Translate this page into:
Arterial Dissection Following the Use of Remote Aspiration Thrombectomy
Address for correspondence: Dr. Min S. Park, Department of Neurosurgery, University of Virginia, Charlottesville, VA, USA. E-mail: mp2tq@hscmail.mcc.virginia.edu
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Remote aspiration thrombectomy using a balloon guide catheter for acute carotid artery occlusion has been proposed as a safe and effective technique. We present a case of iatrogenic arterial dissection of the distal cervical segment in a patient with proximal vessel occlusion who underwent attempted revascularization using this strategy. A 57-year-old male patient presented with computed tomography (CT) angiogram evidence of a left carotid terminus and M1 segment occlusion. The patient was taken emergently for mechanical thrombectomy. Remote aspiration thrombectomy was attempted twice using manual aspiration through a balloon guide catheter in the common carotid artery; however, this resulted in minimal recanalization of the carotid terminus and a new iatrogenic dissection within the internal carotid artery (ICA) just proximal to the skull base. Despite multiple additional attempts at mechanical thrombectomy, only limited recanalization of the ICA terminus and anterior cerebral artery distribution was achieved, with no significant flow past the M1 segment. After the procedure, a large ischemic territory within the left middle cerebral artery distribution consistent with the continued M1 segment occlusion was apparent on CT. The patient died on the poststroke day 6. Although remote aspiration thrombectomy for thromboemboli in this location has potential benefits, it should be used cautiously given the potential risk of injury to the proximal vasculature.
Keywords
Arterial dissection
balloon guide catheter
carotid artery occlusion
remote aspiration thrombectomy
thromboembolus
INTRODUCTION
The treatment of large vessel acute ischemic stroke continues to evolve and undergo refinement. Treatment for internal carotid artery (ICA) terminus occlusion has primarily centered on the use of stent retrievers, direct aspiration catheters, or a combination of these techniques.[1234] Recently, a novel treatment for these thromboemboli using remote aspiration through a balloon guide catheter inflated within the cervical segment of the ICA was reported with good results and no evidence of procedure-related complications.[5] We report a single case in which this technique was used but resulted in an iatrogenic arterial dissection within the distal cervical segment of the ICA that was not related to the catheter or wire manipulation.
CASE REPORT
A 57-year-old male with an extensive history of tobacco use was transferred to our institution with a left middle cerebral artery (MCA) syndrome and computed tomography (CT) angiogram evidence of a carotid terminus and M1 segment occlusion. The patient received intravenous tissue plasminogen activator at the outside institution within 90 min of his stroke onset. On arrival to our facility, within 2½ h of symptom onset, the patient's National Institutes of Health Stroke Scale score was 21. The initial CT of the head at the outside institution revealed an Alberta Stroke Program Early CT Score of 10.
The patient was taken emergently to the angiography suite for attempts at mechanical thrombectomy. After placement of an 8 French femoral sheath, the left ICA was accessed with an 8 French Flowgate balloon guide catheter (Stryker Neurovascular; Fremont, California) over a 6 French Penumbra Select Berenstein catheter (Penumbra Inc.; Alameda, California) over a Glidewire (Terumo; Somerset, New Jersey). The balloon guide catheter was positioned within the proximal cervical ICA. After removal of the Penumbra Select catheter and Glidewire, initial angiograms demonstrated a left supraclinoid ICA occlusion [Figure 1] without evidence of cervical ICA injury during catheter manipulations [Figure 2a and b].

- Initial lateral angiogram of the left internal carotid artery demonstrating occlusion of the supraclinoid segment of the carotid artery (arrow)
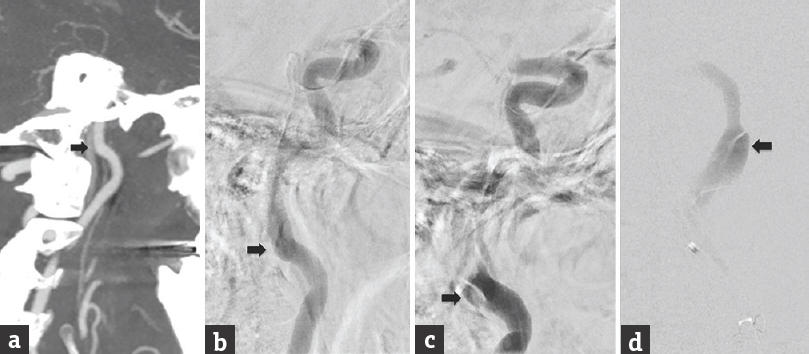
- (a) Preintervention lateral computed tomographic angiography of the neck demonstrating no dissection before intervention (arrow). (b) Initial lateral angiogram of the left internal carotid artery through the balloon guide catheter prior to proximal aspiration without evidence of dissection (arrow). (c) Immediate postproximal aspiration angiogram demonstrating a new, iatrogenic dissection of the cervical internal carotid artery (arrow). (d) Posteroanterior microcatheter angiogram of the left cervical internal carotid artery dissection (arrow) during initial intracranial navigation of the microcatheter and aspiration catheters
The balloon was inflated, and proximal aspiration thrombectomy was attempted twice using manual aspiration with a 60 mL syringe through the balloon guide catheter as described in the initial case report.[5] A follow-up angiogram after these two attempts demonstrated minimal recanalization of the ICA terminus; however, there was evidence of a new iatrogenic dissection within the ICA just proximal to the skull base [Figure 2c and d]. We proceeded with multiple attempts at mechanical thrombectomy using a combination of stent retrievers and direct aspiration at the clot face but were only able to achieve a modified thrombolysis in cerebral infarction (mTICI) grade 1 recanalization of the ICA terminus and anterior cerebral artery distribution [Figure 3]. There was no significant flow past the M1 segment.
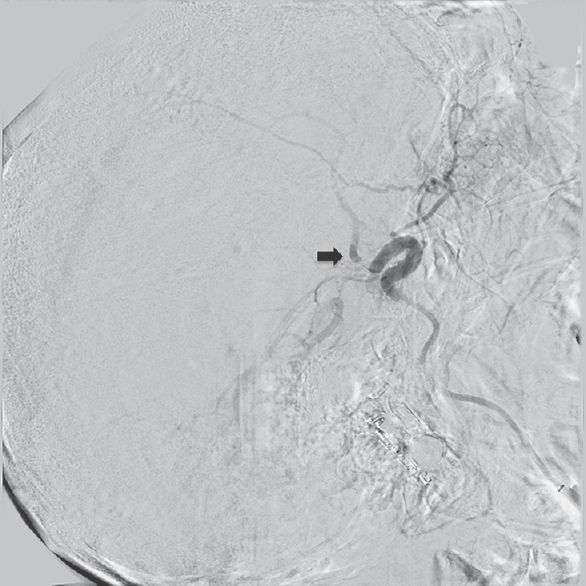
- Final lateral angiogram following balloon guide proximal aspiration and a combined stent retriever and direct aspiration technique demonstrating modified thrombolysis in cerebral infarction Grade 1 recanalization (arrow)
Following the procedure, the patient was admitted to the neurocritical care unit for observation. A follow-up CT head demonstrated a large ischemic territory within the left MCA distribution consistent with the continued M1 segment occlusion [Figure 4]. The patient's examination findings remained poor, with a dense left MCA syndrome. There was no significant improvement in the patient's neurological status during the hospitalization. After lengthy discussions with the family, the patient was placed on comfort care, and he died on the poststroke day 6. Patient consent for publication as a single case report was waived by the institutional review board.

- Postprocedure day 1 computed tomography of the head demonstrating a left middle cerebral artery territory infarct
DISCUSSION
Recently, a new technique for the treatment of thromboemboli within the supraclinoid segment of the ICA was proposed in the literature.[5] The authors detailed three cases of successful recanalization for thromboemboli within this location using remote aspiration through a balloon guide catheter inflated within the cervical segment of the ICA. In addition to being technically successful, this novel strategy appeared to be safe with no procedure-related complications.[5] The authors proposed that this technique may afford a cheaper, technically easier, and safer method of mechanical thrombectomy when compared with direct aspiration or stent retriever plus direct aspiration. Another potential benefit appears to be significantly reduced times to reperfusion. The average time to reperfusion in two cases in the study was 10.5 min. The last case in their series was prolonged by the need for balloon angioplasty of a carotid stenosis before the navigation of catheters into the ICA.[5]
In the case presented here, the balloon guide catheter was easily navigated into the cervical segment, and complete wall apposition of the balloon was achieved during inflation. We also were able to achieve significant flow reversal with the manual aspiration through the 60 mL syringe. Despite these successes, minimal recanalization of the ICA clot was achieved.
In addition, the technique resulted in an iatrogenic arterial dissection within the distal cervical segment that was not related to the previous catheter or wire manipulation. Although the exact cause for this dissection is unclear, we propose that it may have been the result of undue stress on the artery from forceful aspiration resulting in either arterial wall collapse or potentially kinking at the transition point of the artery from an extracalvarial to an intracalvarial location. This undue stress was likely the result of the failure of thrombus extraction with the force of aspiration applied to the vessel walls, rather than the thrombus. Although we agree with the authors of the previous study that this technique has the potential to be a safer method of performing mechanical thrombectomy by reducing the potential for complications associated with intracranial catheter and wire manipulation, it must be recognized, as with all new techniques, that there is the potential for its own set of complications.[56]
Remote aspiration of carotid terminus thromboemboli has the potential for many benefits including technical ease, decreasing cost, reducing time to reperfusion, and reducing complications associated with the intracranial catheter and wire manipulation. Although this novel strategy may be a potentially useful tool in the neurointerventionalists’ armamentarium, this technique may possess its own set of complications.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors would like to thank Kristin Kraus, M. Sc., for her invaluable assistance with the preparation of this paper.
REFERENCES
- Endovascular thrombectomy after large-vessel ischaemic stroke: A meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387:1723-31.
- [Google Scholar]
- Influence of device choice on the effect of intra-arterial treatment for acute ischemic stroke in MR CLEAN (Multicenter Randomized Clinical Trial of Endovascular Treatment for Acute Ischemic Stroke in the Netherlands) Stroke. 2016;47:2574-81.
- [Google Scholar]
- Initial clinical experience with the ADAPT technique: A direct aspiration first pass technique for stroke thrombectomy. J Neurointerv Surg. 2014;6:231-7.
- [Google Scholar]
- Comparison of clinical outcomes in patients with acute ischemic strokes treated with mechanical thrombectomy using either solumbra or ADAPT techniques. J Neurointerv Surg. 2016;8:1123-8.
- [Google Scholar]
- Remote aspiration thrombectomy in large vessel acute ischemic stroke. J Neurointerv Surg. 2017;9:250-2.
- [Google Scholar]
- Stent retrievers in acute ischemic stroke: Complications and failures during the perioperative period. AJNR Am J Neuroradiol. 2014;35:734-40.
- [Google Scholar]






