Translate this page into:
Clinical Evaluation and Diagnostic Utilities of Different Nerve Conduction Tests in 100 Patients with Carpal Tunnel Syndrome
Address for correspondence: Dr. Rameshwar Nath Chaurasia, Department of Neurology, Institute of Medical Science, Banaras Hindu University, Varanasi - 221 005, Uttar Pradesh, India. E-mail: goforrameshwar@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background and Purpose:
The purpose of the study is to determine whether the clinical profile of patients with carpal tunnel syndrome (CTS) has been same over the years with the help of routine and comparative electrodiagnostic tests.
Methods:
A prospective study of 100 patients with suspected CTS was conducted without controls. Three provocative maneuvers were performed. Routine and comparison nerve conduction tests were performed, i.e., second lumbrical interossei motor latency difference (2 LIMLD), digit 4 median-ulnar sensory latency difference (D4MUSLD), palm wrist distal sensory latency difference (PWDSLD), and digit 1 median-radial sensory latency difference (D1MRSLD). Data entry, analysis, and statistical evaluation were done using International Business Machines Corporation Statistical Package for the Social Sciences statistics package (IBM, SPSS).
Results:
A total of 195 hands of 100 patients met the criteria for CTS. Forty-three percentage of patients were homemakers. Considering the rapidly changing communication technology, we observed 84% patients had aggravation of symptoms with continuous long-term daily mobile phone use (>30 min per session per day). We noted positive Tinel's sign in only 25%. Phalen's sign was positive in 53 right hands with mean duration of 11.49s (standard deviation [SD] ± 2.54 s) and was positive in 26 left hands with mean being 10.4 s (SD ± 1.91 s). The mean motor distal latency of median was 4.67 ms (SD ± 1.71 ms) and mean sensory distal latency of median was 3.24 ms (SD ± 1 ms). On internal comparison testing, mean difference in 2 LIMLD was 0.7 ± 0.3 ms, in D4MUSLD was 0.81 ± 0.32, in PWDSLD was 0.71 ± 0.20, and in D1MRSLD was 0.76 ± 0.32.
Conclusion:
Further analysis of clinical profile needs to be done, and new risk or provoking factors should be analyzed in patients with CTS.
Keywords
Carpal tunnel syndrome
electrodiagnostic studies
electromyography
occupations
INTRODUCTION
Carpal tunnel syndrome (CTS) is the most common peripheral nerve problem and most common entrapment neuropathy around the globe and has considerable employment and healthcare costs. If recognized early, it is readily treatable.[1] CTS is believed to be present in 3.8% of the general population. Incidence rates of up to 276:100,000/year have been reported,[2] with a prevalence rate up to 9.2% in women and 6% in men.[3] More common in females than in males, its occurrence is commonly bilaterally with a peak age range of 40–60 years although it occurs in all age groups. Primary features of CTS include pain in the hand, unpleasant tingling, pain or numbness in the distal distribution of the median nerve (thumb, index, middle finger, and the radial side of the ring finger), and a reduction of the grip strength and function of the affected hand. Symptoms tend to be worse at night, and clumsiness is reported during the day with activities requiring wrist flexion. Patients often describe a phenomenon termed the “flick sign,” in which shaking or flicking their wrists relieves symptoms.[456] The diagnostic signs include sensory loss along the lateral aspect of the hand, motor weakness and wasting of abductor pollicis brevis (APB) muscle, and eliciting Tinel's and Phalen's sign at the wrist. Nerve conduction studies (NCS) have been developed as a result of the discovery in 1956 that median nerve conduction times are slowed across the wrists of hands in CTS patients.[7] Prolonged motor and sensory latencies of the median nerve and reduced sensory and motor conduction velocities are accepted as diagnostic criteria for CTS. Even so, some authors have recently reported that optimal diagnostic criteria still remain uncertain.[8] The NCS and electromyography (EMG) demonstrate a distal lesion of the median nerve and help excluding other peripheral conditions resulting in similar symptoms.
METHODS
The present study was conducted in Department of Neurology, Institute of Medical Sciences, Banaras Hindu University, Varanasi, Uttar Pradesh, India, from October 2014 to March 2016. It was a prospective study of 100 consecutive patients referred from general medicine, orthopedic and rheumatology outpatient department with a suspected diagnosis of CTS. Patients undergoing tests were asked the clinical details such as age, gender, predominant symptom and hand involvement, progression, duration, aggravation and relieving factors, and preexisting illnesses.
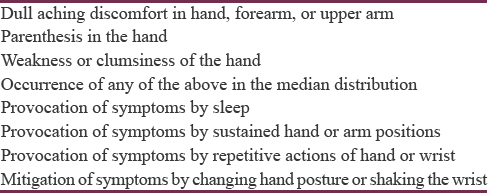
Patients with history or clinical examination or investigations suggestive of cervical radiculopathy (C6, C7, C8), brachial plexopathy, proximal median neuropathy, motor neuron disease, spondylotic myelopathy, syringomyelia, stroke, multiple sclerosis, and polyneuropathy without fulfilling CTS criteria were excluded from the study. Acute and chronic demyelinating polyneuropathy were also excluded in view of the possibility of focal conduction blocks in the distal part of the nerves. Patients fulfilling the following clinical criteria as in Table 1[9] for symptomatology were subjected to further electrodiagnostic (EDX) tests.
Electrodiagnostic studies
EDX studies were performed using Medelek synergy EMG machine. All studies were performed in a warm room. The skin temperature was maintained at >33°C. The motor and sensory median and ulnar NCS of both upper limbs were performed in all participants. For each reading, averaging of 20 stimuli was done. For motor NCS, the median and ulnar motor nerves were stimulated at wrist preferably 5–6 cm proximal to the active recording electrode. The sensory responses were obtained at digit II and digit V for the median and ulnar nerves, stimulating orthodromically at 11–12 cm and 9–10 cm, respectively. The normative value in our laboratory for median motor latency is <4.5 ms and median sensory distal peak latency <4 ms (millisecond). For internal comparison testing, four EDX tests were performed:
-
Second lumbrical-interossei motor latency difference (2 LIMLD)
-
Digit 4 median-ulnar sensory latency difference (D4MUSLD)
-
Palm wrist distal sensory latency difference (PWDSLD)
-
Digit 1 median-radial sensory latency difference (D1MRSLD).
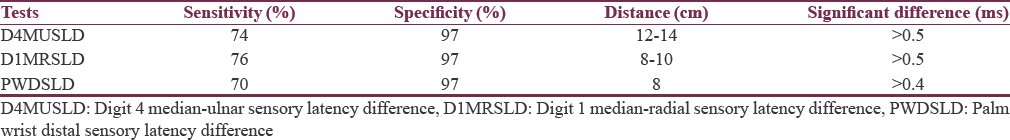
The parameters for internal comparison studies were provided as per AANEM as mentioned in Table 2.[10]
The grades of CTS on EDX were as follows:[11]
-
Grade 1 - CTS demonstrable only with most sensitive tests
-
Grade 2 - Sensory nerve conduction velocity slow on finger/wrist measurement, normal terminal motor latency
-
Grade 3 - Sensory potential slow but preserved with motor slowing, distal motor latency to APB <6.5 ms
-
Grade 4 - Sensory potentials absent but motor response preserved, distal motor latency to APB <6.5 ms
-
Grade 5 - Terminal latency to APB >6.5 ms
-
Grade 6 - Sensory and motor potentials effectively unrecordable.
RESULTS
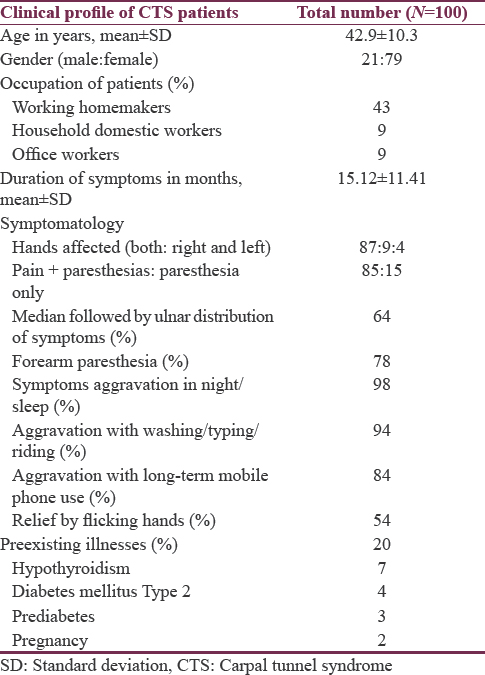
Of the total 100 patients and 200 hands tested, 195 hands were found to have CTS electrophysiologically. The mean of the presentation was 42.9 years with standard deviation (SD) 10.3. The youngest patient was 23 years and oldest at 70 years. Grade 3 of CTS was most common in all age groups of the study patients. Seventy-nine percentage of our patients were females, and as far as occupation was concerned, the majority were working housewives (43%) of the overall patients. The most common symptom noted was paresthesia and pain combined (85%) followed by paresthesia and usually involved both hands on presentation, although, asymmetrically. Paresthesia distribution was started in median followed in ulnar distribution in 64% patients and forearm paresthesias were noted in 78% of the patients, respectively. Nearly, 98% of the patients reported night time aggravation of symptoms in initial course of illness which however was lost in later part in the longer course. Duration of symptoms in our patients ranged from 4 to 60 months with mean duration being 15.12 months and SD ± 11.41 months. Various aggravating factors which cause repetitive movements at wrist such as washing clothes/utensils, riding bike, and prolonged hand typing precipitated symptoms in 94% of the patients. We noticed aggravation with long-term continuous mobile use (>30 min) per day in 84% of the patients, and in some patients, even as the reason for first noticing the symptoms. Relief by flicking hands was noted in 54% of the patients. Preexisting associated illnesses were noted in only 20% of the patients of which the most common was hypothyroidism (1.4%) [Table 3].
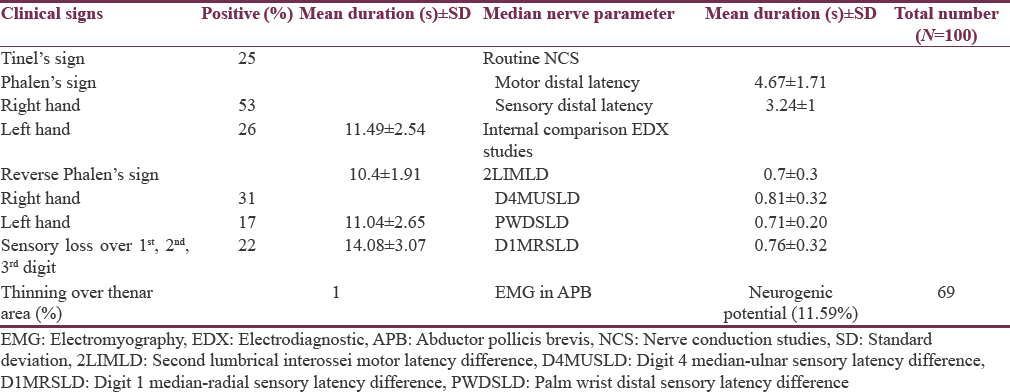
On examination, positive Tinel's sign was noted in only 25% of the patients. Phalen's sign was tested in all the patients of whom 53 had positive response in right hand for which mean of the duration for positive response was 11.49 s with SD ± 2.54 s and was positive in 26 left hands with mean being 10.4 s and SD ± 1.91 s. As far as reverse Phalen's sign is concerned, it was tested positive in 31 right hands with mean duration 11.04 s (SD ± 2.65) and in 17 left hands with mean duration 14.08 s (SD ± 3.07). Sensory loss over 1st, 2nd, and 3rd digits was noted in 22% of the patients and thinning of thenar eminence was noted in only one patient who was a homemaker and later on found to have Grade 6 CTS. NCS and Internal comparision studies testing was done in total 200 hands (100 right and 100 left) in which most common grade was CTS Grade 3 found in 77% in right hands and 60% in left hands. Second most common grade in right hand was Grade 4 and in left hand was Grade 2. Normal NCS were found in three right hands and two left hands. On routine NCS testing, the mean motor distal latency of median was 4.67 ms (SD ± 1.71 ms) and mean sensory distal latency of median was 3.24 ms (SD ± 1 ms). The internal comparison EDX tests (1 motor, 3 sensory) showed motor latency difference between median and ulnar on 2 LIMLD as mean 0.7 ms (SD ± 0.3) and mean sensory latency difference in millisecond on D4MUSLD as 0.81 (SD ± 0.32), PWDSLD as 0.71 (SD ± 0.20), and D1MRSLD as 0.76 (SD ± 0.32). We performed EMG as per the AAN guidelines in 69 patients to rule out proximal median neuropathy or other proximal lesions and found to be neurogenic pattern in 11.59% in APB with sparing of other proximal muscles suggesting active denervation and reinnervation in these patients in the distribution of median nerve distal to carpal tunnel [Table 4]. The erythrocyte sedimentation rate was almost normal in all the patients, mean being 29.33 at the end of 1st h (SD ± 8.86), with only one patient with abnormal value, i.e., 62, who later on was found to have paraproteinemia. The mean hemoglobin level was 12.8 g/dl with SD ± 1.38. On testing for diabetes mellitus, 6 were detected to be diabetic (4 were previously known to have type 2 diabetes mellitus) and 19 were found to have prediabetes (impaired glucose tolerance test [GTT]). Twenty-one patients had thyroid-stimulating hormone (TSH) level more than 5.5 of which 7 were previously known to be hypothyroid. Three patients were found to have associated peripheral neuropathy and one patient was found to have paraproteinemia.
DISCUSSION
CTS is the most common entrapment neuropathy of the upper limb, with a reported prevalence of 6% in the general population.[1213] Seventy-nine percentage patients in our study were females and most common age group affected was 30–50 years with mean age being 42.9 (±10.3 SD) as compared to previous studies.[14] Very few of the previous studies have reported working homemakers as predominantly affected group with CTS. In our study of 100 patients, most common association of CTS with occupation was noted in working homemakers, i.e., 43% of the patients followed by 9% in household workers i.e., maids. In Europe, in 1998, over 60% of upper limb musculoskeletal disorders recognized as work related were CTS cases.[1516] Manual workers such as those involved in construction,[1718] manufacturing,[18] and homemakers[19] have found to have higher incidence of CTS. As studied by Mattioli et al., full-time homemakers were found to have higher incidence and risks as compared to other well-defined risk professions.[19] This part could be due to previous negligence and attribution of symptoms to other causes such as cervical spondylosis or nonspecific musculoskeletal pain. Duration of symptoms in our patients ranged from 4 to 60 months with mean duration being 15.12 months and SD ± 11.41 months as compared to previous studies which reported average duration to be 12 months. Eighty-seven percentage patients in our study had bilateral CTS which is higher than reported study.[20] Eighty-five percentage of the patients in our study had pain and paresthesia combined, while previous studies have reported predominant paresthesia and numbness rather than pain, as predominant symptom.[2122] Aggravation of complaints in night was seen in 98% of the patients. CTS are known to be associated with risk factors which cause repetitive movements or persistent posturing at wrist. We observed different aggravating factors which cause repetitive movements at wrist such as washing clothes or utensils or riding bike or prolonged typing precipitated symptoms in 94% of the patients in our study. In our study, we also observed aggravation with long-term continuous mobile use (>30 min) per day in 84% of the patients, and in some patients, even as the reason for first noticing the symptoms. Fifty-four percentage of the patients had relief in the symptoms by flicking the hands. The symptoms and risk have been previously described in persons who use computer mouse for long time (>8 h).[23] We, however, have observed the presentation of the symptoms with long mobile use and aggravation by it too. With the recent flooding of smartphones in our lives, which are relatively heavier, this could be an important correlating factor. As this was a mere observation, direct causation or risk stratification cannot be commented upon yet. The reported specificity and sensitivity of the Tinel's test varies wildly in the literature. Sensitivities of 23%–67% and specificities of 55%–100% have been reported, these variations may well be due to differences in technique.[24252627] The sensitivity and specificity of the Phalen's test has been reported at between 10% and 91% and 33%–100%, respectively.[24252627] In our study, positive Tinel's sign was noted in only 25% of the patients. Phalen's and reverse Phalen's sign is to be tested for 1 min,[24252627] however, in our study, we noticed positive response in <20 s only. Possible explanation could be that pressure in carpal tunnel significantly increases in 10 s and reaches plateau in 20–30 s.[28] Sensory loss over 1st, 2nd, and 3rd digit was noted in 22% of the patients. Sensory examination assessing for features such as hypoalgesia or diminished two-point discrimination are again specific, but not sensitive for the diagnosis of CTS.[29] On testing for diabetes mellitus, 6 were detected to be diabetic (4 were previously known to have type 2 diabetes mellitus) and 19 were found to have prediabetes (impaired GTT). Twenty-one patients had TSH level more than 5.5 of which 7 were previously known to be hypothyroid. Three patients were found to have associated peripheral neuropathy and one patient was found to have paraproteinemia. As per previous literature, diabetic patients have a prevalence rate of 14% and 30% without and with diabetic neuropathy, respectively,[30] while the prevalence of CTS during pregnancy has been reported to be around 2%.[31] NCS is considered to be the gold standard in the diagnosis of CTS because it is an objective test that provides information on the physiological health of the median nerve across the carpal tunnel.[32] The use of a relative comparison of two nerve segments controls these factors. We found that most common grade was CTS Grade 3 found in 77% in right hands and in 60% in left hands. Second most common grade in right hand was Grade 4 and in left hand was Grade 2. Normal NCS were found in three right hands and two left hands. We performed EMG as per the AAN guidelines in 69 patients to rule out proximal median neuropathy or other proximal lesions and found to be neurogenic pattern in 11.59% in APB with sparing of other proximal muscles suggesting active denervation and reinnervation in these patients in the distribution of median nerve distal to carpal tunnel. Data from previous studies about such EMG profile are not available. On routine nerve conduction testing we performed, the mean motor distal latency of median was 4.67 ms (SD ± 1.71 ms) and mean sensory distal latency of median was 3.24 ms (SD ± 1 ms). On internal comparison testing, mean difference in 2 LIMLD was 0.7 ± 0.3 ms, in D4MUSLD was 0.81 ± 0.32, in PWDSLD was 0.71 ± 0.20, and in D1MRSLD was 0.76 ± 0.32. In previous study, mean value for 2 LIIMLD noted was 2.29 ± 1.72 ms and that for PWDSLD was 0.94 ± 0.63 ms.[33] However, data for analysis of other two comparison tests D4MUSLD and D1MRSLD were not found in previous literature. As clinical symptoms were found to be more severe with higher grades of CTS, similarly severity of symptoms was noticed with higher latency difference on internal comparison tests. The treatment aspect and follow-up of the patients were not studied due to improper compliance, which shall be our next plan of action in due course.
CONCLUSION
We have highlighted a few differences in demographic profile of the patients in our study as compared to previously reported studies. Working homemakers stand equal chance of suffering from morbidity of CTS as compared to other high risk professions. In the light of advances in technologies and communications, fresh views and open mind are needed to look for new risk factors. We have tried to provide the widest range of clinical and electrophysiological data from North India on patients with CTS so that further aspects of this morbid disorder can be studied.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- The first description of carpal tunnel syndrome. J Hand Surg Eur Vol. 2007;32:195-7.
- [Google Scholar]
- Carpal tunnel syndrome surgery in France in 2008: Patients’ characteristics and management. Rev Neurol (Paris). 2011;167:905-15.
- [Google Scholar]
- Diagnosis, treatment and follow-up of the carpal tunnel syndrome: A review. Neurol Sci. 2010;31:243-52.
- [Google Scholar]
- An assessment of the sympathetic function within the hand in patients with carpal tunnel syndrome. J Hand Surg Eur Vol. 2010;35:402-8.
- [Google Scholar]
- The flick sign in carpal tunnel syndrome. J Neurol Neurosurg Psychiatry. 1986;49:220-1.
- [Google Scholar]
- Electrical signs in the diagnosis of carpal tunnel and related syndromes. J Neurol Neurosurg Psychiatry. 1956;19:275-80.
- [Google Scholar]
- Practice parameter for carpal tunnel syndrome (summary statement). Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 1993;43:2406-9.
- [Google Scholar]
- American Association of Electrodiagnostic Medicine, American Academy of Neurology, and American Academy of Physical Medicine and Rehabilitation. Practice parameter for electrodiagnostic studies in carpal tunnel syndrome: Summary statement. Muscle Nerve. 2002;25:918-22.
- [Google Scholar]
- A neurophysiological grading scale for carpal tunnel syndrome. Muscle Nerve. 2000;23:1280-3.
- [Google Scholar]
- Carpal tunnel syndrome: Prevalence in the general population. J Clin Epidemiol. 1992;45:373-6.
- [Google Scholar]
- The carpal-tunnel syndrome. Seventeen years’ experience in diagnosis and treatment of six hundred fifty-four hands. J Bone Joint Surg Am. 1966;48:211-28.
- [Google Scholar]
- Exposure-response relationship in the hand-arm vibration syndrome: An overview of current epidemiology research. Int Arch Occup Environ Health. 1998;71:509-19.
- [Google Scholar]
- Epidemiology of musculoskeletal disorders due to biomechanical overload. Ergonomics. 1998;41:1253-60.
- [Google Scholar]
- Risk factors for carpal tunnel syndrome and median neuropathy in a working population. J Occup Environ Med. 2008;50:1355-64.
- [Google Scholar]
- Attributable risk of carpal tunnel syndrome according to industry and occupation in a general population. Arthritis Rheum. 2008;59:1341-8.
- [Google Scholar]
- Incidence rates of surgically treated idiopathic carpal tunnel syndrome in blue- and white-collar workers and housewives in Tuscany, Italy. Occup Environ Med. 2009;66:299-304.
- [Google Scholar]
- Carpal tunnel syndrome: A series observed at Jordan University Hospital (JUH), June 1999-December 2000. Clin Neurol Neurosurg. 2002;104:49-53.
- [Google Scholar]
- Clinical profile, electrodiagnosis and outcome in patients with carpal tunnel syndrome: A Singapore perspective. Singapore Med J. 2006;47:1049-52.
- [Google Scholar]
- Current concepts in carpal tunnel syndrome: A review of the literature. Eur J Orthop Surg Traumatol. 2010;20:445-52.
- [Google Scholar]
- Computer use and carpal tunnel syndrome: A 1-year follow-up study. JAMA. 2003;289:2963-9.
- [Google Scholar]
- Sensitivity and specificity of carpal tunnel syndrome signs. Am J Phys Med Rehabil. 1997;76:451-7.
- [Google Scholar]
- What is the diagnostic value of ultrasonography compared to physical evaluation in patients with idiopathic carpal tunnel syndrome? Clin Exp Rheumatol. 2007;25:853-9.
- [Google Scholar]
- Hand elevation test for assessment of carpal tunnel syndrome. J Hand Surg Br. 2005;30:361-4.
- [Google Scholar]
- Electrodiagnostic approach to carpal tunnel syndrome. Ann Indian Acad Neurol. 2006;9:177-82.
- [Google Scholar]
- Carpal tunnel syndrome in patients with diabetic polyneuropathy. Diabetes Care. 2002;25:565-9.
- [Google Scholar]
- Carpal tunnel syndrome during pregnancy. Scand J Plast Reconstr Surg Hand Surg. 2006;40:41-5.
- [Google Scholar]
- Carpal tunnel syndrome: Pathophysiology and clinical neurophysiology. Clin Neurophysiol. 2002;113:1373-81.
- [Google Scholar]
- Comparison of high-resolution sonography and electrophysiology in the diagnosis of carpal tunnel syndrome. Ann Indian Acad Neurol. 2015;18:219-25.
- [Google Scholar]






