Translate this page into:
Cerebral Arteriovenous Malformation Associated with a Cyst
Address for correspondence: Dr. Batuk Diyora, Department of Neurosurgery, LTMMC and LTMG Hospital, Sion, Mumbai - 400 022, Maharashtra, India. E-mail: bddiyora@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
An 11-year-old child presented with chronic occipital headache and vomiting. Computed tomography (CT) scan revealed a cystic mass lesion in the right occipital region. Magnetic resonance imaging brain revealed a cystic mass lesion which was hypointense on T1-weighted images and hyperintense on T2-weighted images. A mural nodule was noted in the inferolateral wall of the lesion. CT angiography revealed small arteriovenous malformations (AVM) related to the lesion. The AVM associated with the cyst was excised. The patient recovered well. Cystic AVM is a rare vascular lesion, and only five such cases have been reported in the past. AVMs should be considered in the differential diagnosis of cystic lesions of the brain, especially when associated with a mural nodule.
Keywords
Arteriovenous malformation
cystic lesion
occipital headache
INTRODUCTION
Arteriovenous malformations (AVMs) of the brain are focal abnormal conglomerations of dilated arteries and veins within the brain parenchyma, in which loss of normal vascular organization at the subarteriolar level and lack of a capillary bed result in abnormal arteriovenous shunting.[1] More than 50% AVMs present with intracranial hemorrhage.[2] Next most common presentation being seizures which occurs in ≈20% to 25% of cases.[3] Other presentations include headache (15% of cases) and focal neurological deficits (<5% of cases). An association of a cyst with an AVM is rare. We present a case of cerebral cystic AVM.
CASE REPORT
An 11-year-old child was admitted for complaints of severe headache for 3–4 months. Headache was insidious in onset and more pronounced over the occipital region. He also reported vomiting for 3–4 days. He had no convulsions or vision complaints. Neurological examination revealed no abnormalities except some field defect. Computerized perimetry revealed right homonymous hemianopia. Computed tomography scan showed a 2.1 cm × 2.8 cm × 2.7 cm sized cystic lesion in the right occipital lobe [Figure 1]. Magnetic resonance imaging (MRI) revealed a well-defined predominantly cystic appearing lesion in the right occipital lobe which was homogenously hypointense on T1-weighted images and homogenously hyperintense on T2-weighted images [Figure 2a-c]. It also revealed a small eccentric hypointense mural nodule along the inferolateral wall, which appeared as blooming on gradient recalled echo sequences, indicating that it was probably calcified. An absence of perifocal edema was noted. The cyst wall and nodule showed minimal enhancement on contrast MRI studies. MR angiography showed a cluster of abnormal serpiginous vessels along the inferior aspect of the lesion. The vessels were found to be arising from the right posterior cerebral artery and were reaching up to the eccentric nodule [Figure 2d].
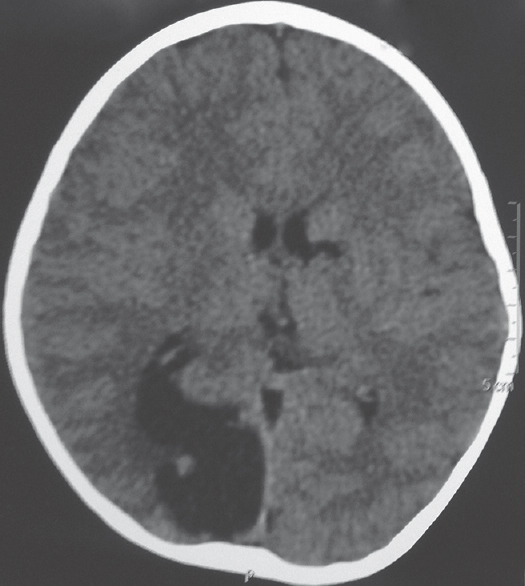
- Computed tomography showing 2.1 cm × 2.8 cm × 2.7 cm sized cystic lesion in the right occipital lobe with small nodule
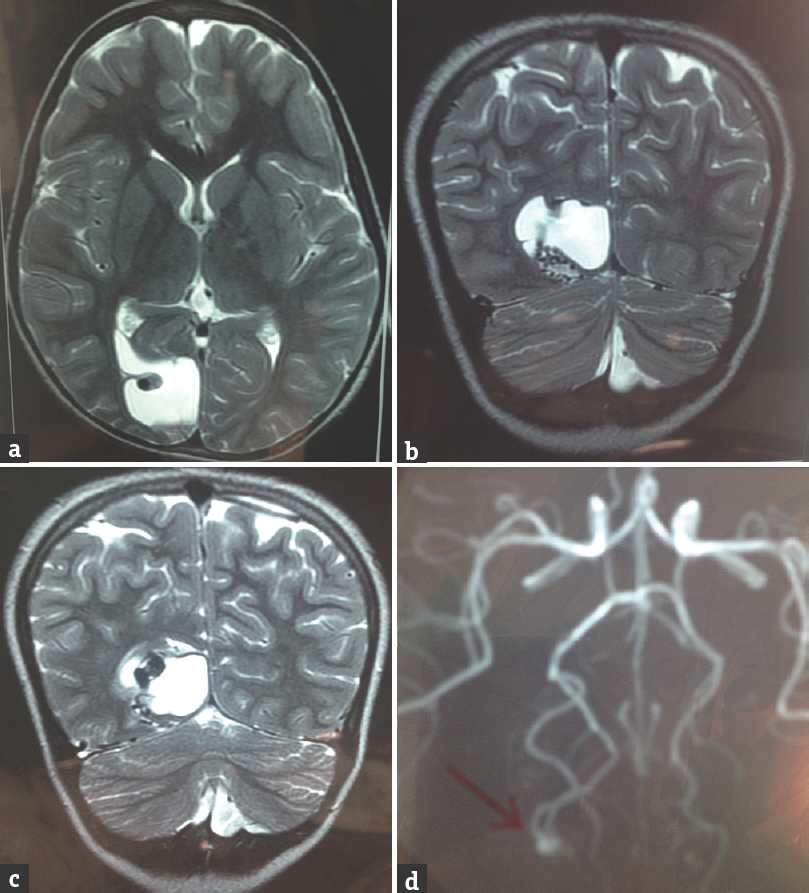
- Magnetic resonance imaging showed well-defined predominantly cystic appearing lesion in right occipital lobe which was homogenous hyperintense on T2-weighted images axial view (a) and coronal view (b and c). It revealed small eccentric hypointense mural nodule along inferolateral lateral wall. Magnetic resonance angiography revealed cluster of abnormal serpiginous vessels along the inferior aspect of this lesion arising from right principal component analysis and were reaching up to eccentric nodule (d)
The patient underwent right parieto-occipital craniotomy. The cyst was extending to the surface, and approximately 30 cc of straw-colored fluid was tapped and aspirated. On opening the cyst wall, a reddish mural nodule was observed along its lateral wall. The cyst along with the nidus was completely excised. Histopathological examination revealed AVM. The postoperative period was uneventful. There was no deterioration in vision, and the headache was relieved postsurgery.
DISCUSSION
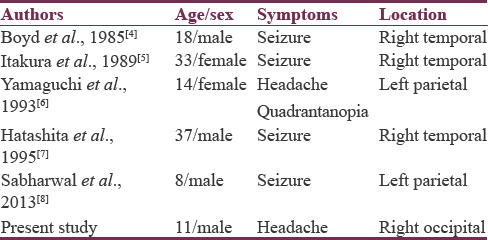
Cystic AVMs are a rare occurrence. Literature search revealed only five such reported cases [Table 1].[45678] Among the six cases (including ours), there were two female and four male patients. Two belonged to the pediatric age group and the rest were adults with ages ranging from 14 to 38 years, with an average age of 20 years. Of the six patients, three presented with seizures, one with headache, and one with focal neurological deficit in the form of visual field loss. Our patient presented with headache, vomiting, and homonymous hemianopia. The right temporal lobe was observed to be the most commonly involved lobe (in three patients), the left parietal lobe was the second most common to be affected (in two patients), and our patient had right occipital lobe involvement – the only patient having cystic AVM in the right occipital lobe. The cysts in four patients contained xanthochromic fluid and in two patients contained blood. Successful total resection was done in all cases and good neurological outcome was achieved.
Two types of cyst have being described in the literature[45] – slit type and round type. The former occurs as a result of prolonged degeneration of multiple small hemorrhages into xanthochromic fluid. These patients usually have a history of recurrent headache. The latter usually results from exudation of fluid from the mural nodule associated with the AVM. These patients do not have recurrent headaches. Hatashita et al.[7] studied the histology of the cyst wall and showed numerous thin-walled vascular channels and deposits of fibrous tissue, which are also seen in the membrane of the giant cysts associated with cavernous angiomas. This hence suggested the formation of a capsule around a minor hemorrhage from the AVM which in turn resulted in a cyst formation. The growth of such a cyst was a result of repeated subclinical hemorrhages from the neovascular channels of the cyst wall.
In our patient, the cyst was round and contained straw-colored fluid which was exuded from the mural nodule as per the theory put forward by Itakura et al.[5] In contrast to the popular belief of the existence of severe headache in patients with slit-like cysts filled with xanthochromic fluid, our patient who had a round cyst filled with straw-colored fluid also exhibited severe headache. This proved the existence of other developmental mechanisms which need to be further explored.
We hence conclude that AVMs associated with cysts as well as those which occur secondary to repeated microhemorrhages or exudation of fluid from mural nodules are an uncommon finding. Total resection should be attempted as it can lead to a complete cure.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Frequency of intracranial hemorrhage as a presenting symptom and subtype analysis: A population-based study of intracranial vascular malformations in Olmsted country, Minnesota. J Neurosurg. 1996;85:29-32.
- [Google Scholar]
- The natural history of unruptured intracranial arteriovenous malformations. J Neurosurg. 1988;68:352-7.
- [Google Scholar]
- Familial arteriovenous malformations. Report of four cases in one family. J Neurosurg. 1985;62:597-9.
- [Google Scholar]
- Cystic arteriovenous malformation. A case report. Acta Neurochir (Wien). 1989;96:154-8.
- [Google Scholar]
- A case of arteriovenous malformation with cyst formation. No Shinkei Geka. 1993;21:453-7.
- [Google Scholar]
- Arteriovenous malformation associated with a large cyst – Case report. Neurol Med Chir (Tokyo). 1995;35:377-9.
- [Google Scholar]
- Arteriovenous malformation associated with cyst in a child: Case report and review of literature. J Pediatr Neurosci. 2013;8:126-8.
- [Google Scholar]






