Translate this page into:
Cerebellar Cystic Oligodendroglioma in a Young Adult
Address for correspondence: Dr. Mukesh Kumar Bhaskar, Department of Neurosurgery, King Gerorge's Medical University, Lucknow - 226 003, Uttar Pradesh, India. E-mail: drmannu84@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Oligodendrogliomas are tumors of glial cells, and they represent approximately 4%–5% of all primary brain tumors.[1] The majority of oligodendrogliomas are supratentorial (>90%) and infrequently encountered in the posterior fossa.[23] Infratentorial cystic oligodendrogliomas are very uncommon, and most of them belong to pediatric age group. We report a cerebellar cystic oligodendroglioma in a young adult.
A 36-year-old male presented with a history of headache and vertigo of 1-month duration. Neurological examination showed impaired tandem gait with no other neurological deficits. Noncontrast and contrast computed tomography of the head revealed a large, well-defined, hypodense vermian lesion, with areas of patchy contrast enhancement [Figure 1a and b]. No evidence of calcification noted. Magnetic resonance imaging (MRI) showed a large inhomogeneous solid cystic lesion. The large cystic component is hypointense on T1-weighted images and hyperintense on T2-weighted images whereas small solid component is isointense on T1-weighted images and hypointense on T2-weighted images. On contrast study, only solid component showed heterogeneous enhancement with evidence of blooming on susceptibility-weighted images (SWI) [Figure 1c-f]. A radiological impression of hemangioblastoma and the possibility of pilocytic astrocytoma was kept in mind, and the patient was prepared for surgery.
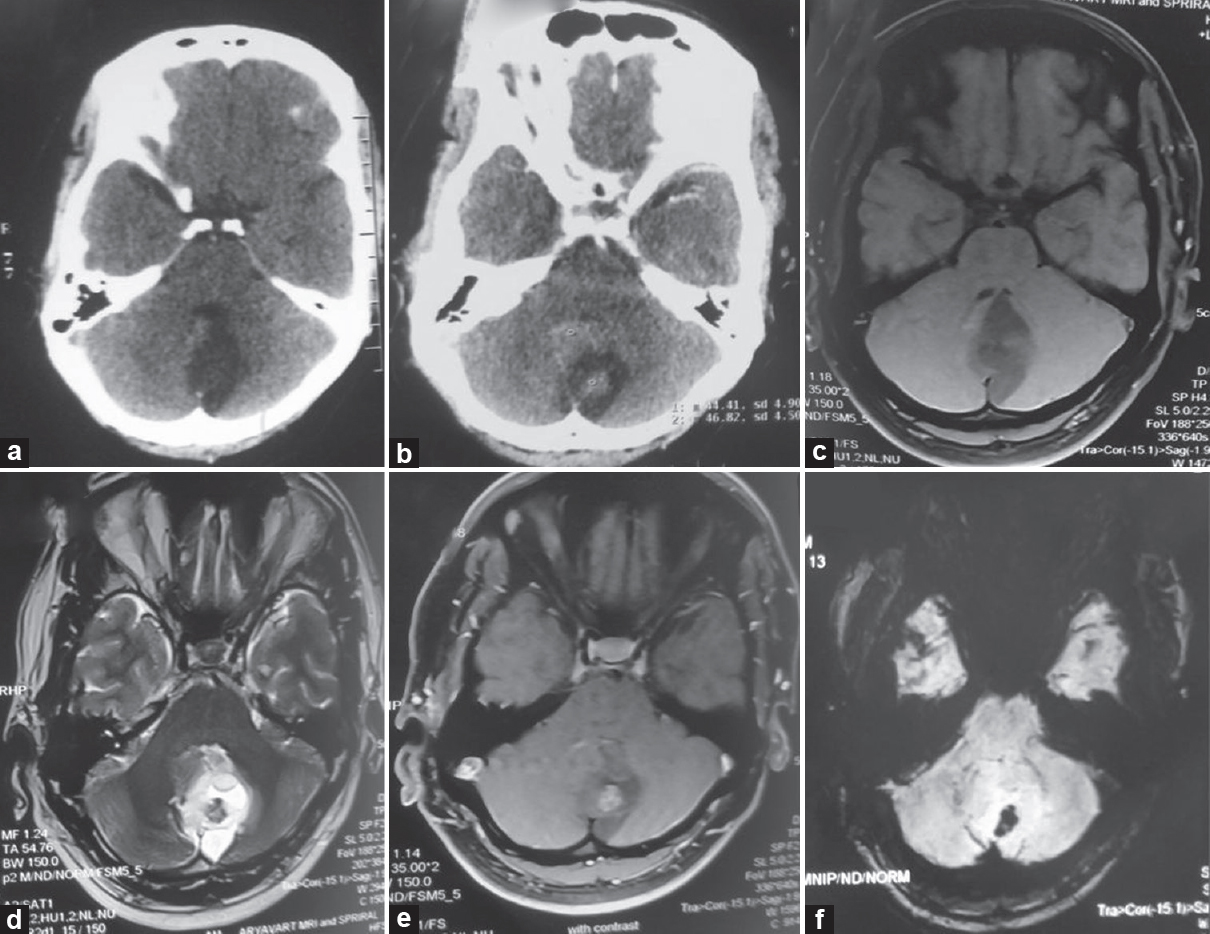
- (a and b) Plain and contrast computed tomography, (c-f) magnetic resonance imaging images (c) T1-weighted image, (d) T2 weighated image, (e) T1 contrast, (f) susceptibility-weighted image
A midline suboccipital craniectomy with complete excision of the lesion was performed, and postoperative recovery was uneventful. Histopathological examination (HPE) of the specimen showed a diffusely infiltrating glial neoplasm composed of monomorphic cells with uniform round vesicular nuclei, small distinct nucleoli, and a perinuclear halo interspersed by arborizing thin-walled blood vessels. The tumor cells were dispersed around ectatic dilated and congested blood vessels. Areas of necrosis were also evident at places [Figure 2d]. The proliferation fraction, as detected by Ki-67, was low (<1%). Immunohistochemistry (IHC) was performed for confirmation; the tumor cells were strongly positive for GFAP along with S-100 and negative for inhibin. Based on HPE and IHC, a diagnosis oligodendroglioma (WHO grade 2) was established. There was no evidence of clinicoradiological recurrence of the lesion at 6-month follow-up [Figure 2a-c]. Cystic cerebellar oligodendroglioma in adult has never been reported in the literature (PubMed search with key words “posterior fossa,” “cystic oligodendroglioma,” “adults”).
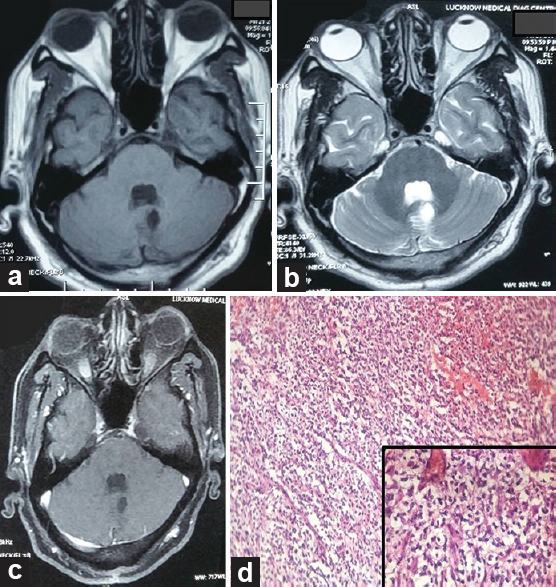
- (a-c) Follow-up magnetic resonance imaging (a) T1-weighted image, (b) T2-weighted image, (c) T1 contrast, (d) histopathological examination ×100 (inset ×400)
The symptoms of oligodendroglial tumors do not reliably distinguish them from other types of low-grade gliomas. The most common presenting symptom is seizures (generalized, simple partial, complex partial), ranging in incidence from 35% to 85% of patients.[4] Other presenting symptoms are headache, change mental status, visual complaints, nausea, vomiting, vertigo, and/or localized sensory/motor deficit.[45] The clinical course of oligodendroglioma in the posterior cranial fossa is relatively indolent, and symptoms (nausea, vomiting, and vertigo) are usually long standing.[6]
Radiological findings of oligodendrogliomas may be characteristic but are not pathognomonic. Usually, these tumors are found in the cortex and/or subcortical white matter with fairly discrete margins (49%–59%) and variable contrast enhancement.[4] Peritumoral edema and mass effect are usually minimal or absent despite the size of the tumor. On MRI, an oligodendroglioma is typically hypointense on T1-weighted images and hyperintense on T2-weighted images, often appearing fairly well demarcated.[47] The diagnosis of oligodendrogliomas is suggested preoperatively when intratumoral or peritumoral calcification is seen on neuroimaging (up to 90% cases).[47] Calcifications and enhancement are seen less frequently in children and adolescents with oligodendrogliomas than in adults.[4] However, posterior fossa oligodendrogliomas may not show characteristic imaging findings with occasional heterogeneous enhancement and absent or mild mass effect.[7] In our case, the tumor was largely cystic with small solid part, and contrast enhancement of solid part was seen along with blooming on SWI.
Oligodendrogliomas are treated by surgical excision with or without adjuvant radiation therapy based on multiple prognostic factors. Oligodendrogliomas seem to be more likely to metastasize outside the central nervous system (to bone, lung, pleura, and liver) than other gliomas.[4] Because of the tendency to metastasize through the cerebrospinal fluid, some authors recommended cerebrospinal fluid cytology in all cases to determine the need for spinal axis irradiation. Others suggest that the oligodendroglioma of the posterior fossa be considered potentially malignant and treat with local as well as prophylactic craniospinal radiotherapy.[6] Infratentorial oligodendrogliomas may be more aggressive and malignant than supratentorial ones.[28] Therefore, postoperative radiotherapy has been advocated in many reported evidence of infratentorial oligodendrogliomas. However, some continue to observe their patients for clinicoradiological recurrence before instituting radiotherapy (as in our case). The exact treatment protocols of posterior fossa oligodendroglioma are yet to be established due to the paucity of cases.
Financial support and sponsorship
This study was financially supported by Department of Neurosurgery, King George's Medical University, Lucknow - 226 003, Uttar Pradesh, India.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
I sincerely thank Professor B. K. Ojha, Professor Anil Chandra, Dr. C. Srivastava, Dr. Manish Jaiswal, and Dr. Somil Jaiswal for their constant support and help in preparation of the manuscript including submission procedures.
REFERENCES
- Infratentorial oligodendrogliomas: Imaging findings in six patients. Acta Radiol. 2010;51:213-7.
- [Google Scholar]
- Oligodendroglioma and anaplastic oligodendroglioma: Clinical features, treatment, and prognosis. Surg Neurol. 2003;60:443-56.
- [Google Scholar]
- Oligodendroglioma: An analysis of prognostic factors and treatment results. Am J Clin Oncol. 2000;23:170-5.
- [Google Scholar]
- Magnetic resonance features of the enigmatic oligodendroglioma. Invest Radiol. 1998;33:222-31.
- [Google Scholar]





