Translate this page into:
Contiguous-Level Unilateral Cervical Spine Facet Dislocation—A Report of a Less Discussed Subtype
Arunkumar Sekar, MCh Department of Neurosurgery, All India Institute of Medical Sciences Bhubaneswar, Odisha 751019 India neurosurg_arun@aiimsbhubaneswar.edu.in arunkumar3002@hotmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Unilateral facet dislocation of subaxial cervical spine trauma is characterized by dislocation of inferior facet of superior vertebra over the superior facet of inferior vertebra. The injury is due to high-velocity trauma and associated with instability of spinal column. Such unilateral facet dislocations occurring at multiple adjacent levels for some reason are not reported or studied frequently. We have reported two cases of multiple-level dislocation of unilateral facets managed in our hospital with a review of available literature. The injury occurs as one side of the motion segment translates and rotates around an intact facet on the contralateral side. The major mechanism of injury is distractive flexion injury with axial rotation component. The injury is associated with instability secondary to loss of the discoligamentous complex. In cases with multiple-level dislocations of unilateral cervical facets, there are multiple mechanisms associated with significant neurological injury and most of them succumb at the site of injury. Only three other cases are available in English language literature. The neurological outcome is invariably poor. Multiple-level facet dislocations of subaxial cervical spine are reported sparsely in literature. We suspect that due to high-velocity nature of these injuries, most of them succumb soon after injury and not often reported. This article reports two cases of contiguous-level unilateral facet dislocation of subaxial cervical spine with associated injuries and the outcomes with review of literature.
Keywords
subaxial cervical spine injury
traumatic spine injury
multiple-level facet dislocation
Introduction
Unilateral facet dislocation is a subset of subaxial cervical spine injury secondary to high-velocity trauma. They are characterized by dislocation of inferior facet of superior vertebra over the superior facet of inferior vertebra as one side of the motion segment translates and rotates around an undislocated facet on the contralateral side.1 They account for ∼4 to 16% of cervical spine injuries. They usually occur secondary to distraction flexion injury with an element of rotation.1 2 Contiguous/adjacent levels of unilateral facet dislocations have rarely been reported in the literature. We present two such cases and the difficulties involved in the management with a brief review of the literature.
Case 1
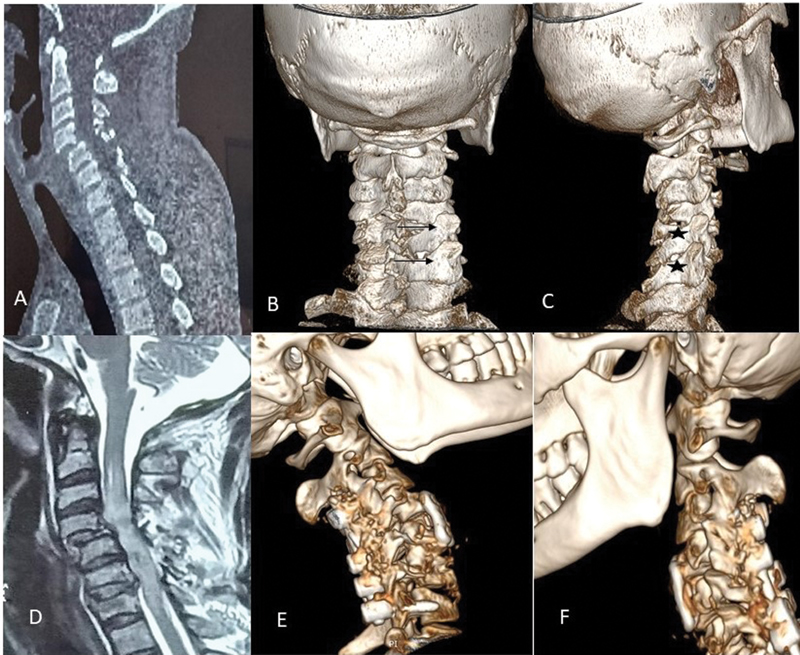
A 30-year-old truck driver presented with American Spinal Injury Association Score (ASIA)-A cervical spine injury C4 below after a high-speed motor vehicle accident. He was in neurogenic shock with persistent bradycardia and hypotension and poor respiratory efforts. His computed tomography (CT) of cervical region scan showed grade II anterolisthesis of C4 over C5, fracture of left C4 lamina with unilaterally locked facet of right-sided C4 to C5, C5 to C6 (Fig. 1A–C). Magnetic resonance imaging (MRI) of cervical spine showed C4 to C5 anterolisthesis along with extensive cord contusion and edema extending from C2 to C7 and mild cord compression anteriorly at C4 to C5 level due to prolapsed disc (Fig. 1D). The dislocation was irreducible with traction.
-
Fig. 1 (A) Grade II anterolisthesis of C4 over C5 with teardrop fractures of C7, (B) fracture of left C5/6 lamina (arrows), (C) unilateral locked facet of right-sided C4–C5, C5–C6 (asterisks), (D) magnetic resonance imaging extensive cord contusion and edema extending from C2 to C7 with associated listhesis, (E and F) postoperative three-dimensional reconstruction of computed tomography C-spine after anterior and posterior fixation.
Fig. 1 (A) Grade II anterolisthesis of C4 over C5 with teardrop fractures of C7, (B) fracture of left C5/6 lamina (arrows), (C) unilateral locked facet of right-sided C4–C5, C5–C6 (asterisks), (D) magnetic resonance imaging extensive cord contusion and edema extending from C2 to C7 with associated listhesis, (E and F) postoperative three-dimensional reconstruction of computed tomography C-spine after anterior and posterior fixation.
He underwent combined anterior and posterior fixation of cervical spine in staged manner in view of his labile hemodynamic status. Due to prolapsed C4/5 intervertebral disc, anterior fixation was planned for that level followed by posterior reduction and fixation from C4 to C7. Intraoperatively, there was clear disruption of the disc and posterior longitudinal ligament at C4/5 level. On posterior approach, there was associated fracture of C5 and C6 lamina with locked and disconnected right C6 lateral mass due to fracture of C6 pedicle. He underwent decompression and fixation posteriorly (Fig. 1E, F). On follow-up, at about 1 month his neurology remained the same despite a stable 360-degree construct.
Case 2
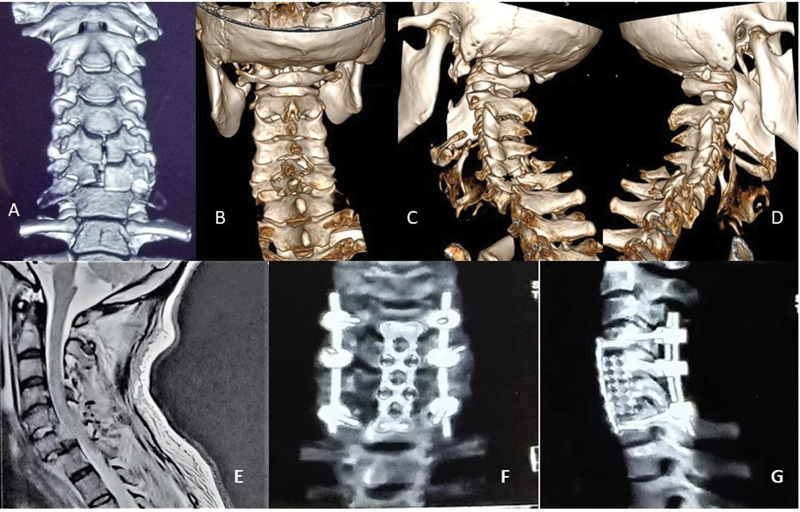
A 42-year-old patient presented with a history of fall from 15 feet height. He had weakness of both upper limbs and paralysis of both lower limbs with absent sensation below T4 and absent bulbocavernosus reflex. CT of cervical spine showed grade III anterolisthesis of C6 to C7, with midline compression burst fracture of C5 and C6 body along with locked facets of right-sided C5/C6 and left C6/C7(Fig. 2A–D). MRI of cervical spine showed C6/C7 listhesis along with cord compression at C6 to 7 level with cord contusion and edema (Fig. 2E). He had developed hemodynamic instability that needed inotrope for stabilization.
-
Fig. 2 (A–D) Computed tomography of the cervical spine showed grade III anterolisthesis of C6 over C7, with sagittally split fracture of C5 and C6 body along with locked facet of right-sided C5 to C6 and left C6 to C7 (asterisk). (E) T2-weighted magnetic resonance imaging sagittal of the cervical spine shoeing listhesis of C6 over C7 with cord edema from C4 to C7. (F, G) Postoperative three-dimensional reconstruction with anterior and posterior fixation.
Fig. 2 (A–D) Computed tomography of the cervical spine showed grade III anterolisthesis of C6 over C7, with sagittally split fracture of C5 and C6 body along with locked facet of right-sided C5 to C6 and left C6 to C7 (asterisk). (E) T2-weighted magnetic resonance imaging sagittal of the cervical spine shoeing listhesis of C6 over C7 with cord edema from C4 to C7. (F, G) Postoperative three-dimensional reconstruction with anterior and posterior fixation.
He underwent combined anterior and posterior fusion in single stage. Initially on posterior approach, decompression and fixation were done using pedicle screws at C4/C7 and lateral mass screws at C5/6 level. The main rotational movement was focused at C6 vertebra with superior facet of C6 locked over adjacent C5 facet on the right and inferior facet of C6 locked over C7 facet on the left. Anteriorly, the construct was completed with a C5/6 corpectomy with mesh cage and fixed with plates and screws (Fig. 2F, G). Postoperatively, he gradually stabilized with continuing rehabilitation.
Discussion
Injuries to the subaxial cervical facets causing dislocation with or without fracture are due to complex flexion and distraction forces with accompanying element of axial rotation. They are associated with significant neurological deficits with tetraplegia reported in as high as 87% of cases.3 These injuries are usually associated with high-speed injuries and severe neurological deficits.4 Allen et al conceptualized the effects of dynamic loading along an established vector in relation to the position of the spine at the time of impact into different mechanisms of injury. This has helped in extrapolating the mechanisms into real-life scenarios.5 The motion associated with distractive flexion stages (DFS) can create a spectrum of facet injuries depending on the extent of the deformational forces injuries.6 7 The spectrum ranges from DFS1 in which there is facet subluxation, DFS2—unilateral facet dislocation, DFS3 and 4 with bilateral facet dislocation and body displacement of less or more than 50%.8 In case of unilateral facet dislocation, the incidence of neurological deficit is up to 37% of cases. The distraction flexion mechanism is frequently associated with secondary compressive lesions in the lower levels.9 When DFS2 variety is associated with neurological injury, the posterior ligamentous complex is significantly compromised. Usually, these facet dislocations are focused around lower cervical region due to more horizontally oriented facets in these levels.10 About 19% of cases have associated floating lateral mass depending on the severity of injury.11 However, despite all these combinations of injuries that can occur in distraction flexion injury, only few cases regarding multiple contiguous levels unilateral facet dislocations are reported in English literature.
Eismont et al12 reported a case with ASIA-A spinal injury due to diving. He had a unilateral facet dislocation at C6/7 level with bilateral dislocations at C5/6 level. He underwent posterior fixation, but his neurology remained the same at 2 years follow-up.
A second report from Bourghli et al13 was about a 52-year-old patient with hang-gliding injury. He had incomplete tetraplegia. His imaging revealed unilateral C3/4 with bilateral C4/5 injury with associated sagittal split fracture at C5 level. He underwent anterior decompression and fusion at the involved levels. He had improvement with good clinical and radiological outcomes.
Zemmar et al14 reported a patient with ASIA-A injury following a fall from height. He had sustained bilateral facets dislocations at C6/7 and C7/T1 levels and underwent posterior reduction and fixation. He, however, remained in the same neurology.
The most recent report by Agrawal et al15 presented a case of fall injury with C4/5 and C6/7 grade III subluxation with complete spinal cord injury. He underwent posterior reduction and fixation. Patient continued rehabilitation without any clinical improvement.
In our case report like other previous case reports, the common features are high-velocity injuries. Both patients had sustained complete spinal cord injury. There were other associated secondary injury combinations as proposed by the mechanistic classification. In first case, the primary injury is DFS2 at C4/5 and C5/6 with associated anterior inferior compression fracture of C5/C6 and C7 vertebra. There was associated C6 right pedicle fracture. In second case along with DFS2 injury at C5/6, there was associated vertical compression loading in the lower level. Three-dimensional reconstruction images had significantly contributed to the understanding of the extent of injury and preoperative planning. Both patients had a stormy perioperative course due to associated hemodynamic instability. Despite many cervical spine injuries seen worldwide, it is surprising to see only small number of contiguous-level unilateral facet dislocations in literature. We suspect it may be the serious nature of the injury leading to prehospital mortality and fewer cases presenting for treatment.
Conclusion
Contiguous-level unilateral facet dislocations are rare high-velocity subaxial cervical spine injuries. Multiple secondary mechanisms like compressive and axial loading are associated with primary distractive flexion injury with a significant rotational component. Identifying these contiguous-level subluxations is important as they are highly unstable injuries requiring a rigid construct. Usually, they present with complete spinal cord injury with poor neurological outcomes. More of this subset of injuries needs to be studied to understand their outcomes.
Conflict of Interest
None declared.
Funding None.
References
- Unilateral facet dislocations and fracture-dislocations of the cervical spine. J Bone Joint Surg Br. 1991;73(6):977-981.
- [Google Scholar]
- Traumatic subaxial cervical facet subluxation and dislocation: epidemiology, radiographic analyses, and risk factors for spinal cord injury. Spine J. 2018;18(3):387-398.
- [Google Scholar]
- The impact of facet dislocation on clinical outcomes after cervical spinal cord injury: results of a multicenter North American prospective cohort study. Spine. 2013;38(2):97-103.
- [Google Scholar]
- Subaxial cervical spine injury classification systems. Neurosurgery. 2013;72(02):170-186.
- [Google Scholar]
- Distractive flexion injuries of the subaxial cervical spine treated with anterior plate alone. J Spinal Disord Tech. 2004;17(1):1-7.
- [Google Scholar]
- Mechanical patterns of cervical injury influence postoperative neurological outcome: a verification of the Allen system. Spine. 2011;36(6):E441-E446.
- [Google Scholar]
- A mechanistic classification of closed, indirect fractures and dislocations of the lower cervical spine. Spine. 1982;7(1):1-27.
- [Google Scholar]
- Hyperflexion Sprain of the Cervical Spine. Cervical Spine II . Springer Vienna; 1989. p. :12-17. In:
- [Google Scholar]
- Clinical outcomes of 90 isolated unilateral facet fractures, subluxations, and dislocations treated surgically and nonoperatively. Spine. 2007;32(26):3007-3013.
- [Google Scholar]
- Anterior fusion for rotationally unstable cervical spine fractures. Spine. 2000;25(16):2028-2034.
- [Google Scholar]
- Complete dislocations at two adjacent levels of the cervical spine. A case report. Spine. 1984;9(3):319-322.
- [Google Scholar]
- Two adjacent levels dislocation of the cervical spine managed Viaan anterior only approach: a case report. J Med Liban. 2016;64(3):181-185.
- [Google Scholar]
- Bilateral cervical facet dislocations at two adjacent levels: a case report. Surg Neurol Int. 2019;10(48):48.
- [Google Scholar]
- Noncontiguous two levels traumatic dislocation of the cervical spine managed with a posterior only approach. J Orthop Spine. 2019;7(2):80.
- [Google Scholar]







