Translate this page into:
Traumatic spinal cord injury in West Virginia: Impact on long-term outcomes by insurance status and discharge disposition
-
Received: ,
Accepted: ,
How to cite this article: Dekeseredy P, Hickman WP, Fang W, Sedney CL. Traumatic spinal cord injury in West Virginia: Impact on long-term outcomes by insurance status and discharge disposition. J Neurosci Rural Pract 2022;13:652-7.
Abstract
Objectives:
Specialized rehabilitation is important for people with traumatic spinal cord injuries (SCIs) to optimize function, independence and mitigate complications, and access to this service varies by the payor. In West Virginia, admission to acute rehabilitation facilities is a “non-covered entity,” impeding access to this care for patients with SCI and Medicaid. Our previous work examined the discharge disposition from an acute care hospital of patients with and without Medicaid and found that Medicaid patients were almost twice as likely to be discharged home or to a nursing home, despite similar injury severity and younger age compared to non-Medicaid patients. West Virginia is a largely rural state with multiple health-care challenges. A lack of availability of rehabilitation facilities for Medicaid beneficiaries likely explains this difference. This present study examines the relationship between insurance coverage, discharge disposition at time of injury, and long-term outcomes for people in West Virginia with traumatic SCI.
Materials and Methods:
This study utilized a retrospective chart review and telephone survey from a Level 1 Trauma Center in West Virginia. Participants included 200 patients with traumatic SCI from 2009 to 2016 in West Virginia. Thirty-four patients completed the survey through telephone interviews, with another 16 completing the survey but declining to answer economic questions. Survey participants were asked the Craig Handicap Assessment and Reporting Technique (CHART), which indicates the degree of impairment, and disability; they experience years after initial injury and rehabilitation. Proportional odds regression models, a regression model generalization of the Wilcoxon rank sum test, were employed where normal distribution of the response variables was not assumed and was performed, controlling for age and injury severity.
Results:
Total CHART score correlated with discharge disposition (P = 0.01). Insurance type correlated with mobility sub-score (P = 0.03).
Conclusion:
Patients discharged to a rehabilitation center have overall higher CHART scores post-injury, indicating better long-term outcomes than those discharged home or a nursing home. People with Medicaid as payors had lower scores for mobility than those with other insurance coverage.
Keywords
Spinal cord injury
Insurance disparities
Health Outcomes
INTRODUCTION
A traumatic spinal cord injury (SCI) typically occurs suddenly and unexpectedly, causing lifelong physical, psychological, and socioeconomic consequences. The incidence of traumatic SCIs in the United States is estimated to be 54 cases per million.[1] From 1973 to 2020, vehicular accidents (41.93%) and unintentional falls (23.04%) were the leading causes for SCI in the United States. Long-term outcomes for patients with traumatic SCI depend on many factors including level, and completeness of neurological harm, age,[2] and other variables, including access to high-quality rehabilitation. Significant is the acute phase of rehabilitation, the intensive, multidisciplinary treatment that begins as soon as possible after stabilization in the hospital and can be predictive of better long-term outcomes.[3] Unfortunately, even after intense and lengthy rehabilitation periods, people with SCIs may experience an increase in secondary complications and a progressive decline in function over time.[2,4] However, specialized rehabilitation after the acute injury can mitigate long-term complications and disability to achieve maximum recovery.[5,6]
Our previous research indicated that people with SCI in West Virginia who have publicly funded Medicaid insurance have longer hospital stays and are more apt to be discharged home or to a skilled nursing facility rather than a specialized rehabilitation facility.[7] This disparity in discharge disposition likely results from inpatient rehabilitation facility admission being a “non-covered service” as per the West Virginia Health and Human Resources Bureau of Medical Services[8] and may lead to patients with Medicaid being released to a setting that lacks specially designed SCI programs such as a private home or nursing home. Lack of specialized care may prevent patients from reaching optimum function, independence, and quality of life.[9,10] The immediately increased reliance on others and future functional decline exacerbate the multiple socioeconomic aspects associated with a SCI[6] and can add physical and emotional strain to family caregivers.[11] In addition, in West Virginia, Medicaid patients stay in the acute hospital setting for over twice as long as patients with other coverage, possibly related to a lack of specialized rehabilitation beds that accept Medicaid as a payor.[7] Despite the immediate health-care disparities people experience related to public versus private insurance, few studies have examined the long-term outcomes of people with SCI related to insurance status and discharge disposition. This study aims to explore the relationship between insurance coverage, discharge disposition, and long-term outcomes for people in West Virginia with traumatic SCI.
MATERIALS AND METHODS
Subjects
The Center for Medicare and Medicaid Services (CMS) requires that patients going to acute rehabilitation be able to undergo 3 h of intense rehabilitation services at least 5 days/week. In skilled nursing facilities, patients are either unable to tolerate the rehabilitation requirements for acute rehabilitation facilities, or are too high or too low functioning to benefit from those services. There are no specific rehabilitation requirements for home care. These requirements are similarly used by other payors.[12] At our facility, disposition is recommended by inpatient rehabilitation services and then arranged by care management based on what the patient/family desire and payor coverage.[7] The Jon Michael Moore Trauma Center is the only nationally certified Level 1 trauma center in West Virginia. Since 1985, the trauma center has maintained an institutional trauma registry that captures all trauma patients’ demographic and medical information. Following approval from the institutional review board, a trauma databank query was ran for all patients admitted with a new traumatic SCI based on ICD9 and 10 codes from 2009 to 2016. We excluded patients under 18 years of age because the instrument we chose measures adult outcomes such as economic and cognitive independence.[13] Patients were included if they had ICD9 codes for “fracture of vertebral column with SCI” (806 group) as well as patients who were erroneously coded within the 952 group (“SCI without evidence of spinal bone injury”) if they also carried a separate diagnosis of a corresponding fracture at the level of injury. Using ICD codes for institutional studies in the setting of other US Level 1 trauma centers has been shown to be highly accurate.[14] Patient demographics, length of stay, injury mechanism discharge disposition, associated injuries, discharge status, Injury Severity Score (ISS), charges billed, charges collected, and insurance type on discharge were returned. ISS is a standardized tool used to grade the severity of injury of trauma patients.[15]
The outcome measure
The Craig Handicap Assessment and Reporting Technique (CHART) consists of 32 questions that evaluate six domains to evaluate the degree of impairment and disability; patients experience years after initial injury and rehabilitation.[13] Domains or subscales of CHART include: (1) Physical independence, (2) mobility, (3) occupation, (4) social integration, (5) economic self-sufficiency, and (6) cognitive independence. Each domain has a maximum score of 100, indicating normal function. The higher the score, the less physical impairment and greater integration and engagement in their social community. CHART was chosen as the outcome measure because it has been evaluated extensively, has demonstrated reliability and validity for long-term outcomes of neurologic disease, can be administered by telephone, and answered by proxy if necessary. In addition, CHART is aimed at people with SCI, predominantly younger and without cognitive impairment.[16] Research personnel contacted patients by telephone to explain the study, obtain verbal consent to participate, and administer the survey.
Data analysis
This research aimed to investigate whether there was any significant difference regarding the total CHART scores or sub scores (physical independence/cognitive independence/ mobility score/occupation score/social integration, and economic self-sufficiency) among insurance types (or discharge locations) at the time of injury after controlling for age and ISS. Proportional odds regression models, a regression model generalization of the Wilcoxon rank sum test, were employed where normal distribution of the response variables was not assumed.
All statistical analyses were performed using R (Version 4.0.3) and the “rms” (Version 6.1-1) package.
RESULTS
The trauma bank query identified 200 patients. [Figure 1] illustrates the selection of participants. We were able to contact 50 patients by telephone and asked them to complete the CHART survey. Thirty-four patients completed the entire survey to generate a CHART score and 16 CHART surveys were incomplete.
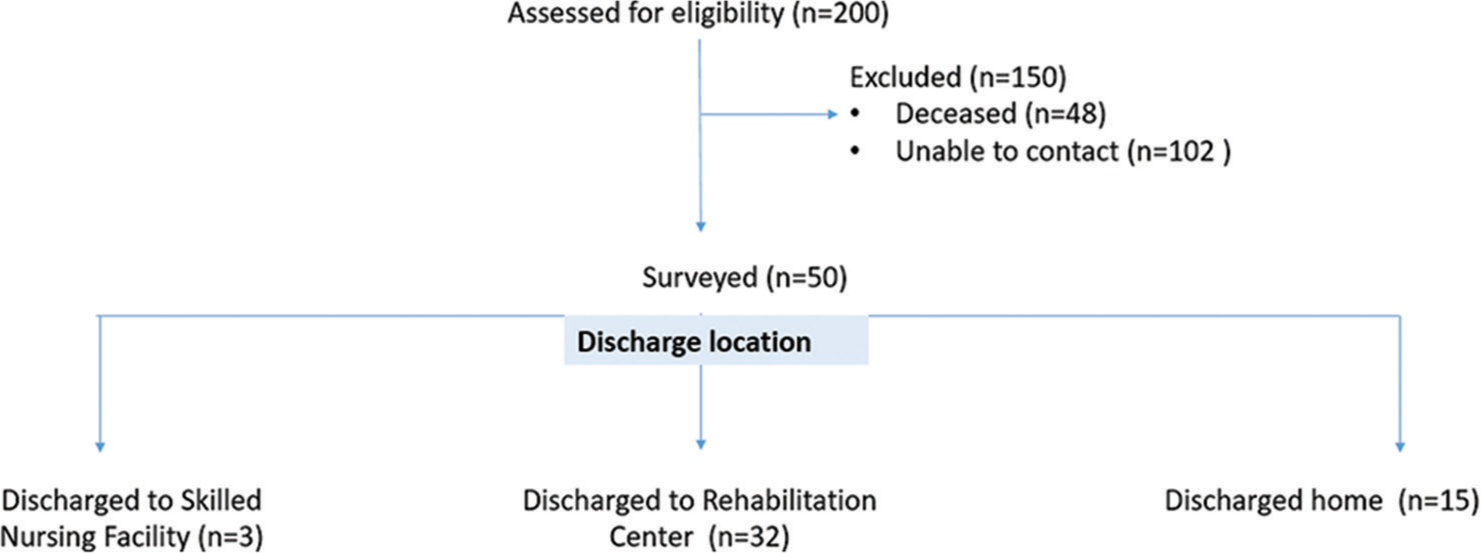
- Diagram to identify participants.
Payor distribution for complete CHART scores is presented in [Table 1].
| Payor number of patients % of patients*(%) | |
|---|---|
| Medicaid | 6 18 |
| Automotive | 5 15 |
| Commercial | 12 35 |
| Medicare | 6 18 |
| Workman’s compensation | 5 15 |
n=34 * rounded to whole number, CHART: Craig handicap assessment and reporting technique
The age, ISS, and discharge disposition for Medicaid and non-Medicaid insurance coverage is collected and presented in [Table 2].
| Characteristic | Medicaid | Non-medicaid |
|---|---|---|
| Mean age | 36 | 45 |
| ISS | 21 | 24 |
| Disposition to Rehab. Center | 3 of 6 | 20 of 28 |
(n=34)
Results from the statistical analysis are presented in [Table 3].
| Insurance coverage** | Discharge location*** | |
|---|---|---|
| Physical independence | 0.60 | 0.69 |
| Cognitive independence | 0.11 | 0.22 |
| Mobility score | 0.03 | 0.55 |
| Occupation score | 0.10 | 0.32 |
| Social integration | 0.17 | 0.09 |
| Economic self sufficiency | 0.06 | 0.25 |
| Total CHARTscore | 0.06 | 0.01 |
The significance level was set at P = 0.05. After controlling for age and ISS, the total CHART score correlated with discharge disposition (P = 0.01). Insurance type significantly correlated with mobility sub-score (P = 0.03). The bivariate correlation between “physical independence” and “level of injury” was −0.31, using Spearman’s rho. The bivariate correlation between “insurance coverage” and “discharge location” was −0.13, using Phi coefficient.
The incomplete CHART scores were missing economic data only due to patients declining to answer those questions over the phone. We conducted an analysis accounting for these incomplete surveys and found no significant difference in results.
DISCUSSION
Findings from this study suggest that discharge disposition has a significant relation to long-term outcomes as measured by the overall CHART survey. Patients discharged to a rehabilitation center have overall higher CHART scores post-injury, indicating better long-term results than those discharged home or to a nursing home. Insurance status at the time of injury is significantly related to the long-term post-injury motor sub score of CHART. Our previous work on this patient population indicated that patients with private insurance are more likely to be discharged to an acute rehabilitation center and thus more apt to receive the intense therapy required to maximize recovery.[7]
These results are similar to other investigations related to insurance coverage for people with SCI. For example, Tate et al. found people with Medicaid coverage received less benefits than those covered by other insurance.[17] Similarly, Whiteneck et al. identified Medicaid as a predictor of poorer outcomes compared to private insurance following SCIs.[18] For people with SCIs, rehabilitation can be a prognostic factor of long-term outcomes. Early specialized intervention is associated with more significant improvement of functional outcomes.[19] Any delay, such as a lack of service, or bed unavailability could jeopardize the effectiveness of rehabilitations treatment and influence a patient’s recovery.[19] The present study similarly found that people who were discharged to specialized rehabilitation centers had better long-term outcomes.
A traumatic SCI brings many physical and psychological challenges. However, having Medicaid as a payor is associated with less chance of specialized rehabilitation and decreased chance of maximizing outcome long-term in West Virginia, as evidenced in the CHART motor sub score. Krause et al. conducted an 11-year follow-up study of people with traumatic SCI to identify mortality risk over time.[20] Similar to the present study, a large number of participants were deceased in Krause’s study (16%) and likewise, the researchers had difficulty contacting and recruiting former patients for the study. Results of their study indicate lower quality of life and more specifically, lower employment and activities were predictive of mortality for people with SCI. The strong relationship between life adjustment following SCI and mortality suggests the importance of timely and comprehensive rehabilitation following injury to maximize reintegration to society for these patients. Employment, and an overall active and satisfying lifestyle, was key to increased longevity post-injury.[20] Standardized treatment and discharge planning for all people in West Virginia with SCI regardless of insurance coverage could help to overcome this health-care disparity.
Unfortunately, there is no known way to reverse damage to the spinal cord although therapies to mitigate and even reverse the injury to neural pathways are in development.[21] Therefore, currently, people will live with the physical, psychological, and socioeconomic consequences of their injury for the rest of their lives. Life expectancy following a SCI has improved over the past 50 years; however, it is still lower than a person without SCI.[22] Prevention and early intervention in the immediate months following SCI may mitigate the secondary health conditions accelerated by aging with SCI and improve long-term outcomes.[22] Results from the present study evidenced that people discharged to a rehabilitation center have improved mobility compared to other discharge locations, often cited as a priority focus post-injury[23-25] and can lead to improved physical, psychological, and social outcomes.[26] Importantly, Richard-Denis et al. found mobility sub scores to be significantly associated with improved quality of life in the year following a traumatic SCIs.[26]
SCI is not the only area of care disparity that exists for Medicaid patients. Worse outcomes have been seen in Medicaid patients with cancer treatment, cardiac surgery, and orthopedic procedures.[27-31] Access to care is also different, with primary care physicians being less likely to accept new patients having Medicaid as compared to other insurance types.[32-35] Medicaid coverages vary by state, and in West Virginia, admission to acute rehabilitation facilities is a “non-covered entity” including for patients with SCI,[8] even though SCI is a CMS-compliant diagnosis and the benefits of acute rehabilitation for these patients are well-characterized.[9,36,37] Therefore, elucidation and documentation of these disparities and their long-term effects are important.
This study has some limitations. The sample is small and from one site and thus limits generalization to people outside of WV who experience a traumatic SCI but may be pertinent to other locations with similar payor systems. Furthermore, while the payor model may be specific to our area, it provides important observational data regarding the importance of equitable rehabilitation coverage to this population which can be utilized in other systems and locations. Furthermore, the recruitment of participants many years after their injury was challenging. The data set included people between 4 and 11 years post-injury and we were only able to contact 50 of the 152 (assumed) living patients to complete the CHART survey by telephone. The electronic medical record may not have up-to-date contact information (people who have moved or changed phone numbers or could also be deceased), which may have limited our ability to reach some patients. Contacting people by telephone could have limited our ability to speak to some people due to unanswered or deleted calls from an unknown number. The future studies with in-person administration (e.g., follow-up appointments) could encourage more participation than telephone contact.
This report is one of the few studies exploring long-term outcomes for people with SCI as influenced by insurance coverage. Our results suggest that having Medicaid affects access to post-acute rehabilitation services, which is associated with decreased mobility and less favorable long-term outcomes. The future studies aimed at health-care reform should include information on access to post-acute rehabilitation services, especially for those with life-altering events such as SCI, to ensure equitable, high-quality care for everyone.
CONCLUSION
This study examines the long-term impact of access to post-acute rehabilitation services as a potential predictor of health iniquities for individuals with SCI based on insurance.
People with traumatic SCI who are in receipt of rehabilitation services report less physical impairment and greater long-term integration and engagement in their social community. Health equity ensures, everyone receives the best available care to optimize recovery. However, people with Medicaid insurance may be denied the immediate rehabilitation care; they require based on insurance coverage leading to sub-optimum recovery.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Research reported in this publication was supported by the National Institute of General Medical Sciences of the National Institutes of Health under Award Number 5U54GM104942-05. The content is solely the authors’ responsibility and does not necessarily represent the official views of the National Institutes of Health.
Conflicts of interest
There are no conflicts of interest to report.
References
- NSCISC Spinal Cord Facts abd Figures ata Glance. 2020 SCI Data Sheet. National Spinal Cord Injury Statistical Center. Available from: https://www.nscisc.uab.edu/public/facts_and_figures_2020.pdf [Last accessed on 2020 Feb 12]
- [Google Scholar]
- Longitudinal outcomes in spinal cord injury: Aging, secondary conditions, and well-being. Arch Phys Med Rehabil. 1999;80:1429-34.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic complications of spinal cord injury. World J Orthop. 2015;6:24-33.
- [CrossRef] [PubMed] [Google Scholar]
- Investigating changes in quality of life and function along the lifespan for people with spinal cord injury. Arch Phys Med Rehabil. 2012;93:413-9.
- [CrossRef] [PubMed] [Google Scholar]
- International Perspectives on Spinal Cord Injury Malta: World Health Organization Press; 2013.
- [Google Scholar]
- Traumatic spinal cord injury in West Virginia: Disparities by insurance and discharge disposition from an acute care hospital. J Spinal Cord Med. 2020;43:106-10.
- [CrossRef] [PubMed] [Google Scholar]
- Covered Services, Limitations, and Exclusions for Hospital Services. Change Log Ch. 510. West Virginia: Department of Health and Human Resources West Virginia; Available from: https://www.dhhr.wv.gov/bms/provider/documents/manuals/bms_manuals_chapter_510_hospital.pdf [Last accessed on 2022 Jun 27]
- [Google Scholar]
- Nursing home residence: Quality of life among individuals with spinal cord injury. Am J Phys Med Rehabil. 2001;80:404-9.
- [CrossRef] [PubMed] [Google Scholar]
- Family caregivers of individuals with spinal cord injury: Exploring the stresses and benefits. Spinal Cord. 2016;54:732-6.
- [CrossRef] [PubMed] [Google Scholar]
- Inpatient Rehabilitation Facilities. United States: Centers for Medicare and Medicaid Services; Available from: https://www.cms.gov/medicare/provider-enrollment-and-certification/certificationandcomplianc/inpatientrehab [Last accessed on 2022 Mar 30]
- [Google Scholar]
- Craig Handicap Assessment and Reporting Technique. Available from: https://www.craighospital.org/uploads/craighospital.chartmanual.pdf [Last accessed on 2022 Jun 27]
- [Google Scholar]
- Accuracy of ICD-9-CM coding of cervical spine fractures: Implications for research using administrative databases. Ann Adv Automot Med. 2008;52:101-5.
- [Google Scholar]
- Abbreviated injury scale and injury severity score a scoring chart. J Trauma. 1985;25:60-4.
- [CrossRef] [PubMed] [Google Scholar]
- Craig handicap assessment and reporting technique (CHART) In: Tate RL, ed. A Compendium of Tests, Scales and Questionnaires (1st ed). United Kingdom: Psychology Press; 2010. p. :498-505.
- [CrossRef] [Google Scholar]
- Insurance benefits coverage for persons with spinal cord injuries: Determining diffreences across payors. J Am Paraplegia Soc. 1993;16:76-80.
- [CrossRef] [PubMed] [Google Scholar]
- Relationship of patient characteristics and rehabilitation services to outcomes following spinal cord injury: The SCIRehab project. J Spinal Cord Med. 2012;35:484-502.
- [CrossRef] [PubMed] [Google Scholar]
- Early versus delayed inpatient spinal cord injury rehabilitation: An Italian Study. Arch Phys Med Rehabil. 2005;86:512-6.
- [CrossRef] [PubMed] [Google Scholar]
- Mortality after spinal cord injury: An 11-year prospective study. Arch Phys Med Rehabil. 1997;78:815-21.
- [CrossRef] [PubMed] [Google Scholar]
- National Institutes of Health. What are the Treatments for Spinal Cord Injury (SCI)?. United States: US Department of Health and Human Services; Available from: https://www.nichd.nih.gov/health/topics/spinalinjury/clinicaltrials/default [Last accessed on 2021 Apr 02]
- [Google Scholar]
- Aging with spinal cord injury. Phys Med Rehabil Clin N Am. 2017;28:821-8.
- [CrossRef] [PubMed] [Google Scholar]
- The need for a multidisciplinary outreach service for people with spinal cord injury living in the community. Clin Rehabil. 2001;15:600-6.
- [CrossRef] [PubMed] [Google Scholar]
- The health and life priorities of individuals with spinal cord injury: A systematic review. J Neurotrauma. 2012;29:1548-55.
- [CrossRef] [PubMed] [Google Scholar]
- Who wants to walk? Preferences for recovery after SCI: A longitudinal and cross-sectional study. Spinal Cord. 2008;46:500-6.
- [CrossRef] [PubMed] [Google Scholar]
- Determining priorities in functional rehabilitation related to quality of life one-year following a traumatic spinal cord injury. J Spinal Cord Med. 2020;43:241-6.
- [CrossRef] [PubMed] [Google Scholar]
- Trends in cancer survival by health insurance status in California from 1997 to 2014. JAMA Oncol. 2018;4:317-23.
- [CrossRef] [PubMed] [Google Scholar]
- Disparities in quality of cancer care. Medicine (Baltimore). 2017;96:e9125.
- [CrossRef] [PubMed] [Google Scholar]
- An official American thoracic society systematic review: Insurance status and disparities in lung cancer practices and outcomes. Am J Respir Crit Care Med. 2010;182:1195-205.
- [CrossRef] [PubMed] [Google Scholar]
- Primary payer status affects outcomes for cardiac valve operations. J Am Coll Surg. 2011;212:759-67.
- [CrossRef] [PubMed] [Google Scholar]
- Medicaid insurance as primary payer predicts increased mortality after total hip replacement in the state inpatient databases of California, Florida and New York. J Clin Anesth. 2017;43:24-32.
- [CrossRef] [PubMed] [Google Scholar]
- Changes in medicaid physician fees and patterns of ambulatory care. Inquiry. 2017;46:291-304.
- [CrossRef] [PubMed] [Google Scholar]
- Access to primary care physicians differs by health insurance coverage in mississippi. South Med J. 2014;107:87-90.
- [CrossRef] [PubMed] [Google Scholar]
- Characteristics of office-based physicians and their practices: United States, 2003-04. Vital Health Stat 13. 2007;164:1-34.
- [Google Scholar]
- The differential effect of compensation structures on the likelihood that firms accept new patients by insurance type. Int J Heal Econ Manag. 2016;16:65-88.
- [CrossRef] [PubMed] [Google Scholar]
- Does specialized inpatient rehabilitation affect whether or not people with traumatic spinal cord injury return home? J Neurotrauma. 2017;34:2867-6.
- [CrossRef] [PubMed] [Google Scholar]
- Spinal Cord Injury. Geneva: World Health Organization; Available from: https://www.who.int/en/news-room/fact-sheets/detail/spinal-cord-injury [Last accessed on 2022 Mar 30]
- [Google Scholar]






