Translate this page into:
Computed tomography predictors of adult spinal cord injury without radiographic abnormality
*Corresponding author: Navneet Singla, Department of Neurosurgery, Post Graduate Institute of Medical Education and Research, Chandigarh, India. drnavi2007@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Singla N, Nellikoppad HS, Latawa A, Ahuja CK. Computed tomography predictors of adult spinal cord injury without radiographic abnormality. J Neurosci Rural Pract 2022;13:658-62.
Abstract
Objective:
Elasticity of the skeletal system in children and degenerative changes in adults are responsible for SCIWORA. The purpose of this study was to determine those degenerative changes on CT scan that predispose adults to SCIWORA, their correlation with MRI findings, clinical presentation and recovery.
Materials and Methods:
This prospective study was conducted over a period of 1.5 years and 30 patients were enrolled. Apart from the demographic profile, mode of injury, clinical symptoms, ASIA at admission, X-ray, CT and MRI findings were noted. All patients were managed conservatively and were followed up after 3 months. NCCT and MRI findings were correlated with each other, with clinical presentation and with recovery. Recovery was defined as any improvement in ASIA class.
Statistical Analysis:
Data was collected and organized. For normally distributed data parametric test and for others non-parametric test was used. Kendall tau rank correlation coefficient was used to measure the ordinal association between two measured quantities.
Results:
28 (93.3%) patients were males and 2 (6.7%) were females. Patients with osteoporosis and/or osteophytes (n = 16) had a higher incidence of development of cord edema or non-haemorrhagic contusion (n = 15) (P = 0.028) while patients with canal stenosis and/or ligamentous calcification (n = 14) had a higher incidence of development of haemorrhagic contusion (n = 12) (P = 0.04). Patients with canal stenosis and/or ligament calcification showed significantly less recovery (n = 3) when compared with patients of osteophytes and/or osteoporosis (n = 6) (P = 0.04). Disc abnormality was seen in 1 patient only. 9 patients showed recovery and maximum recovery was seen in ASIA D (n = 4) class while no patient recovered in ASIA A class.
Conclusion:
Osteoporosis, osteophytes, canal stenosis and ligament calcification are the factors that predispose adults to SCIWORA. The final outcome seems to be poorer in cases of canal stenosis when compared with osteophytes and osteoporosis. NCCT findings can be used as an adjunct to MRI to predict clinical presentation, severity and recovery in adult SCIWORA.
Keywords
Spinal cord injury without radiographic abnormality
Spinal cord injury without computed tomography evidence of trauma
Non-contrast computed tomography
Magnetic resonance imaging
INTRODUCTION
Spinal cord injury without radiographic abnormality (SCIWORA) is a term used to represent clinicoradiologic mismatch in children with spinal cord injury.[1] This term was coined by Pang and Wilberger in 1982 as the presence of neurologic deficits in the background of normal x-rays and computed tomography (CT) scan in pediatric patients.[2] These cases are generally diagnosed on magnetic resonance imaging (MRI). However, some authors have used the term “Real SCIWORA” for cases with normal MRI.[3] Initially, this terminology was extrapolated to adults also, but as our understanding has evolved, we found that the term spinal cord injury without CT evidence of trauma (SCIWOCTET) better defines adult SCIWORA because the CT in adult SCIWORA shows degenerative changes in the majority which are not normal, though also, those are not the result of trauma.[4] Degenerative changes predispose adults to SCIWORA. In this study, we tried to determine the degenerative changes on CT scan that can predict the occurrence of adult SCIWORA.
MATERIALS AND METHODS
This study is a prospective, observational, and non-randomized study. All patients (age >18 years) over a period of 1.5 years (July 2019–December 2020) with a diagnosis of SCIWOCTET (there was no fracture or dislocation on CT scan though other degenerative changes may be seen) were enrolled in the study. All comatose patients and those with any evidence of trauma on X-rays or CT scan were excluded from the study. Apart from the demographic profile of these patients, mode of injury, time of injury, clinical symptoms, American Spine Injury Association (ASIA) grade, spinal shock, and other associated injuries were noted. All patients were evaluated with X-rays, CT, and MRI. CT findings such as osteoporosis (defined on DEXA scan with T value ≤−2.5), canal stenosis (calculated using Torg-Pavlov ratio <0.8),[5] ligament abnormalities, osteophytes, congenital bone abnormality and MRI findings such as cord edema, contusion, disc herniation, and ligament abnormalities were noted. All patients were immobilized and were managed conservatively and those presenting in the acute phase (within 6 h) were given steroids. Non-contrast CT (NCCT) and MRI findings were correlated with each other, with clinical presentation and with recovery. Recovery was defined as any improvement in ASIA class at the 3-month follow-up.
RESULTS
Among 36 patients diagnosed with SCIWOCTET, four were lost to follow-up and two patients died in hospital admission due to pulmonary embolism so the remaining 30 patients were enrolled for analysis. Twenty-eight patients (93.3%) were males and 2 (6.7%) were females. About 10% of patients were in the 21–30 years of age group, 20% in 31–40 years of age group, and 36.66% of the patients (n = 11) were within the age group of 41–50. Above 50 age group constitutes 33.3% (n = 10). Mode of injury was road traffic accident (RTA) in 26 (86.7%) patients followed by fall from height in 4 (13.3%) patients. The onset of symptoms was within minutes in 27 patients (90%) while three patients (10%) took hours to develop symptoms probably due to development of edema later on. The most common symptom was the weakness of the limbs seen in all patients followed by tenderness at back followed by backache and sensory loss in 17 patients which were followed by incontinence in five patients. None of the patients in our study had a spinal shock and reflex loss. The frequency of various symptoms in our study is shown in [Figure 1]. Patients were classified according to ASIA class at admission and at follow-up as shown in [Table 1]. The level of injury was C5–7 in 24 (80%) patients, T1-T3 in 5 (17%) patients. One patient presented with a dorsolumbar injury. Various degenerative changes on NCCT found in our patients (NCCT) are shown in [Figure 2 and Table 2]. It shows the NCCT findings corresponding to the level at which MRI changes were found. These degenerative changes were directly proportional to age with the highest incidence in more than 60 years of age group. The posterior longitudinal ligament calcification is of four types: Continuous, segmental, mixed, and localized and was found to be highest in the 51–60 age group than any other age group in this study. Ligamentum flavum was not calcified. Various MRI findings in patients of SCIWOCTET are shown in [Figure 3 and Table 3]. It shows that one patient has disc herniation alone; however, other patients of disc herniations with associated findings like contusions are classified along with contusions and same as the case with patients of ligamentous abnormalities. Similarly in [Table 3], patients with contusions also have associated edema but those patients were categorized with contusions only. Patients with osteoporosis and/or osteophytes (n = 16) had a higher incidence of development of cord edema or non-hemorrhagic contusion (signal change or myelomalacia) (n = 15) (P = 0.028) while patients with canal stenosis and/or ligamentous calcification (n = 14) had a higher incidence of development of hemorrhagic contusion (n = 12) (P = 0.04). Patients with canal stenosis and/or ligament calcification showed significantly less recovery (n = 3) (P = 0.04) when compared with patients of osteophytes and/or osteoporosis (n = 6). After 3 months of follow-up, a total of nine patients showed improvement. Four out of ten patients recovered in ASIA D class, four out of 11 patients recovered in ASIA C class (one improved to ASIA D and other three improved to ASIA E), and one out of five patients showed improvement in ASIA B (improved to ASIA D). None of the patients in ASIA class A showed any improvement. Six (37.5%) out of 16 patients with osteophytes and/or osteoporosis recovered and 3 (21.42%) patients of canal stenosis and/or ligamentous calcification showed recovery. NCCT spine and recovery is shown in [Table 4]. About 40% (n = 6) of the patients with edema/non-hemorrhagic contusion showed recovery whereas 16.66% (n = 2) showed recovery from hemorrhagic contusion.
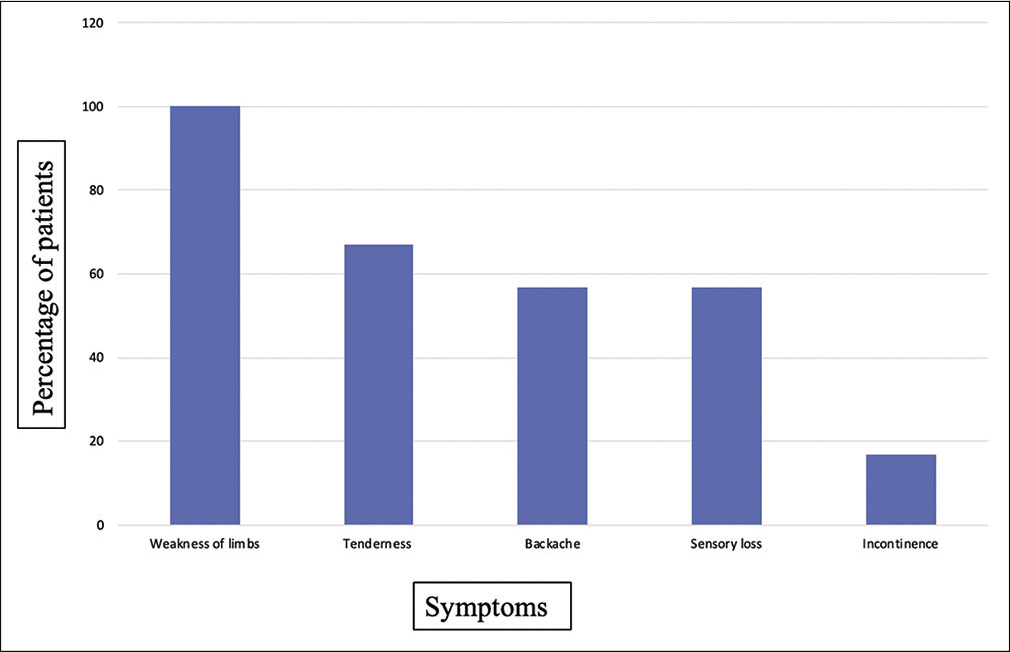
- Percentage of patients with various symptoms.
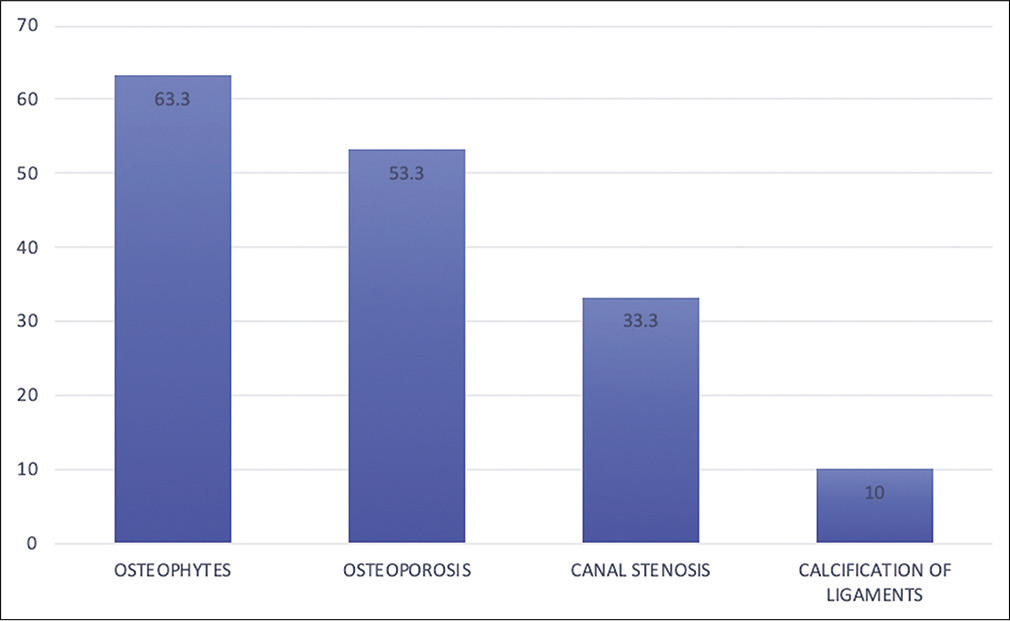
- Frequency distribution of various lesions in non-contrast computed tomography (NCCT) spine. NCCT spine showed osteophytes in 63% (n = 19) of the patients. Osteoporosis was seen in 53% (n = 16) patients. Canal stenosis was found in 10 (33%) patients and ligamentous calcification in 3 (10%) patients.
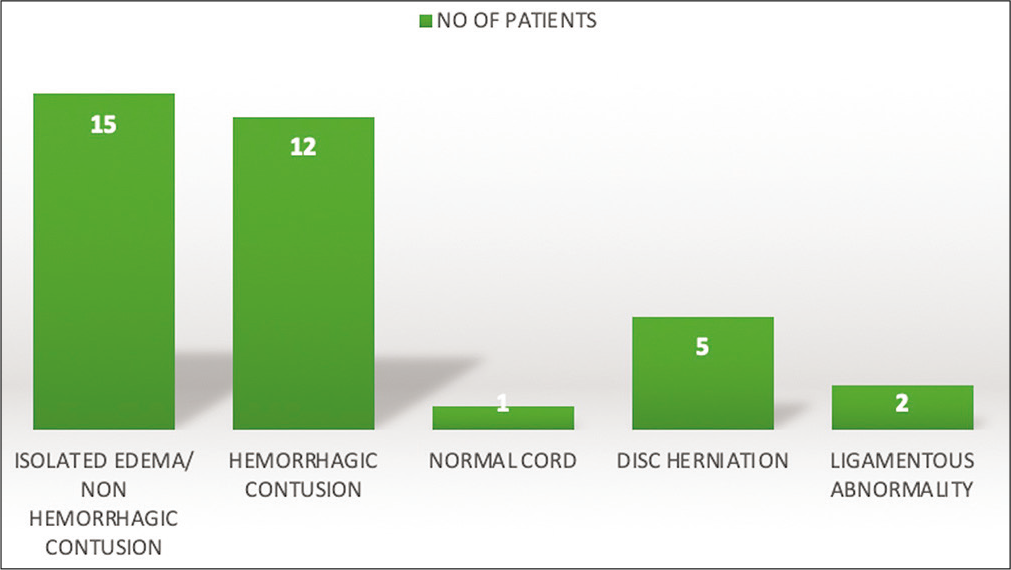
- Findings on magnetic resonance imaging.
| ASIA CLASS | ASIA A (%) | ASIA B (%) | ASIA C (%) | ASIA D (%) | ASIA E (%) |
|---|---|---|---|---|---|
| Initially | 4 (13.33) | 5 (16.66) | 11 (36.66) | 10 (33.33) | - |
| At 3-month follow-up | 4 (13.33) | 4 (13.33) | 7 (23.33) | 8 (26.66) | 7 (23.33) |
ASIA: American Spinal Injury Association
| NCCT Spine findings | No of patients (percentage) |
|---|---|
| Osteophytes | 13 (43.33) |
| Osteoporosis | 3 (10) |
| Canal stenosis | 10 (33.33) |
| Ligamentous calcification | 4 (13.33) |
MRI: Magnetic resonance imaging, NCCT: Non-contrast computed tomography
| MRI findings | Spinal cord edema/Non-hemorrhagic contusion | Hemorrhagic contusion | Disc herniation | Ligament abnormalities | Normal MRI (Real sciwora) |
|---|---|---|---|---|---|
| No of patient (percentage) | 15 (50) | 12 (40) | 1 (3.33) | 1 (3.33) | 1 (3.33) |
MRI: Magnetic resonance imaging
| NCCT Spine | ASIA Grade | Total Patient | Percent | Recovery | Percent |
|---|---|---|---|---|---|
| Osteoporosis and osteophytes | A | - | - | - | - |
| B | 2 | 6.66 | 1 | 50 | |
| C | 7 | 23.33 | 3 | 42.85 | |
| D | 7 | 23.33 | 2 | 28.57 | |
| Total | 16 | 53.33 | 6 | 37.5 | |
| Canal stenosis and calcification of ligaments | A | 4 | 13.33 | 0 | 0 |
| B | 3 | 10 | 0 | 0 | |
| C | 4 | 13.33 | 1 | 25 | |
| D | 3 | 10 | 2 | 66.66 | |
| Total | 14 | 46.66 | 3 | 21.42 |
ASIA: American Spinal Injury Association, NCCT: Non-contrast computed tomography
DISCUSSION
This prospective study to the best of our knowledge is the only study determining the severity of clinical features based on findings of NCCT spine. The initial largest study which evaluated the adult SCIWOCTET was NEXUS study by Hendey et al. which incorporated 27 patients.[6] The term SCIWORA was initially described in children and the mechanism cited was the inherent elasticity of the skeletal system, leading to spinal cord injury without fractures/ dislocations.[7] However, in adults, the mechanisms are entirely different because the adult skeletal system is not elastic like the children. In adults, the degenerative changes predispose adults to SCIWORA and since these degenerative changes are neither normal nor traumatic so the term SCIWOCTET should be used in adults.[8]
Crooks and Birkett and Regenbogen et al. reported a 28% incidence of SCIWORA in adult patients.[9,10] The total number of spine patients including SCIWORA patients treated at our center during this study period was 443. Incidence of SCIWORA in this study was 8.12%. Incidence in our study is comparable to as quoted by Tewari et al. (8.12% vs. 8.47%).[4]
Majority of the patients are males due to the high incidence of RTA s in males in conjunction with our study where 93.3% of patients were males. A RTA was the mechanism of injury in 86.7% of patients of our study while the rest had fallen from height. The most common symptom was the weakness of the limbs seen in all patients followed by tenderness at back followed by backache and sensory loss which was followed by incontinence. In SCIWOCTET, motor weakness predominates over sensory symptoms due to the arrangement of fibers, the motor being centrally situated while sensory being peripherally situated.[11] None of the patients in our study had a spinal shock and reflex loss. The occurrence of symptoms was within minutes in the majority while 10% of patients took hours to develop symptoms. These are those patients who presented to us late after injury and the time after which their symptom onset occurred was purely based on history from the relatives. We cannot be sure about the subtle injury and deficits because no one has examined them during that time. Thus, we can only hypothesize that these are the patients may be in whom the edema took some time to develop that is why symptoms occurred after a while. The majority (80%) of the injuries were at the lower cervical level (C5–7) which might be explained because of the fulcrum of the cervical motion at the lower spine.
Spinal canal stenosis is thought to be the major factor predisposing adults to SCIWOCTET.[5,12,13] Various degenerative changes on NCCT spine in adult SCIWOCTET in our study were osteophytes, osteoporosis, canal stenosis, and ligamentous calcification in decreasing order of occurrence. These degenerative changes tend to increase with age and, henceforth, the adults in the 5–6th decade are the most usual sufferers.[14] In our study, degenerative changes were directly proportional to age with the highest incidence in more than 60 years of age group. Osteophytes and osteoporosis were the most common findings than canal stenosis and calcification of ligaments similar to a study by Tator.[15]
The most common MRI findings seen in SCIWOCTET were cord edema/non-hemorrhagic contusion (50%), hemorrhagic contusion (40%), disc herniation, and ligamentous abnormalities. Disc herniation was commonly seen between 41 and 60 years of age in our study while ligamentous abnormalities were seen in a slightly younger population of 31–50 years correlating with the increased occurrence of a hemorrhagic contusion in the same age group. Kulkarni et al. have already described these cord changes in SCIWOCTET and their prognostic value has already been proved by others with cord edema/non-hemorrhagic contusion having a better prognosis than the hemorrhagic contusions.[16-18]
We tried to correlate the NCCT spine findings with MRI findings. We have found that patients with osteoporosis and/or osteophytes had a higher incidence of development of cord edema or non-hemorrhagic contusion (P = 0.028) while patients with canal stenosis had a higher incidence of development of hemorrhagic contusion (P = 0.04) indirectly proving that osteoporosis and/or osteophytes were associated with better outcome when compared to canal stenosis in SCIWOCTET.
The rate of recovery was significantly better in the younger age group (21–30 years) as compared to the elderly similar to literature.[19] Patients with canal stenosis and/or ligament calcification showed significantly less recovery (P = 0.04) when compared with patients of osteophytes and/or osteoporosis again signifying a worse outcome in canal stenosis cases when compared with osteophytes and/or osteoporosis in SCIWOCTET. Patients with isolated cord edema and/or non-hemorrhagic contusions showed better recovery than patients of cord hemorrhage and contusion due to the fact that cord edema heals with minimal myelomalacia while cord contusions and hemorrhage form cysts in a recovery phase and thus recover late. This is also evident by the fact that patients with hemorrhage and contusions mainly presented in ASIA A and B class while those with cord edema presented mainly in ASIA C and ASIA D class. Carrol et al. in their study proved maximum improvement in ASIA D class as compared to ASIA B and C.[20] In our study, we also found maximum improvement in ASIA D class (40%) followed by ASIA C (36.36%), followed by ASIA B (20%) and no improvement was seen in ASIA A class. Hence, post-injury ASIA class also determines recovery with better outcomes in ASIA C and ASIA D as compared to ASIA A and ASIA B classes. Motor symptoms/signs improved in most.
CONCLUSION
SCIWOCTET is more common in the cervical cord. Osteophytes, osteoporosis, canal stenosis, and ligament calcification were the main CT findings present in cases of adult SCIWOCTET. Osteophytes, osteoporosis on CT, and edema/non-hemorrhagic contusion on MRI confer better outcomes. Canal stenosis and hemorrhagic contusion along with elderly age and poor ASIA at admission are associated with poor clinical presentation and outcome. NCCT findings can be used as an adjunct to MRI to predict clinical presentation, severity, and recovery in SCIWORA.
Declaration of patient consent
Patient’s consent not required as there is no patient in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Spinal cord injury without radiographic abnormality in children the SCIWORA syndrome. J Trauma. 1989;29:654-64.
- [CrossRef] [PubMed] [Google Scholar]
- Spinal cord injury without radiographic abnormalities in children. J Neurosurg. 1982;57:114-29.
- [CrossRef] [PubMed] [Google Scholar]
- Spinal cord injury without radiological abnormality in adults: Clinical and radiological discordance. World Neurosurg. 2018;114:e1147-51.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis and prognostication of adult spinal cord injury without radiographic abnormality using magnetic resonance imaging: Analysis of 40 patients. Surg Neurol. 2005;63:204-9.
- [CrossRef] [PubMed] [Google Scholar]
- The Torg-Pavlov ratio for the prediction of acute spinal cord injury after a minor trauma to the cervical spine. Spine J. 2013;13:605-12.
- [CrossRef] [Google Scholar]
- Spinal cord injury without radiographic abnormality: Results of the national emergency X-radiography utilization study in blunt cervical trauma. J Trauma. 2002;53:1-4.
- [CrossRef] [PubMed] [Google Scholar]
- The misapplication of the term spinal cord injury without radiographic abnormality (SCIWORA) in adults. J Trauma Acute Care Surg. 2012;73:1261-6.
- [CrossRef] [PubMed] [Google Scholar]
- Cervical spinal cord injuries in patients with cervical spondylosis. AJR Am J Roentgenol. 1986;146:277-84.
- [CrossRef] [PubMed] [Google Scholar]
- Predicting the risk and severity of acute spinal cord injury after a minor trauma to the cervical spine. Spine J. 2013;13:597-604.
- [CrossRef] [PubMed] [Google Scholar]
- The risk of acute spinal cord injury after minor trauma in patients with preexisting cervical stenosis. Neurosurgery. 2015;77:561-5.
- [CrossRef] [PubMed] [Google Scholar]
- The adult spinal cord injury without radiographic abnormalities syndrome: Magnetic resonance imaging and clinical findings in adults with spinal cord injuries having normal radiographs and computed tomography studies. J Trauma. 2008;65:86-93.
- [CrossRef] [PubMed] [Google Scholar]
- 1.5 tesla magnetic resonance imaging of acute spinal trauma. Radiographics. 1988;8:1059-82.
- [CrossRef] [PubMed] [Google Scholar]
- Adult spinal cord injury without radiographic abnormalities (SCIWORA): Clinical and radiological correlations. J Clin Med Res. 2009;1:165-72.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and magnetic resonance imaging correlation in acute spinal cord injury. Spinal Cord. 1997;35:664-73.
- [CrossRef] [PubMed] [Google Scholar]
- Neurological outcome, working capacity and prognostic factors of patients with SCIWORA. Spinal Cord. 2012;50:78-80.
- [CrossRef] [PubMed] [Google Scholar]
- Spinal cord injuries without radiologic abnormality in children: A systematic review. Spinal Cord. 2015;53:842-8.
- [CrossRef] [PubMed] [Google Scholar]






