Translate this page into:
Conservative treatment in hemifacial spasm due to vertebrobasilar dolichoectasia
*Corresponding author: Yudhi Adrianto, Department of Neurology, Airlangga University Faculty of Medicine, Airlangga University Hospital, Surabaya, Indonesia. yudhi_neuro@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Supit VD, Adrianto Y, Setyowatie S. Conservative treatment in hemifacial spasm due to vertebrobasilar dolichoectasia. J Neurosci Rural Pract. 2024;15:390-2. doi: 10.25259/JNRP_41_2024
Abstract
Primary or secondary hemifacial spasm (HFS) can be caused by a variety of conditions, one of which is caused by neurovascular contact with a vertebrobasilar dolichoectasia (VBD). Microvascular decompression (MVD) had been known for the treatment of neurovascular contact that gives best outcome, however there were still limitations which surgery cannot be performed. In that case, conservative treatment plays essential role. Our case reported A 69-year-old man with chief complaint right HFS for four years that getting better with conservative treatment (blood pressure management and clonazepam oral).
Keywords
Vertebrobasilar dolichoectasia
Hemifacial spasm
Facial nerve compression
Conservative treatment
Neurovascular contact
INTRODUCTION
Various studies have shown prevalence rates of vertebrobasilar dolichoectasia (VBD) which range from 7.6% to 18%. The most common segment involved is the vertebrobasilar segment[1] VBD, which may be asymptomatic or symptomatic, is characterized by elongation and dilation of the vertebrobasilar arteries. The VBD patients are at high risk of vascular events and structural compression.[2]
Hemifacial spasm (HFS) is a condition featuring unilateral involuntary spasms, brief or persistent, of the facial muscles. Despite a lack of pain, HFS symptoms can be both physically and psychologically devastating. The HFS can be either primary or secondary, with one cause being facial nerve compression by aberrant blood vessels.[3,4]
Microvascular decompression (MVD) is proven to be an effective management of HFS caused by VBD. However, there are limitations to which surgery cannot be performed such as facility and operator availability or patients with a high-risk profile for surgery. In this case, we present a patient with HFS caused by VBD that significantly gets better using conservative treatments.
CASE REPORT
A 69-year-old man with a four-year history of right HFS, getting worse when the patient wakes up in the morning and does exercises. The HFS diminished when the patient rested and disappeared during sleep. The other symptoms such as headache, tinnitus, diplopia, facial pain, and paresis in extremities were all denied. He had no family history of symptoms like this. The patient has a history of diabetes mellitus, hypertension, and chronic kidney disease. The patient has been smoking for 20 years one pack a day.
Upon first evaluation, the patient presented with hypertension (160 mmHg systolic and 100 mmHg diastolic) and was not on any antihypertensive medication. Neurological examination showed ipsilateral, involuntary, paroxysmal contraction of the facial muscles on the right side. Other remaining cranial nerves did not reveal any abnormalities. Magnetic resonance angiography (MRA) shows the vertebrobasilar dolichoectasia [Figure 1] with the height of bifurcation indented and elevated at the floor of the third ventricle [Figures 2a and b], and MRI FIESTA shows neurovascular contact with the right facial nerve [Figure 2c]. Based on the smoker’s criteria, this patient was diagnosed with dolichoectasia of the vertebrobasilar artery.
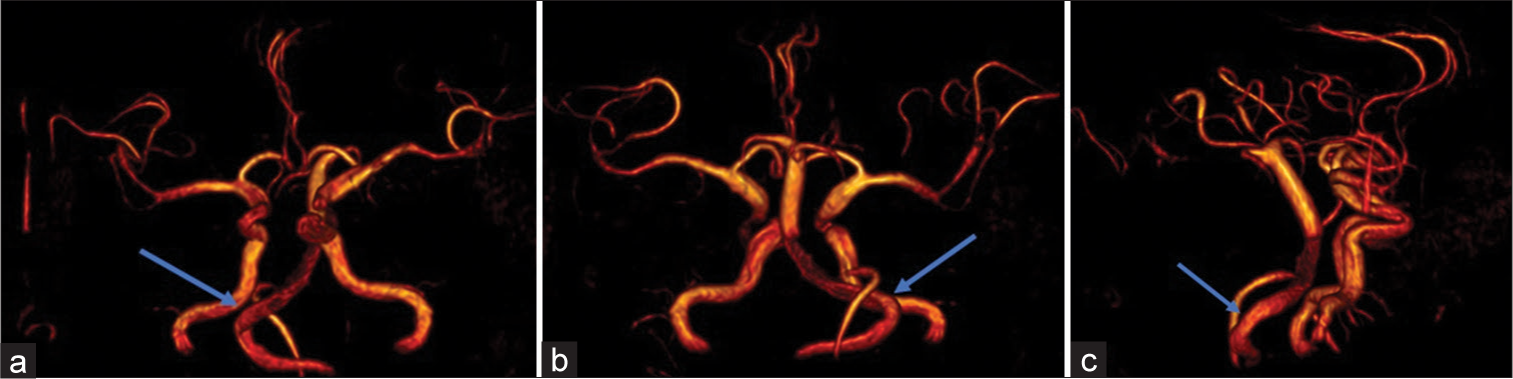
- Three-dimensional volume rendering of magnetic resonance imaging (a) anterior view, (b) posterior view, (c) right lateral view shows vertebrobasilar dolichoectasia (blue arrows).

- (a) Magnetic resonance imaging (MRI) T2 sagittal view shows vertebrobasilar dolichoectasia (blue arrow). (b) Magnetic resonance angiography time of flight shows bifurcation of the basilar artery indenting and elevating at the floor of the third ventricle (blue arrow). (c) MRI FIESTA shows neurovascular contact with the right facial nerve (blue arrows).
The patient was referred to a neurosurgeon for MVD; however, the patient declined the surgery. The patient received clonazepam 1 mg once daily to control HFS and amlodipine 10 mg once daily to control hypertension. After one month of follow-up, HFS had significantly reduced, and BP had been controlled.
DISCUSSION
Patients with VBD are at high risk for neurological deterioration. Clinical manifestations can be divided into compressive symptoms and vascular events. The most common vascular event is ischemic stroke.[2] Compressive symptoms in VBD are caused by an enlarged vessel exerting pressure on surrounding structures, including cranial nerves. The HFS is one of the common results of compressive symptoms due to neurovascular contact with the facial nerve. The HFS must be distinguished from partial motor seizures because of differences in etiology and treatment. The HFS tends to resolve with rest or sleep. Electroencephalography may be used as a tool to differentiate these two.[3,4] Other symptoms depend on which cranial nerves are compressed.[5]
Even though VBD may remain asymptomatic, VBD may be progressive and may influence the likelihood of various complications. The VBD is related to both hemodynamic and anatomical factors. Therefore, vasculopathy risk factors might contribute to the prognosis and clinical events of VBD. Studies have shown a relationship between VBD with older age and hypertension, resulting in arteriopathy. Aging causes a decrease in elasticity and thickening of the vessel wall. High BP increases pulsatility and atherosclerosis in the blood vessels, thus leading to vascular expansion, elongation, and bending of the vascular.[1] The VBD can be diagnosed using several imaging modalities such as digital subtraction angiography (DSA), computed tomography angiography, and magnetic resonance imaging (MRI)-MRA.[5] The MRI-MRA played an essential part in the work-up for HFS to look up for any vascular contact with the facial nerve. Its advantages over computed tomography and cerebral angiography are its non-invasiveness and its ability to demonstrate vascular compression against the facial nerve.[3]
Treatment options for HFS caused by VBD are conservative or surgical management. Despite good surgical outcomes for HFS due to VBD, MVD is surgically challenging and increases the risk of ischemic injury.[2] For conservative treatment, some studies have reported that clonazepam could be effective in managing HFS.[6] The BP management also plays a significant role in the management of HFS caused by VBD contact with facial nerve and prevents the incidence of vascular events. This case report faced notable limitations, inability to perform DSA due to poor renal function, and unexplored alternative HFS treatments. Further research is required to determine which patients need surgery for MVD or conservative treatment alone can successfully treat the patient.
CONCLUSION
The patient with HFS should be considered for neurovascular contact with the facial nerve. The MRI-MRA is a good diagnostic tool to evaluate neurovascular contact and vascular abnormalities. Conservative management of HFS caused by VBD should be considered compared to surgical MVD, especially in the elderly or in patients with high-risk surgical profiles. The BP management and benzodiazepine medication are some of the keys in managing HFS caused by VBD.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consents.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Prevalence and clinical correlates of intracranial dolichoectasia in individuals with ischemic stroke. Stroke. 2021;52:2311-8.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical course and treatment of vertebrobasilar dolichoectasia: A systematic review of the literature. Neurol Res. 2013;35:131-7.
- [CrossRef] [PubMed] [Google Scholar]
- Hemifacial spasm resulting from vertebral artery dolichoectasia. Neurosci J. 2005;10:304-6.
- [Google Scholar]
- Hemifacial spasm: The past, present and future. J Neurol Sci. 2015;356:27-31.
- [CrossRef] [PubMed] [Google Scholar]
- Multimodality imaging of vertebrobasilar dolichoectasia: Clinical presentations and imaging spectrum. Radiographics. 2016;36:1129-46.
- [CrossRef] [PubMed] [Google Scholar]
- Safety and efficacy of clonazepam in patients with hemifacial spasm: A double-blind, randomized, placebo-controlled trial. Parkinsonism Relat Disord. 2022;103:1-6.
- [CrossRef] [PubMed] [Google Scholar]







