraoperative manipulation of the nerve, thermal injury due to use of cautery and drills and any obvious vascular injury. In the authors’ personal series of 71 TS meningiomas, postoperative worsening of vision occurred in 3 (4.22%) cases and was apparent immediately postoperatively in all the cases. However, in this case, the visual deterioration was noticed at the time of discharge 7 days after surgery.
The reasons for delayed deterioration remains unclear in our case. In a similar report of two patients, Santarius et al.[3] postulate an ischemic etiology due to vasospasm. They performed angiography and verapamil infusion in their patients, and although angiography did not reveal any significant vasospasm, verapamil infusion did help in recovery in one of the patients. Santarius et al.[3] have thus evolved a protocol of hypervolemic hypertensive therapy for 48 h postoperatively for all tuberculum and perioptic meningioma patients in whom the clinoid or optic canal is drilled. Their postulate being that during surgery a critical quantum of optic pathway-supplying vasculature is compromised making the tissues vulnerable to ischemia, and it would be ideal to avoid further tissue hypoperfusion by ensuring adequate blood pressure.
Venous insults manifest in a subacute fashion unlike an arterial ischemia, and occlusion of venous drainage could be related to delayed deterioration. Preservation of veins in the suprasellar area is not carried out as diligently as in other areas such as parasagittal area. Our case did have a small venous injury which was thought to be inconsequential at the time of surgery. Venous drainage of the optic apparatus probably needs to be studied more, and all attempts should be made to preserve them whenever possible.
It is well known that decompression of a critical spinal canal stenosis can result in postoperative neurological deterioration secondary to spinal cord edema. Probably, a similar mechanism with sudden decompression resulting in probable reperfusion injury could happen after optic nerve decompression. We believe that more the severity of compression, more the chances of deterioration with decompression. Thus, patients with significant preoperative optic nerve compression as evidenced by severe optic atrophy and minimal vision (hand movement or perception of light) are more likely to have postoperative deterioration as was seen in our patient.
Thermal injury due to cautery and drills and mechanical injury due to manipulation could at times result in delayed optic nerve edema which could be another possible etiology for delayed visual deterioration; most of the TS meningiomas have an optic canal extension, and Mortazavi et al. have suggested early decompression of the optic canal by extradural clinoidectomy and optic canal deroofing to reduce intraoperative manipulation of the optic nerve.[4] This along with careful use of cautery with liberal irrigation of saline while coagulating the dural attachment are some maneuvers which can prevent postoperative visual deterioration.
CONCLUSION
Postoperative visual deterioration is not an uncommon sequel following transcranial excision of a TS meningioma. The deterioration can occur immediately or few days postoperatively. Patients with severe optic atrophy and poor vision are more likely to have this complication. The possible mechanism could be vascular, mechanical, or sequel to sudden decompression. Extradural clinoid drilling, adequate hydration during the use of drill and cautery, gentle and careful handling of optic nerves, intraoperative use of papaverine, and postoperative hypervolemic hypertensive therapy are a few prophylactic steps which could prevent this catastrophe.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- The endoscope-assisted ventral approach compared with open microscope-assisted surgery for clival chordomas. World Neurosurg. 2011;76:318-27.
- [Google Scholar]
- Anatomical origin of tuberculum sellae meningioma: Off-midline location and its clinical implications. World Neurosurg. 2016;89:552-61.
- [Google Scholar]
- Delayed neurological deficit following resection of tuberculum sellae meningioma: Report of two cases, one with permanent and one with reversible visual impairment. Acta Neurochir (Wien). 2014;156:1099-102.
- [Google Scholar]
- Planum sphenoidale and tuberculum sellae meningiomas: Operative nuances of a modern surgical technique with outcome and proposal of a new classification system. World Neurosurg. 2016;86:270-86.
- [Google Scholar]






