Translate this page into:
Concurrent Venous Stenting of the Transverse and Occipito-Marginal Sinuses: An Analogy with Parallel Hemodynamic Circuits
Address for correspondence: Dr. Thomas J. Buell, Department of Neurosurgery, University of Virginia Health System, Box: 800212, Charlottesville, Virginia 22908, USA. E-mail: tjb4p@hscmail.mcc.virginia.edu
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Nonthrombotic intracranial venous occlusive disease (NIVOD) has been implicated in the pathophysiology of idiopathic intracranial hypertension (IIH) and various non-IIH headache syndromes. Endovascular stenting of stenotic, dominant transverse sinuses (TSs) may reduce trans-stenosis pressure gradients, decrease intracranial pressure, and alleviate symptoms in a subset of NIVOD patients. We present a case in which concurrent stenting of the occipito-marginal sinus obliterated the residual trans-stenosis pressure gradient across an initially stented dominant TS. We hypothesize that this observation may be explained using an electric-hydraulic analogy, and that this patient's dominant TS and occipito-marginal sinus may be modeled as a parallel hemodynamic circuit. Neurointerventionalists should be aware of parallel hemodynamic drainage patterns and consider manometry and possibly additional stenting of stenotic, parallel venous outflow pathways if TS stenting alone fails to obliterate the trans-stenosis pressure gradient.
Keywords
Endovascular outcomes
intracranial stent
stenosis
venous sinus
INTRODUCTION
Nonthrombotic intracranial venous occlusive disease (NIVOD) has been posited to have a role in the pathophysiology of idiopathic intracranial hypertension (IIH), as well as various non-IIH headache syndromes.[1234567] In a subset of NIVOD patients with venous sinus stenosis and an associated trans-stenosis pressure gradient, endovascular treatment with venous sinus stenting (VSS) may provide symptomatic relief.[3789] The distal transverse sinus (TS) is the most common site of venous stenosis in NIVOD, and stenting of the dominant TS can be effective in appropriately selected patients.[10] However, if the stenotic TS exists within a parallel hemodynamic circuit, stenting of the affected TS alone may be insufficient to abolish the trans-stenosis venous pressure gradient. We present a NIVOD patient with cerebral venous drainage through a parallel hemodynamic circuit involving stenotic transverse and occipito-marginal sinuses. VSS of both parallel sinuses was necessary to completely obliterate their trans-stenosis pressure gradients.
CASE REPORT
A 34-year-old female with a history of a repaired lumbar myelomeningocele, subsequent cord de-tethering, and shunted hydrocephalus presented with medication-refractory headaches and right-sided, pulse-synchronous tinnitus.
Investigations
Neuroimaging was negative for overt shunt malfunction, but revealed a hypoplastic left TS and stenosis of the dominant right TS. The patient underwent catheter cerebral angiography and venous manometry, which confirmed the presence of a dominant right TS, but also revealed significant venous drainage through the occipital and left marginal sinuses (left occipito-marginal sinus). Both the right TS and left occipito-marginal sinus were found to be radiographically and physiologically stenotic, with associated trans-stenosis pressure gradients of 8 mmHg each [Figure 1].
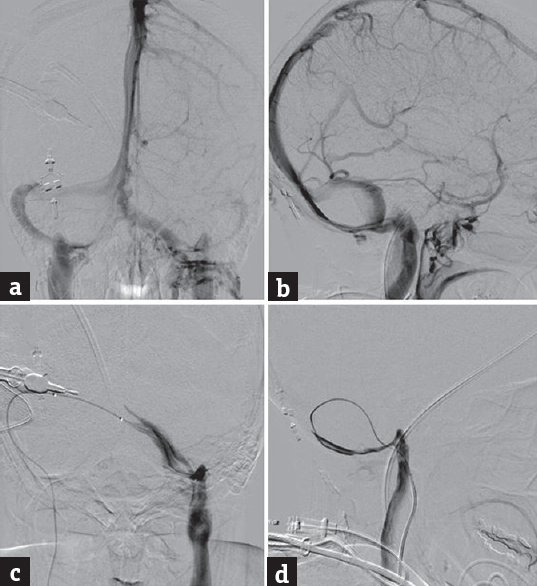
- Catheter cerebral angiography and venous manometry were performed. The venous phase of an internal carotid artery injection showed a dominant right transverse sinus, but also left greater than right occipito-marginal sinus drainage on anteroposterior (a) and lateral (b) views. (c and d) an occipital sinus injection on anteroposterior and lateral views, respectively. Both the right transverse and left marginal sinuses appeared stenotic and were associated with focal pressure gradients of 8 mmHg
Treatment
The next day, we performed VSS and balloon angioplasty of the right TS and left occipito-marginal sinus. First, we deployed a Zilver® 8 mm × 60 mm self-expanding stent (Cook Medical, Bloomington, IN, USA) into the right TS, which reduced the trans-stenosis pressure gradient to 4 mmHg [Figure 2a and b]. Since a residual pressure gradient remained after TS stenting, we then deployed a second Zilver 8 mm × 80 mm stent into the left occipito-marginal sinus. Concurrent stenting of the right TS and left occipito-marginal sinus completely abolished both trans-stenosis pressure gradients [Figure 2c and d].
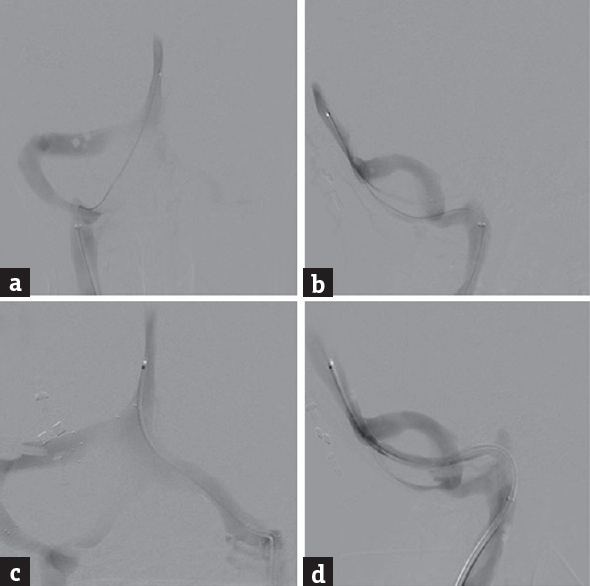
- We performed balloon angioplasty and endovascular stenting of the right transverse sinus and left occipito-marginal sinus. Initially, we deployed a Zilver® 8 mm × 60 mm self-expanding stent (Cook Medical, Bloomington, IN, USA) into the right transverse sinus, and the trans-stenosis pressure gradient decreased by 50%. Due to a residual 4 mmHg pressure gradient, we then deployed a Zilver 8 mm × 80 mm stent into the left occipito-marginal sinus. Both trans-stenosis pressure gradients were completely abolished after concurrent stenting of the right transverse sinus and left occipito-marginal sinus. Note the improved luminal caliber of the right transverse sinus (a and b) and left occipito-marginal sinus (c and d) on poststent imaging
Outcome and follow-up
After VSS, the patient's preoperative symptoms of headaches and tinnitus immediately improved, and she was discharged home on postoperative day 1 in good condition. Evaluation of the patient's pre- and post-VSS symptoms using the Headache Impact Test-6, Tinnitus Handicap Inventory, and the 36-Item Short Form Health Survey (SF-36) quality of life questionnaire showed quantitative improvement at 4-week follow-up [Table 1].[111213] The patient reported continued symptom improvement at the last clinic follow-up 3 months after stenting.
| Pre-VSS | Post-VSS (4 weeks) | |
|---|---|---|
| HIT-6 | 69 (severe impact on QOL) | 46 (little to no impact on QOL) |
| THI | 46 (grade 3; moderate) | 32 (grade 2; mild) |
| SF-36 QOL | ||
| Physical functioning | 20±25.8 | 50±40.8 |
| Role limitations due to physical health | 0 | 100±50 |
| Role limitations due to emotional problems | 0 | 100±0 |
| Energy/fatigue | 0 | 55±34.2 |
| Emotional well-being | 24±16.7 | 60±37.4 |
| Social functioning | 0 | 62.5±17.7 |
| Pain | 0 | 57.5±24.7 |
| General health | 10±13.7 | 25±17.7 |
SF-36 scores reported as mean±SD, with higher scores indicating less disability. HIT-6: Headache Impact Test-6, THI: Tinnitus Handicap Inventory, VSS: Venous sinus stenting; QOL: Quality of life, SF-36: 36-Item Short Form Health Survey, SD: Standard deviation
DISCUSSION
VSS may be an effective treatment for a subset of NIVOD patients with various headache syndromes.[171415161718] Indications for VSS include focal stenosis of a dominant TS that is associated with an elevated trans-stenosis pressure gradient.[11920] Neurointerventionalists have used 8 mmHg as a minimum trans-stenosis gradient prior to VSS;[12122] however, some patients may still benefit from endovascular treatment of lower gradients.[8]
The goal of VSS is to relieve the trans-stenosis pressure gradient by increasing the luminal diameter of the affected sinus.[9] From Hagen–Poiseuille's law, increasing the radius of a stenotic segment will decrease the trans-stenosis pressure gradient by an exponential factor of 4.[2324] In many patients, deployment of a single, appropriately sized stent into a stenotic, dominant TS is sufficient to obliterate the pressure gradient.[9] However, we previously identified a subset of patients with primary stenosis of the posterior superior sagittal sinus (S1 segment) who may also benefit from longer constructs comprising multiple stents.[8] In these patients, two or more stents were deployed in series, spanning the S1 superior sagittal sinus and TS.[8] When stent-adjacent stenosis occurs after initial TS stenting, other authors have also deployed stents in series spanning the TS and S1 superior sagittal sinus.[2526] In this case report, we present a unique scenario in which stents were deployed in a parallel configuration.
The electric-hydraulic circuit analogy is conceptually useful for understanding how additional stenting of the occipito-marginal sinus could decrease the trans-stenosis pressure gradient of the TS.[24] From the electric-hydraulic circuit analogy, stenotic segments of hydraulic channels can be thought of as electrical resistors [Figure 3].[24] In both types of circuits, potential energy is equivalent across parallel segments: voltages for electrical resistors and pressure gradients for stenotic hydraulic channels.[24] Our patient's main intracranial venous drainage pathways were the right TS and left occipito-marginal sinus, and we hypothesize that these sinuses can be modeled as a parallel hemodynamic circuit. The patient's TS and occipito-marginal sinus both had trans-stenosis pressure gradients of 8 mmHg based on preoperative venous manometry. Stenting the TS reduced trans-stenosis pressure gradients of both the TS and occipito-marginal sinus to 4 mmHg, which could be explained by their parallel configuration. The TS stent appeared widely patent without waist deformity or contrast stasis; therefore, we decided to stent the left occipito-marginal sinus, which completely abolished both trans-stenosis pressure gradients.
![The electric-hydraulic circuit analogy is conceptually useful for understanding how additional occipito-marginal sinus stenting decreased the trans-stenosis pressure gradient of the transverse sinus.[24] In this analogy, stenotic segments of hydraulic channels can be thought of as electrical resistors. In both circuits, potential energy is equivalent when in parallel configuration: voltages for electrical resistors and pressure gradients for stenotic hydraulic segments. Ohm's law for electrical current flow corresponds to Hagen–Poiseuille's law for incompressible, laminar fluid flow.[24] V: Voltage, I: Electrical current, R: Resistance, P: Pressure, Q: Volumetric flow rate](/content/150/2019/10/2/img/JNRP-10-334-g003.png)
- The electric-hydraulic circuit analogy is conceptually useful for understanding how additional occipito-marginal sinus stenting decreased the trans-stenosis pressure gradient of the transverse sinus.[24] In this analogy, stenotic segments of hydraulic channels can be thought of as electrical resistors. In both circuits, potential energy is equivalent when in parallel configuration: voltages for electrical resistors and pressure gradients for stenotic hydraulic segments. Ohm's law for electrical current flow corresponds to Hagen–Poiseuille's law for incompressible, laminar fluid flow.[24] V: Voltage, I: Electrical current, R: Resistance, P: Pressure, Q: Volumetric flow rate
This case illustrates the possibility of parallel hemodynamic venous sinus drainage in NIVOD patients. Currently, there are no recommendations for the management of parallel stenotic venous sinuses in patients with NIVOD. Based on our findings, we have begun to investigate the venous pressure gradients of parallel outflow channels. Although substantial venous drainage through the occipital sinus is rare, co-dominance of the TS is commonly observed. Therefore, in patients who have residual or recurrent venous pressure gradients after unilateral TS stenting, manometry of major parallel sinuses appears warranted. If a significant pressure gradient is identified, additional VSS of a stenotic parallel segment may provide further physiologic improvement of intracranial venous drainage.
A limitation of this report is that clinical improvement may have been achieved with TS stenting only. However, since there was a residual trans-stenotic pressure gradient after the initial TS stent deployment, we performed concurrent stenting of a parallel outflow channel to reduce the likelihood of refractory symptoms and obviate the need for additional procedures. Furthermore, it is unknown whether occipito-marginal sinus stenting alone would have completely obliterated both trans-stenosis pressure gradients. Preoperative calculation of flow velocity in our patient's transverse and occipito-marginal sinuses, using either transcranial Doppler ultrasound[27] or phase-contrast magnetic resonance imaging,[2829] may have provided supporting evidence for occipito-marginal sinus stenting alone. We hypothesize that stenting the affected sinus with the highest impedance, which can be estimated using flow velocity, pressure gradient, and Hagen–Poiseuille's law,[24] would maximally reduce the trans-stenosis pressure gradient in a parallel hemodynamic circuit. The current IIH literature is limited mainly to TS and superior sagittal sinus stenting.[825] Therefore, further studies are needed to determine the clinical outcomes for stenting alternate venous outflow pathways such as occipito-marginal sinuses, which may exist in parallel with a dominant TS.
CONCLUSION
VSS has emerged as an effective treatment for appropriately selected NIVOD patients with IIH or non-IIH headache syndromes. The majority of VSS for NIVOD involves the dominant TS.[3789] We present a case in which concurrent VSS of both the TS and occipito-marginal sinus was necessary to obliterate the trans-stenosis pressure gradient across both venous channels. We hypothesize that this result may be explained using an electric-hydraulic analogy and modeled the sinuses as a parallel hemodynamic circuit. Neurointerventionalists should be aware of parallel hemodynamic drainage patterns and consider manometry of parallel venous outflow pathways if TS stenting alone fails to adequately alleviate the trans-stenosis pressure gradient. If stenosis of a major parallel outflow channel is identified, additional VSS of this affected segment may further reduce the pressure gradient across the initially stented TS.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. Informed consent was obtained for images and other clinical information to be reported in the journal. The patient name and identifying information has been removed to protect her privacy.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Venous sinus stenting in idiopathic intracranial hypertension: Results of a prospective trial. J Neuroophthalmol. 2017;37:113-21.
- [Google Scholar]
- Venous sinus stenting in patients without idiopathic intracranial hypertension. J Neurointerv Surg. 2017;9:512-5.
- [Google Scholar]
- Endovascular treatment of venous sinus stenosis in idiopathic intracranial hypertension: Complications, neurological outcomes, and radiographic results. ScientificWorldJournal. 2015;2015:140408.
- [Google Scholar]
- Venous sinus stenting for idiopathic intracranial hypertension: A review of the literature. J Neurointerv Surg. 2013;5:483-6.
- [Google Scholar]
- Patency of the vein of labbé after venous stenting of the transverse and sigmoid sinuses. J Neurointerv Surg. 2017;9:587-90.
- [Google Scholar]
- Incidence and predictors of dural venous sinus pressure gradient in idiopathic intracranial hypertension and non-idiopathic intracranial hypertension headache patients: Results from 164 cerebral venograms. J Neurosurg. 2017;126:347-53.
- [Google Scholar]
- Long-term patency of venous sinus stents for idiopathic intracranial hypertension. J Neurointerv Surg. 2014;6:238-42.
- [Google Scholar]
- A pilot study and novel angiographic classification for superior sagittal sinus stenting in patients with non-thrombotic intracranial venous occlusive disease. J Neurointerv Surg. 2018;10:74-7.
- [Google Scholar]
- Venous sinus stenting for reduction of intracranial pressure in IIH: A prospective pilot study? J Neurosurg. 2017;127:1126-33. doi: 10.3171/2016.8.JNS16879. [Epub 2016 Dec 23]
- [Google Scholar]
- Idiopathic intracranial hypertension: The prevalence and morphology of sinovenous stenosis. Neurology. 2003;60:1418-24.
- [Google Scholar]
- A six-item short-form survey for measuring headache impact: The HIT-6. Qual Life Res. 2003;12:963-74.
- [Google Scholar]
- Development of the tinnitus handicap inventory. Arch Otolaryngol Head Neck Surg. 1996;122:143-8.
- [Google Scholar]
- The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473-83.
- [Google Scholar]
- Development of an intracranial dural arteriovenous fistula after venous sinus stenting for idiopathic intracranial hypertension. J Neurointerv Surg. 2018;10:e15.
- [Google Scholar]
- Venous sinus stenting using transcranial access for the treatment of idiopathic intracranial hypertension in a pediatric patient. J Neurosci Rural Pract. 2017;8:672-5.
- [Google Scholar]
- Development of an intracranial dural arteriovenous fistula after venous sinus stenting for idiopathic intracranial hypertension. BMJ Case Rep 2017 2017 pii: bcr-2017-013282
- [Google Scholar]
- Transient resolution of venous sinus stenosis after high-volume lumbar puncture in a patient with idiopathic intracranial hypertension. J Neurosurg. 2018;129:153-6.
- [Google Scholar]
- Effect of body mass index on venous sinus pressures in idiopathic intracranial hypertension patients before and after endovascular stenting. Neurosurgery. 2018;82:555-61.
- [Google Scholar]
- Intracranial venous sinus stenting for benign intracranial hypertension: Clinical indications, technique, and preliminary results. World Neurosurg. 2011;75:648-52.
- [Google Scholar]
- Idiopathic intracranial hypertension: 12 cases treated by venous sinus stenting. J Neurol Neurosurg Psychiatry. 2003;74:1662-6.
- [Google Scholar]
- Resolution of pulsatile tinnitus after venous sinus stenting in patients with idiopathic intracranial hypertension. PLoS One. 2016;11:e0164466.
- [Google Scholar]
- Intracranial venous pressures under conscious sedation and general anesthesia. J Neurointerv Surg. 2017;9:986-9.
- [Google Scholar]
- Management of hepatocellular carcinoma in cirrhotic patients with portal hypertension: Relevance of hagen-poiseuille's law. Liver Cancer. 2014;3:428-38.
- [Google Scholar]
- Design of pressure-driven microfluidic networks using electric circuit analogy. Lab Chip. 2012;12:515-45.
- [Google Scholar]
- Dural sinus stenting for idiopathic intracranial hypertension: Factors associated with hemodynamic failure and management with extended stenting. J Neurointerv Surg. 2017;9:867-74.
- [Google Scholar]
- Pattern of pressure gradient alterations after venous sinus stenting for idiopathic intracranial hypertension predicts stent-adjacent stenosis: A proposed classification system. J Neurointerv Surg. 2018;10:391-5.
- [Google Scholar]
- Cerebral venous flow velocity predicts poor outcome in subarachnoid hemorrhage. Stroke. 2004;35:1873-8.
- [Google Scholar]
- Phase contrast MR imaging measurements of blood flow in healthy human cerebral vessel segments. Physiol Meas. 2015;36:1517-27.
- [Google Scholar]
- In vivo analysis of physiological 3D blood flow of cerebral veins. Eur Radiol. 2015;25:2371-80.
- [Google Scholar]






