Translate this page into:
Tuberculum Sella Meningioma: Surgical Management and Results with Emphasis on Visual Outcome
Rajneesh Kachhara, MCh Department of Neurosurgery, Institute of Neurosciences, Medanta Multi-Speciality Hospital Indore, Madhya Pradesh 452010 India rkachhara@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background Tuberculum sella meningioma form a distinct surgical entity with significant morbidity for the patient due to early and profound visual involvement. Surgical treatment of tuberculum sella meningioma is challenging in view of the proximity of vital neuro-vasculature. These lesions may be approached via a high-route (trans-cranial) or a low-route (trans-sphenoidal).
Materials and Methods The authors present a consecutive series of 36 patients, operated by the first author from 1996 onward, with an analysis of clinical presentation (emphasizing visual deterioration), imaging features, operative approaches, and outcome with postoperative visual status.
Results There were 36 patients (72 eyes) in the series, 75% females and 25% males. The mean age of patients was 48.05 ± 10.02 years. In all, 88.89% had visual diminution, 50% had headache, 5.56% had behavioral changes, and 2.78% had seizures. The mean tumor size was 4.01 ± 1.01 cm. The frontotemporal approach was employed in 66.67% of patients, and all patients underwent a right-sided approach. There was no significant difference between improvement in the vision between the right eye and left eye, despite the fact that right-sided approach was employed in nearly cases.
Conclusion While tuberculum sella meningioma have profound morbidity in terms of visual deterioration, timely surgical intervention may help patients gain serviceable vision postoperatively. We advocate the trans-cranial approach and find no difference in visual outcomes on employing right-sided approach, regardless of the side with worse vision.
Keywords
meningioma
tuberculum sella
visual outcome
trans-cranial
trans-sphenoidal
Introduction
Anterior skull base meningiomas comprise ∼40% of all intracranial meningiomas, of which ∼25% are tuberculum sella meningioma—a distinct group of anterior skull base meningiomas (thus forming ∼10% of all intracranial meningiomas).1 2 These tumors were first reported as autopsy finding by Steward in 1899 and were first removed completely by Cushing in 1916.3 The present anatomical knowledge ascribes the origin of these tumors from tuberculum sella, chiasmatic sulcus, limbus sphenoidale, and the diaphragma sella.1 2 4 Arising from above-mentioned structures, these tumors can extend anteriorly to involve the planum sphenoidale, laterally to involve optic nerves and carotid artery, postero-superiorly to involve the optic chiasm, anterior cerebral artery complex, hypothalamus, and sometimes into the sella.
It is common for these tumors to extend into both optic canals and involve chiasm; consequently, visual symptoms are very common presentation even in small tumors, usually starting in one eye and progressing to the other.2
These tumors, like all other meningiomas, are found more commonly in females (3:1) and their most common presentation is in the fourth or fifth decade of life.1 2
Over the years, treatment of these tumors has remained challenging in view of the proximity of vital neuro-vasculature. With time, various approaches have come to be employed for resection of these tumors, ranging from microsurgical excision to endo-nasal endoscopic approaches with proponents of each claiming safer and better results.
Authors present a consecutive series of 36 patients, operated by the first author from 1996 onward, with an analysis of clinical presentation (emphasizing visual deterioration), imaging features, operative approaches, and outcome with postoperative visual status.
Materials and Methods
Inclusion Criteria: This was a series of surgically treated patients of tuberculum sella meningioma by the first author consecutively at three centers viz., Sree Chitra Tirunal Institute for Medical Sciences and Technology (SCTIMST), Trivandrum, Bombay Hospital, Indore and Medanta Super-specialty Hospital, Indore, Madhya Pradesh (MP), India over a period of 25 years. A total of 36 patients were operated during this period.
Investigations: All patients underwent imaging that included computed tomography (CT) scan or magnetic resonance imaging (MRI) of the brain with contrast study. Visual acuity was documented for all patients and field charting was done.
Treatment: All patients in this series underwent surgical treatment via one of the following routes–fronto-temporal with or without orbital osteotomy, fronto-lateral, unilateral frontal (Seeger's modification), bi-frontal and microscopic trans-sphenoidal.
Outcome Analysis: Patients were followed up for a minimum period of 6 months. Postoperative visual status was documented as well as improvement in other complaints of patient.
The patient data were collected and analyzed using the SPSS 23 software. (IBM Corp, Armonk, New York)
Results
Demographic details such as sex, age, and presenting complaints of the patients are summarized in Table 1.
|
No. of patients (No. of eyes) |
36 (72) |
|
Female |
27 (54) |
|
Male |
9 (18) |
|
Mean age (median age) |
48.05 ± 10.02 years (48 years) |
|
Female |
47.37 ± 10.23 years (48 years) |
|
Male |
50.11 ± 9.62 years (52 years) |
|
Presenting complaints |
|
|
Visual deterioration (M/F) |
32–88.89% (7/25) |
|
Headache (M/F) |
18–50% (4/14) |
|
Seizures (M/F) |
1–2.78% (1/0) |
|
Behavioral changes (M/F) |
2–5.56% (0/2) |
In all, 14 patients presented with both headache and visual diminution, 1 patient had headache and behavioral changes, and 1 patient had headache, visual diminution and behavioral changes (Fig. 1).
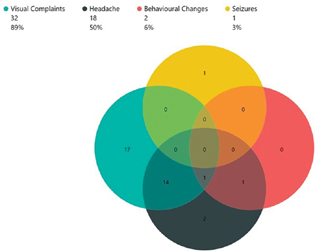
-
Fig. 1 Patient symptoms.
Fig. 1 Patient symptoms.
Visual Complaints: Diminution of vision was the most common complaint. Visual deterioration was graded in accordance with the World Health Organization (WHO) recommended ICD-10 criteria, on an ordinal scale, from grade 0 to grade 5.5 Of the 32 patients presenting with visual diminution, only 2 patients presented with grade 0 visual loss in one eye while having visual deterioration in the other; in all other 30 patients, the involvement was bilateral. Thus, 62 “eyes” in the series had visual diminution.
Two patients had grade 5 visual loss (complete blindness: no perception of light) in both eyes, while 14 other patients had grade 5 vision loss in one eye. Thus, there were 18 “eyes” in the series were completely blind.
Preoperative visual diminution in both right and left eyes is summarized in Table 2.
|
Right eye |
Total |
|||||||
|---|---|---|---|---|---|---|---|---|
|
Gr 0 |
Gr 1 |
Gr 2 |
Gr 3 |
Gr 4 |
Gr 5 |
|||
|
Left eye |
Gr 0 |
4 |
4 |
|||||
|
Gr 1 |
1 |
2 |
3 |
|||||
|
Gr 2 |
3 |
1 |
1 |
5 |
||||
|
Gr 3 |
1 |
1 |
1 |
1 |
4 |
|||
|
Gr 4 |
1 |
2 |
3 |
6 |
12 |
|||
|
Gr 5 |
1 |
2 |
3 |
2 |
8 |
|||
|
Total |
6 |
2 |
4 |
6 |
8 |
10 |
36 |
|
The best vision preoperatively (both eyes taken together) was grade 0 in 6 patients, grade 1 in 4 patients, grade 2 in 6 patients, grade 3 in 6 patients, grade 4 in 12 patients, and grade 5 in 2 patients with median best vision being grade 3 (Table 3).
|
Best preoperative vision |
Total |
|||||||
|---|---|---|---|---|---|---|---|---|
|
Gr 0 |
Gr 1 |
Gr 2 |
Gr 3 |
Gr 4 |
Gr 5 |
|||
|
Best postoperative vision |
Gr 0 |
6 |
6 |
|||||
|
Gr 1 |
4 |
1 |
5 |
|||||
|
Gr 2 |
4 |
4 |
1 |
9 |
||||
|
Gr 3 |
1 |
1 |
7 |
1 |
10 |
|||
|
Gr 4 |
2 |
1 |
3 |
|||||
|
Gr 5 |
1 |
1 |
||||||
|
Patient Expired |
1 |
1 |
2 |
|||||
|
Total |
6 |
4 |
6 |
6 |
12 |
2 |
36 |
|
The grade of vision loss was worse in the left eye in 11 patients, in the right eye in 11 patients, and was same in both eyes in 14 patients.
The median grade of visual loss for the right eye, left eye, and all eyes taken together were all grade 4. There was no significant difference between grade of visual loss at presentation between two eyes (Friedman's test, p > 0.05). The grade of visual loss was not significantly related to the age of patient, sex of patient, and importantly, to the size of the tumor at presentation (ordinal regression, all p > 0.05).
Tumor Size: The mean and median tumor sizes in the series were 4.01 ± 1.01 cm and 4.35 cm, respectively. The tumor size was arbitrarily divided into three groups: <3 cm, 3–5 cm and > 5 cm. Most tumors were between 3 and 5 cm in size (25, 69.44%), followed by <3 cm (6, 16.67%) and > 5 cm (5, 13.89%).
Approach and Extent of Excision: The frontotemporal approach was employed in 24 patients (66.67%), frontotemporal approach with orbital osteotomy in 4 patients (11.11%), frontolateral approach in 4 patients (11.11%), trans-sphenoidal approach in 2 patients (5.56%), unilateral frontal (Seeger's modification) approach in 1 patient (2.78%), and bi-frontal approach in 1 patient (2.78%). Except for the patients undergoing trans-sphenoidal and bi-frontal approaches (3, 8.33%), all patients underwent a right-sided approach (33, 91.67%).
Nearly, all patients (34, 94.5%) underwent total excision of the tumor, while 2 patients (5.5%) underwent sub-total excision. The extent of excision was not significantly related to the approach employed or the side of approach (ordinal logistic regression, p <0.05).
Mortality: There were two mortalities in the series.
Visual Outcome: Various visual outcomes (such as postoperative vision in the right and left eyes, best vision, and grades of improvement) are summarized in Tables 3,4,5,6,7.
|
Right eye |
Total |
||||||||
|---|---|---|---|---|---|---|---|---|---|
|
Gr 0 |
Gr 1 |
Gr 2 |
Gr 3 |
Gr 4 |
Gr 5 |
Patient died |
|||
|
Left eye |
Gr 0 |
4 |
4 |
||||||
|
Gr 1 |
1 |
2 |
1 |
1 |
5 |
||||
|
Gr 2 |
1 |
4 |
1 |
6 |
|||||
|
Gr 3 |
1 |
2 |
4 |
2 |
9 |
||||
|
Gr 4 |
1 |
1 |
2 |
2 |
6 |
||||
|
Gr 5 |
2 |
1 |
1 |
4 |
|||||
|
Pt. Expired |
2 |
2 |
|||||||
|
Total |
6 |
3 |
9 |
6 |
5 |
5 |
2 |
36 |
|
|
Preoperative right eye vision |
Improvement in Vision |
Total |
||||
|---|---|---|---|---|---|---|
|
Deterioration |
Status quo |
By 1 grade |
By 2 grades |
Patient expired |
||
|
Gr 0 |
6 |
6 |
||||
|
Gr 1 |
2 |
2 |
||||
|
Gr 2 |
1 |
2 |
1 |
4 |
||
|
Gr 3 |
2 |
4 |
6 |
|||
|
Gr 4 |
1 |
3 |
3 |
1 |
8 |
|
|
Gr 5 |
2 |
5 |
1 |
2 |
10 |
|
|
Total |
2 |
17 |
13 |
2 |
2 |
36 |
|
Preoperative left eye vision |
Improvement in Vision |
Total |
||||
|---|---|---|---|---|---|---|
|
Deterioration |
Status quo |
By 1 grade |
By 2 grades |
Patient died |
||
|
Gr 0 |
4 |
4 |
||||
|
Gr 1 |
3 |
3 |
||||
|
Gr 2 |
4 |
1 |
5 |
|||
|
Gr 3 |
2 |
1 |
1 |
4 |
||
|
Gr 4 |
3 |
7 |
1 |
1 |
12 |
|
|
Gr 5 |
3 |
4 |
1 |
8 |
||
|
Total |
0 |
19 |
13 |
2 |
2 |
36 |
|
Best preoperative vision |
Improvement in best vision |
Total |
||||
|---|---|---|---|---|---|---|
|
Deterioration |
Status quo |
By 1 grade |
By 2 grades |
Patient died |
||
|
Gr 0 |
6 |
6 |
||||
|
Gr 1 |
4 |
4 |
||||
|
Gr 2 |
1 |
4 |
1 |
6 |
||
|
Gr 3 |
1 |
4 |
1 |
6 |
||
|
Gr 4 |
1 |
2 |
7 |
1 |
1 |
12 |
|
Gr 5 |
1 |
1 |
2 |
|||
|
Total |
2 |
17 |
13 |
2 |
2 |
36 |
Of the 10 eyes in the series that had no preoperative visual diminution, none had any visual deterioration postoperatively. There were 5 eyes that had grade 1 visual loss preoperatively; all these remained status quo at grade 1 visual loss postoperatively. There were 9 eyes with grade 2 visual loss in the series. Of these, 2 eyes improved to grade 1 vision, 6 remained status quo at grade 2 vision, while 1 eye had postoperative deterioration to grade 4. Grade 3 visual loss was present in 10 eyes; of these, 7 improved in visual status and 2 remained status quo. One patient with grade 3 visual diminution in one eye died. Of the 20 eyes in the series that had grade 4 visual loss, 14 improved, 4 remained status quo, 1 deteriorated while one patient with grade 4 vision in one eye died. In all, 18 eyes had grade 5 visual loss, of which 8 improved, 8 remained status quo while two patients with grade 5 vision loss in one eye died.
There was statistically significantly difference in preoperative and postoperative visual grades for both eyes as well as for the best vision of the patient (ordinal logistic regression, p < 0.05).
Apart from three patients, the approach was right-sided in all other 33 patients. This was contrary to the practice of approaching the tumor from the side of the worse eye. Of the 10 patients with worse vision in the right eye and right-sided approach, and excluding two mortalities, vision in the right eye improved in five patients and remained status quo in three; vision in the left eye (the better eye) in these patients improved in four patients, remained status quo in four. In contrast, in 10 patients with worse vision in the left eye and right-sided approach, vision in the left eye improved in 4 patients and remained status quo in 6 patients; vision in the right eye (the better eye) improved in 3 patients, remained status quo in 5 patients, and deteriorated in 2 patients. In patients with same grade of vision loss in both eyes and right-sided approach, vision in the left eye improved in 6 patients and remained status quo in 7 patients; vision in the right eye improved in 5 patients and remained status quo in 8 patients. None of the differences were statistically significant (chi-square test, p > 0.05).
Of note is that there was no significant difference between improvement in the vision between the right eye and left eye, despite the fact that the right-sided approach was employed in nearly all cases.
Discussion
Tuberculum sella meningioma is a distinct neuro-oncological entity that accounts for ∼10% of all intracranial meningiomas.1 2 6 They were first reported by Steward, first operated by Cushing, and first classified by Cushing and Eisenhardt.3 7 8 However, due to their use of the term suprasellar chiasmal syndrome for the tumors, which did not denote the anatomical origin of the lesion, there were many reports of “suprasellar meningiomas,” which included lesions arising from the planum sphenoidale, medial sphenoid ridge, olfactory groove, optic foramen, and anterior clinoid, whereas reports of true tuberculum meningioma are relatively scant in number.3 However, some authors go so far as to differentiate between tumors arising from the diaphragm sella and tuberculum as separate entities.3 9
These tumors are up to three times more common in females, similar to other meningiomas, and the frequent age of presentation is the fourth or fifth decade of life.1 2 In our series, females were, accordingly, three times the male patients and the most common age of presentation was fourth decade (36%), followed by the fifth decade (28%).
Microsurgical Anatomy and Clinical Presentation. Tuberculum sella meningioma arise from the dura of tuberculum sella, chiasmatic sulcus, planum sphenoidale, and diaphragm sella.1 2 4 6 9 10 11 In small tumors, the dural attachment may remain confined to tuberculum sella but as the tumor grows, so does the attachment and the tumor frequently fills up the pituitary fossa.12 The growth over the planum, especially, is considered to be due predisposing anatomical factors such as defect in the arachnoid or a post-fixed chiasm; further growth encases the vasculature and the optic nerves.3 12 Tuberculum sella meningioma frequently extend into the optic foramen.1 2 In addition, the growth of these tumors tends to displace the chiasm superiorly such that it straddles the tumor, causing visual deterioration.2 8
However, as these tumors often arise off-midline, visual loss in patients is more commonly asymmetric with one eye deteriorating earlier instead of a classical bi-temporal hemianopia.4 10 In our series, 22 out of 32 patients presenting with visual deterioration had asymmetric visual involvement.
Fahlbusch and Schott attempted to quantify the visual loss, taking into account the loss of acuity and field deficits and their system has remained one of the most accepted systems of quantifying visual deficits due to tuberculum sella meningioma.13
Other than visual deficits, other clinical presentations of the tumor may include headache, seizures, and behavioral changes. Hemiparesis (up to 15%) and pituitary insufficiency (up to 22%) are also reported.2 A comparison of clinical presentations, especially concerning visual deterioration, is summarized in Table 8.
Surgical Approaches
Surgical approaches to tuberculum sella meningiomas have come a long way since the time Cushing first removed the tumor. Over the time, many transcranial approaches were developed that includes pterional, frontolateral, unilateral frontal, bifrontal, frontolateral, and supraorbital keyhole approach. Many authors preferred orbital osteotomy in addition to the pterional approach. With further development of microsurgical and later endoscopic procedures, trans-sphenoidal route also gained favor.
High Route or Low Route: The high route or the transcranial route encompasses variations of the bifrontal, unifrontal, and pterional approaches with supraorbital keyhole approaches gaining ascendancy in recent years. The low route or the trans-sphenoidal route encompasses three variations—microsurgical (with its variations of sublabial, trans-rhinoseptal, and direct endo-nasal), endoscopic endo-nasal, and endoscopic-assisted microsurgical.
The salient features of transcranial surgical technique and trans-sphenoidal approach are summarized in Table 9.14
|
Author |
Patients/affected eyes |
Clinical presentation |
Resection |
Postop. visual status |
|---|---|---|---|---|
|
Margalit et al18 |
51 patients/100 eyes |
• Visual impairment – 66.7% • Headache –19.6% • Dizziness –2% • Incidental –21.6% |
GTR – 88.2% |
• Improvement – 40 eyes • Deterioration – 4 eyes |
|
Karsy et al24 |
49 patients |
• Visual deficit – 91.8% • Headache – 10.2% • Cranial nerve deficit – 0% • Cognitive deficit – 6.1% • Anosmia – 2% |
GTR – 71.25% |
|
|
Schick and Hassler2 |
53 patients |
• Visual impairment – 87% |
GTR – 90.5% |
• Improvement – 20 patients • Static – 25 patients • Deterioration – 7 patients |
|
Engelhardt et al15 |
20 patients |
• Visual impairment – 90% • Headache – 15% • Incidental – 10% |
GTR – 90% |
• Improvement – 14 patients • Static – 2 patients • Deterioration – 3 patients |
|
Li-Hua et al17 |
67 patients/134 eyes |
• Visual impairment – 100% • Headache – 47.76% • Behavior changes – 22.39% • Endocrinopathy – 4.5% • Seizure – 1.5% |
• Improvement – 87 eyes • Static – 39 eyes • Deterioration – 8 eyes |
|
|
Present study |
36 patients/72 eyes |
• Visual impairment – 88.9% • Headache – 50% • Behavior changes – 5.6% • Seizure – 2.8% |
GTR – 94.5% |
• Improvement – 31 eyes • Static – 35 eyes • Deterioration – 2 eyes |
|
Transcranial (the high route) |
Trans-sphenoidal (the low route) |
|
|---|---|---|
|
Salient features |
1. Craniotomy with shortest possible distance to the lesion. 2. Cerebrospinal fluid release (CSF) for brain relaxation. 3. Wide exposure with minimal brain retraction. 4. Early identification of the carotid and optic pathways. 5. Decompression of the bony optic canal 6. Coagulation of dural attachments, dissection of tumor from the surrounding structures and tumor resection. |
1. Adequate preparation of the anatomic corridor for expanded exposure of the anterior cranial base. 2. Early attack on the tumor base for devascularization and de-bulking. 3. Sub-dural, extra-arachnoid dissection 4. Meticulous reconstruction of osteo-dural defect. |
|
Approaches |
1. Pterional 2. Bifrontal 3. Frontolateral 4. Supra-orbital keyhole |
1. Trans-nasal microscopic 2. Endo-nasal endoscopic 3. Endoscope-assisted microsurgery |
|
Advantages |
1. Approach through the sterile corridor 2. Significantly low incidence of a. CSF Leak b. Infection c. Olfactory complications 3. Lesser tumor recurrence 4. Easier access to laterally extending tumors and more feasibility of Simpson Gr 1 resection |
1. Early devascularization of tumor 2. Better visual outcomes 3. Marginally lower endocrinopathies |
An important difference between transcranial and trans-sphenoidal techniques is that in the trans-sphenoidal technique, the intracranial pressure is paradoxically of assistance by facilitating the descent of the tumor in the field.
The High Route—Craniotomy: The surgical techniques of craniotomy along with its multiple variants, important among them being the pterional approach and the fronto-lateral approach have been well described by several authors.1 3 13 15 16 17 18 19 Like all skull base surgeries, surgery for tuberculum sella meningioma proceeds in three stages, viz., approach using an adequately wide exposure and drainage of cerebrospinal fluid (CSF) from basal cisterns, lamina terminalis, Sylvian and carotid cisterns and early control of blood supply, dissecting in the arachnoid plane and finally reconstruction.1
Another approach that has recently gained ascendancy is the supra-orbital keyhole approach. While the benefits of the approach include rapid access and cosmesis, it also has limitations of breaching the frontal sinus and difficult removal in case of extension over the planum sphenoidale.12
Nakamura et al compared the three classical trans-cranial approaches, viz., pterional, bifrontal, and fronto-lateral and found that while the outcomes including the extent of resection and visual outcome were not significantly different, the fronto-lateral approach provided the least invasive approach to the lesion.20
Side of approach: The traditional wisdom has been to approach the tumor from the side of poorer vision with the intent of preserving the vision in the better eye and in cases where tumor is in the midline, to approach it from the non-dominant side.3 17 18 19 On the contrary, several other authors have recommended that the approach be contralateral to the side of poorer vision, with the rationale being that better nerve may be less prone to insult due to manipulation on one hand, while minimal handling of the poorer nerve provides it with a better probability of recovery, on the other hand. In addition, it is the infero-medial portion of the tumor that causes the maximum visual compromise and is better removed without manipulating the nerve when approached contralaterally.15 16 However, in 2002, Fahlbusch and Schott reported approaching nearly all tumors from the right side, regardless of the extent and side of visual involvement (excepting cases where tumor had only left-sided extension).13 This allows more dexterous maneuvers by a right-handed surgeon on non-eloquent side, with the added benefit of lesser handling of the left nerve, should that be the worse one. In our series, we approached all patients from the right side, regardless of the side of poorer vision.
The Low Route—Trans-sphenoidal: Trans-sphenoidal techniques of removal of tuberculum sella meningiomas may be trans-sphenoidal microscopic, endo-nasal endoscopic, or endoscope-assisted microsurgery. The chief advantages that the trans-sphenoidal approaches present are lack of brain retraction, early devascularization of tumor supply, early bilateral optic nerve decompression, minimal handling of the optic nerve, and superior hypophyseal artery at the very end of tumor resection and better cosmesis.14 21 22 On the contrary, the trans-sphenoidal approach has its own fair share of limitations, which include the application of greater force on the surrounding structures in comparison with micro-instruments, difficult access in case of tumors with significant lateral extension, difficulty in achieving Simpson Grade I resection as it is difficult to resect the entire dural attachment, and postoperative CSF leak that has been reported to be as high as 20 to 30%.21
Outcomes
As the most common and debilitating clinical feature of tuberculum sella meningioma at presentation is visual deterioration, most of the series of tuberculum sella meningioma focus on visual outcomes.2 18 20 23 24 25 26 27 28 29
Visual diminution is the most common presenting complaint in most of the series and ranges from 65% to 100%. Visual improvement was seen postoperatively in nearly 50 to 87% of eyes in different series, and the vision remained static in 40 to 50% of eyes. A small number of eyes showed postoperative visual deterioration to the tune of 4 to 6% but has occasionally been reported to be as high as 25%.2 15 17 18 24 30
Pamir et al performed an analysis of multiple series to determine the factors that determine the outcome for tuberculum sella meningioma operated via the trans-cranial approach and found following to have significantly important bearing on the outcome—patient age, duration of visual symptoms, severity of visual symptoms, predominantly vertical growth potential, presence of significant peri-tumoral edema, presence of an intact arachnoid plane, and extensive removal.27
Postoperative Visual Deterioration: Postoperative visual deterioration is seen in 4 to 25% of the operated patients.2 15 17 18 24 30 The deterioration is usually immediate or early (a few hours to a few days) but may, on occasion, occur as late as 1 year after surgery.31 32 33
While the etiology of delayed deterioration is still unclear, direct mechanical and/or vascular injury is most commonly implicated in cases of immediate or early postoperative deterioration.3 13 14 20 33 34 35 Widespread vasospasm following skull base surgery is rare but known to occur and may be radiologically occult, especially insofar as small arteries such as the superior hypophyseal artery and chiasmatic perforators.33 36 37 38 This may be another cause of early deterioration and Santarius et al reported improvement in early deterioration after instillation of intra-arterial verapamil.33 Other factors that have been proposed include hypotension causing hypo-perfusion of already injured vasculature, focal factors such as optic pathway edema secondary to vascular or paracrine pathologies and re-perfusion injury to optic pathways.33
Comparison of outcomes and complications in Craniotomy vis-à-vis Trans-sphenoidal approach: Several authors have compared and contrasted the visual outcomes and complications of craniotomy and the trans-sphenoidal route.
Lu et al and Yang et al have conducted a comparative meta-analysis of trans-cranial and trans-sphenoidal series to quantify various outcomes and complication parameters comparing the two approaches.29 39 In their studies, it was found that
-
There was significantly lower incidence of CSF leak with the trans-cranial route with an odds ratio (OR) of 4.68, favoring the trans-cranial route.
-
There was significantly lower incidence of infection with the trans-cranial route with an OR of 2.36, favoring the trans-cranial route.
-
There was significantly lower incidence of olfactory complications with the trans-cranial route with an OR of 2.93, favoring the trans-cranial route.
-
Improvement in postoperative visual status was better with the trans-sphenoidal route with an OR of 3.93, favoring the trans-sphenoidal route.
-
There was marginally lower incidence of intracranial hemorrhage and endocrinopathies with the trans-sphenoidal route with an OR of 0.68 and 0.85 against trans-cranial route, while there was marginally lower incidence of tumor recurrence with the trans-cranial route with an OR of 1.02 favoring, the trans-cranial route.
The above conclusions are summarized in Fig. 2.
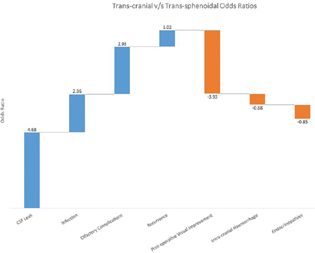
-
Fig. 2 Transcranial versus trans-sphenoidal odds ratio. CSF, cerebrospinal fluid.
Fig. 2 Transcranial versus trans-sphenoidal odds ratio. CSF, cerebrospinal fluid.
Treatment Strategy
Several authors have attempted to propound treatment strategies that best suit the resection of these tumors, taking into account various factors such as tumor characteristics, visual diminution, and surgeon's familiarity with the approach among others.
Magill et al have classified the tumor based on three parameters—size of tumor (<17 mm and ≥7 mm), invasion of the optic canal (≤ 3 mm, > 3 mm unilaterally, > 3 mm bilaterally), and arterial encasement (abutment, <180°, ≥ 180°).25
In contrast, Kuga et al have classified these tumors in three types (I-III) based on the size of the tumor and its relation to the optic chiasm and advocate the endoscopic approach for types I and II and the trans-cranial approach for type III. However, as the authors themselves note, the classification suffers from the drawback of evaluating the radiological features of the tumor only in the mid-sagittal plane.40
Schroeder has discussed in some depth about the choice of approach for tuberculum sella meningiomas.41 He emphasizes that in the endo-nasal route, discomfort to patient is more due to greater dissection in the nasal cavity compared with dissection in the trans-cranial route, chances of CSF leak, and consequent meningitis are higher and risk of loss of olfaction is greater and thus the preference should be the trans-cranial route, with endoscope-assistance, for all cases of tuberculum sella meningioma, except in cases where there is significant extension of the lesion in the nasal cavity or the lesion is midline, < 2 cm, and situated under a pre-fixed chiasm.41
Conclusion
Tuberculum sella meningiomas have significant debilitating potential for the patient, primarily due to the early and profound visual diminution. However, timely surgical intervention may help improve visual diminution significantly and may provide the patient with serviceable vision. In our experience, approaching the tumor from the right side, regardless of the side of the worse vision, does not significantly change the visual outcome. We also advocate the trans-cranial route over the endo-nasal route, as CSF leak, consequent meningitis, and potential life-threatening morbidities of it are significantly higher with the latter and not, in our opinion, justified when dealing with a histopathologically benign lesion.
Conflict of Interest
None declared.
Funding None.
References
- Surgical treatment of anterior basal meningiomas. J Neurooncol. 1996;29(3):239-248.
- [Google Scholar]
- Surgical management of tuberculum sellae meningiomas: involvement of the optic canal and visual outcome. J Neurol Neurosurg Psychiatry. 2005;76(7):977-983.
- [Google Scholar]
- Tuberculum sellae meningiomas: microsurgical anatomy and surgical technique. Neurosurgery. 2002;51(6):1432-1439. , discussion 1439–1440
- [Google Scholar]
- Anatomical origin of tuberculum sellae meningioma: off-midline location and its clinical implications. World Neurosurg. 2016;89:552-561.
- [Google Scholar]
- International statistical classification of diseases and related health problems, 10th revision, 2nd ed. Geneva: World Health Organization; 2004.
- [Google Scholar]
- The Chiasmal syndrome: of primary optic atrophy and bitemporal filed defects in adults with a normal sells Turtica. Arch Ophthalmol. 1930;3(6):704.
- [Google Scholar]
- Suprasellar meningiomas: the chiasmal syndrome. Springfield; 1938. p. :224-249. Eds. Meningiomas Their Classif. Reg. Behav. Life Hist. Surg. End Results. Charles C. Thomas:
- [Google Scholar]
- Tuberculum sellae meningioma: a report on management on the basis of a surgical experience with 70 patients. Neurosurgery. 2002;51(6):1358-1363. , discussion 1363–1364
- [Google Scholar]
- Tuberculum sella meningioma. Otolaryngol Clin North Am. 2011;44(4):953-963. , viii–ix
- [Google Scholar]
- Pterional surgery of meningiomas of the tuberculum sellae and planum sphenoidale: surgical results with special consideration of ophthalmological and endocrinological outcomes. J Neurosurg. 2002;96(2):235-243.
- [Google Scholar]
- Tuberculum sellae meningiomas: high route or low route? A series of 51 consecutive cases. Neurosurgery. 2008;62(3):556-563. , discussion 556–563
- [Google Scholar]
- Contralateral transcranial approach to tuberculum sellae meningiomas: long-term visual outcomes and recurrence rates. World Neurosurg. 2018;116:e1066-e1074.
- [Google Scholar]
- The contralateral subfrontal approach can simplify surgery and provide favorable visual outcome in tuberculum sellae meningiomas. Neurosurg Rev. 2012;35(4):601-607. , discussion 607–608
- [Google Scholar]
- Microsurgical management of tuberculum sellae meningiomas by the frontolateral approach: surgical technique and visual outcome. Clin Neurol Neurosurg. 2011;113(1):39-47.
- [Google Scholar]
- Tuberculum sellae meningiomas: surgical technique, visual outcome, and prognostic factors in 51 cases. J Neurol Surg B Skull Base. 2013;74(4):247-258.
- [Google Scholar]
- Technical nuances in the management of tuberculum sellae and diaphragma sellae meningiomas. Neurosurg Focus. 2013;35(6):E7.
- [Google Scholar]
- Tuberculum sellae meningiomas: clinical outcome considering different surgical approaches. Neurosurgery. 2006;59(5):1019-1028. , discussion 1028–1029
- [Google Scholar]
- Nonsurgical management of small and intracanalicular acoustic tumors. Neurosurgery. 1985;16(6):801-803.
- [Google Scholar]
- Endoscopic endonasal approach for removal of tuberculum sellae meningiomas. Neurosurg Clin N Am. 2015;26(3):349-361.
- [Google Scholar]
- Surgical outcome of tuberculum sellae and planum sphenoidale meningiomas based on Sekhar-Mortazavi tumor classification. J Neurosurg Sci. 2021;65(2):190-199.
- [Google Scholar]
- Clinical outcomes with transcranial resection of the tuberculum sellae meningioma. World Neurosurg. 2017;108:748-755.
- [Google Scholar]
- Tuberculum sellae meningiomas: grading scale to assess surgical outcomes using the transcranial versus transsphenoidal approach. Neurosurg Focus. 2018;44(4):E9.
- [Google Scholar]
- Visual outcome of tuberculum sellae meningiomas after extradural optic nerve decompression. Neurosurgery. 2006;59(3):570-576. , discussion 570–576
- [Google Scholar]
- Outcome determinants of pterional surgery for tuberculum sellae meningiomas. Acta Neurochir (Wien). 2005;147(11):1121-1130. , discussion 1130
- [Google Scholar]
- Clinical outcomes of tuberculum sellae meningiomas focusing on reversibility of postoperative visual function. Acta Neurochir (Wien). 2013;155(1):25-31.
- [Google Scholar]
- Transsphenoidal versus transcranial approach for treatment of tuberculum sellae meningiomas: a systematic review and meta-analysis of comparative studies. Sci Rep. 2019;9(1):4882.
- [Google Scholar]
- Tuberculum Sellae Meningiomas.Al-Meftys Meningiomas, 2nd ed. New York: Thieme Medical; 2011. p. :206-213. In: eds.
- [Google Scholar]
- Visual recovery following optic nerve decompression for chronic compressive neuropathy. Acta Neurochir (Wien). 2009;151(4):325-334.
- [Google Scholar]
- Visual outcome in surgically treated suprasellar meningiomas. J Neuroophthalmol. 2003;23(1):3-10.
- [Google Scholar]
- Delayed neurological deficit following resection of tuberculum sellae meningioma: report of two cases, one with permanent and one with reversible visual impairment. Acta Neurochir (Wien). 2014;156(6):1099-1102.
- [Google Scholar]
- Microsurgical removal of suprasellar meningiomas. Neurosurgery. 1985;16(3):364-372.
- [Google Scholar]
- Tuberculum sellae meningiomas: functional outcome in a consecutive series treated microsurgically. Surg Neurol. 2006;66(1):37-44. , discussion 44–45
- [Google Scholar]
- Vasospasm after resection of skull base tumors. Acta Neurochir (Wien). 1995;132:53-58. (1–3):
- [Google Scholar]
- Vasospasm after cranial base tumor resection: pathogenesis, diagnosis, and therapy. Surg Neurol. 1999;52(6):577-583. , discussion 583–584
- [Google Scholar]
- Delayed vasospasm after removal of a skull base meningioma. J Neurol Surg A Cent Eur Neurosurg. 2012;73(4):249-252.
- [Google Scholar]
- Olfactory groove and tuberculum sellae meningioma resection by endoscopic endonasal approach versus transcranial approach: A systematic review and meta-analysis of comparative studies. Clin Neurol Neurosurg. 2018;174:13-20.
- [Google Scholar]
- Treatment strategy for tuberculum sellae meningiomas based on a preoperative radiological assessment. World Neurosurg. 2018;120:e1279-e1288.
- [Google Scholar]
- Indications and limitations of the endoscopic endonasal approach for anterior cranial base meningiomas. World Neurosurg. 2014;82:S81-S85. (6, Suppl)
- [Google Scholar]







