Translate this page into:
Anesthetic and surgical predictors of treatment outcome in re-do craniotomy
Address for correspondence: Dr. Adigun T.A., Department Of Anaesthesia, University College Hospital, Ibadan, Nigeria
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Craniotomy is a neurosurgical operation done to remove brain tumor, repair vascular lesion, and relieve intracranial pressure. Complications can arise which may necessitate re-do craniotomy. The study is planned to find out the relationship between variables such as age, American Society of Anaesthesiologist (ASA), Glasgow coma score (GCS), frequency of re-do craniotomy, and surgical outcome of re-do craniotomy.
Materials and Methods:
This is a retrospective study of all the patients who had re-do craniotomy over a 4-year period. The data that were collected included age, sex, ASA classification, indication for re-do craniotomy, GCS, frequency of re-do craniotomy, postoperative complications, and outcome.
Results:
Twenty-five patients had indication for re-do craniotomy within the study period. Forty percent were male and 60% were female, and their mean age was 38.56 ± 17.38 years. The indications for re-do craniotomy were removal of residual tumor, evacuation of clot, and cerebrospinal fluid leakage. Seventy-six percent had good outcome, while 24% had poor outcome. Outcome was good for patients who had re-do craniotomy done once, while poor outcome was for patients with second and third craniotomies. Ninety percent of patients with ASA 2 had good outcome, while 9.1% had poor outcome; but 64.3% had good outcome with ASA 3, while 37.7% had poor outcome with a P-value of 0.18. Seventy-five percent had poor outcome in patients with GCS of less than 9, while 25% had good outcome; but 14.3% had poor outcome in patients with GCS above 9, while 85.7% had good outcome with a P-value of 0.031.
Conclusions:
Increasing frequency of re-do craniotomy and lower GCS were major factors affecting outcome in re-do craniotomy in our center. The outcome of these patients is valuable in the management of other patients with re-do craniotomy in future.
Keywords
Outcome
predictors
re-do craniotomy
Introduction
Craniotomy is a commonly performed neurological operation. It is often performed to remove brain tumors, repair vascular lesion, and to relieve intracranial pressure. Complications that can occur include bleeding which may vary from intracerebral, intraventricular, subarachinoid haemorrhage and tumor bed hematoma, infection, stroke, and brain swelling, all of which may be an indication for a re-do craniotomy. Re-do craniotomy may be necessary to improve the clinical condition of the patients concerned. Our study was therefore planned to find the relationship between variables such as age, American society of Anaesthesiologist (ASA) classification, Glasgow coma scale (GCS), intraoperative hypotension, frequency of re-do craniotomy, and surgical outcome of re-do craniotomy in our patients.
Materials and Methods
Patients who had re-do craniotomy in our center between January 2005 and December 2008 were included in the study. Data were collected from neurosurgical and anesthesia operative records. Data that were collected included age, sex, the ASA classification, primary diagnosis, indication for re-do craniotomy, frequency of re-do craniotomy, GCS, intraoperative hypotension, postoperative complications, and outcome. Good outcome was defined as those who were discharged from the intensive care unit in good clinical condition, while poor outcome are those that died in the intensive care unit. Probable risk factors that could affect the outcome of management were explored using the Fisher's exact test. The level of significance was set at a P-value of ≤0.05. Multiple logistic regression was also applied to establish a relationship between the various risk factors and outcome. The odds ratio and 95% confidence interval were also calculated for the risk factors.
Results
One hundred and ninety craniotomies were performed during the study period, out of which 25 patients had an indication to undergo re-do craniotomy. Ten patients (40%) were male, while 15 patients (60%) were females. Fourteen patients were less than 40 years, while 11 patients were above 40 years with a mean age of 38.56 ± 17.38 years. Seventy percent of patients less than 40 years had good outcome, while 87.5% of the patients above 40 years had good outcome with a P-value of 0.624. Patients with less than 40 years of age had odds ratio of 5.56, while those above 40 years had odds ratio of 1.8 with confidence interval of 0.54. Six patients (24%) had poor outcome (died), while 19 (76%) had good outcome.
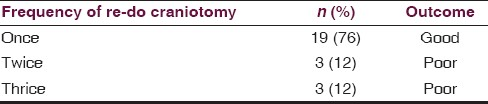
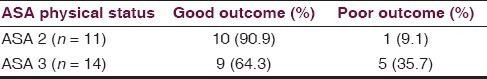
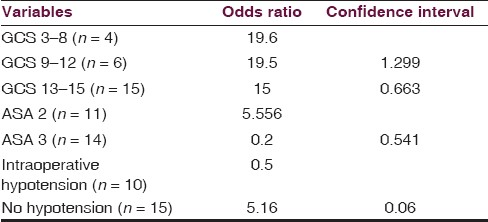
Ninety six percent of the patients had craniotomy for tumor excision, while 4% was for arteriovenous malformation. Table 1 shows indications for re-do craniotomy, which included removal of residual tumor (72%), evacuation of clot (16%), and cerebrospinal fluid (CSL) leakage (12%). Eighty percent of the patients had re-do craniotomy once, 12% had it twice, while 8% had it three times. Outcome was good for patients who had re-do craniotomy done once, while poor outcome was for patients with second and third craniotomies [Table 2]. Eleven patients had ASA's classification physical status of 2, while 14 patients had ASA of 3 preoperatively, and 90.9% of patients in ASA 2 had good outcome, while 9.1% had poor outcome; but 64.3% had good outcome in ASA 3, while 37.7% had poor outcome with a P-value of 0.18. The odds ratio was 5.6 for ASA 2, while it was 0.2 for ASA 3.The 95% confidence interval was 0.641 [Table 3].

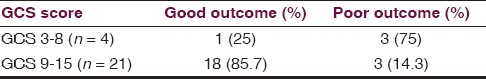
Four patients had a GCS of less than 9, while 21 patients had GCS between 9 and 15 before their re-do craniotomies, and 75% had poor outcome in patients with GCS of less than 9, while 25% had good outcome; but 14.3% had poor outcome in patients with GCS above 9, while 85.7% had good outcome with a P-value of 0.031. Patients with severe GCS had odds ratio of 19.6, and those with mild GCS had odds ratio of 19.5, while those with moderate GCS was 15 [Table 4].
The incidence of intraoperative hypotension (systolic blood pressure less than 100 mmHg) in this study was 40%; 12% of patients had poor outcome, while 27% of patient had good outcome with a P-value of 0.653. The odd ratio for those with intraoperative hypotension was 0.5, while for those without hypotension was 5.16 with 95% confidence interval of 0.06 [Table 5].
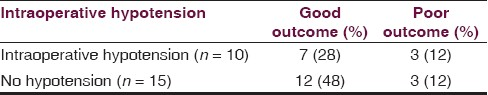
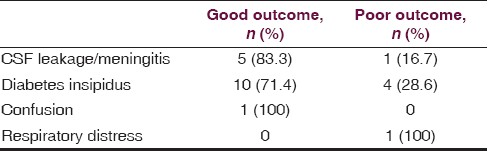
Table 6 illustrates the postoperative complications in the patients, and variables with odds ratio and confidence interval are shown in Table 7.
Discussion
The indications for re-do craniotomy in this study were removal of residual tumor, removal of tumor bed hematoma, and CSF leakage. In our center, evidence of residual tumor, tumor bed hematoma as seen on postoperative cranial computed tomography, and deteriorating GCS were used to determine the urgency of the re-do craniotomy.
In a study by Chang et al.,[1] looking into perioperative complications of neurological outcome of first and second craniotomies for glioma, they found 408 patients underwent first craniotomy and 91 patients for second craniotomy and found that papilloedema and altered level of consciousness were common indications for second craniotomy, and occasionally, the brain tumor may be too extensive to be removed at first surgery and hence a second or a third craniotomy may be needed or hemodynamics instability may cause the surgery to be rescheduled.
Age is a frequently studied variable. This study showed that more patients with age above 40 years had good outcome compared with those below 40 years after a re-do craniotomy, but this was not statistically significant. Using the patient's age alone as a score to determine whether or not they will survive has been shown to be invalid. There is a large amount of evidence that older patients do worse after emergency surgery with mortality rate in over 75 year olds double that of 65–75 years old in a United Kingdom study,[2] and they attributed this to more comorbidities in the elderly than younger patients. Age on its own has been shown to be a poor predictor of mortality, morbidity, and length of stay in hospital.
The ASA is a classification that grades the patients according to their general health and fitness for anesthesia and surgery.[3] ASA is easily available from the anesthetic record of the patient. Because ASA represents a global measure of the patient's pathophysiological response to disease burden or alternatively the lack of reserve to a stress because of disease burden, it follows that poor physical status will be associated with poor outcome.
To categorize these patients into different groups, the ASA classification is used. It was first devised by the ASA. They devised a system for collection and tabulation of statistical data in anesthesia for operative risk,[4] and six categories of operative risk were produced. Dripps et al.[4] modified it to five categories. Scores range from 1 (representing a healthy person) to 5 (representing a patient not expected to survive longer than 24 h). Several studies have shown correlation of ASA with surgical mortality.[5–7] From this study, 90.9% of patients in ASA 2 had good outcome, while 9.1% had poor outcome; but 64.3% had good outcome in ASA 3, while 37.7% had poor outcome but was not statistically significant. From this study also patients with ASA 2 are 5.6 times more likely to survive compared with ASA 3 after a re-do craniotomy, and ASA 3 patients are 0.2 times less likely to survive.
GCS is a neurological scale that aims to give a reliable, objective way of recording the conscious state of a person for initial and subsequent assessment.[8] A patient is assessed against the criteria of the scale, and the resulting points give a patient score between 3 (indicating deep unconsciousness) and either 14 (original scale) or 15 (the more widely used modified or revised scale). It was invented in 1974 by Graham Teasdale and Bryan J Jennet, professors of neurosurgery at the University of Glasgow.[8] From this study, 75% of patients with GCS of less than 9 had poor outcome, while 25% had good outcome; but the outcome was poor in 14.3% patients with GCS between 9 and 15, while 85.7% had good outcome and this was statistically significant. It shows that patients with GCS less than 8 are 19.6 times less likely to survive.
Intraoperative parameters measured by blood pressure and heart rate are frequently measured variables during anesthesia, and intraoperative hypotension is a common intraoperative side effect and has been reported to be associated with adverse perioperative outcome.[9] The incidence of intraoperative hypotension of systolic of less than 100 mmHg in this study was 40%, and 12% of patients had poor outcome, while 27% of patient had good outcome but was not significant. Patients without hypotension are 5.16 times more likely to survive than those with hypotension. In the current era, the risk of intraoperative hypotension in the immediate perioperative period appears to be quite small, but a prospective, longitudinal study[9] of 1-year postoperative mortality after non-cardiac surgery confirms that comorbidity is the primary predictor and that intraoperative hypotension and prolonged cumulative deep hypnotic time are also significant risk factors predicting mortality after non-cardiac surgery. Better intraoperative anesthetic management may have a greater effect on long-term outcomes than previously appreciated.
Outcome of surgery is related to the frequency of the re-do craniotomy in this study, and outcome is good after the first re-do craniotomy, while outcome is poor following second and third re-do craniotomies. This may be due to the fact that patients who had two or more re-do craniotomy had lower GCS and also increasing number of postoperative complications.
The most common complications in our patients were CSL leakage/meningitis, and diabetes insipidus. Table 5 shows that most of the patients with these complications were successfully treated. However, poor outcome was noted in patients who had multiple complications.
In conclusion, it can be clearly seen that patients can undergo re-do craniotomy up to three times as long as there is an indication for it; however, our study shows that second and third re-do craniotomies were associated with poor outcome. This is a challenge for us as effort must be put in place to improve the outcome of such surgeries. Increasing frequency of re-do craniotomy and lower GCS scores are major factors leading to poor outcome in our patients. Better intraoperative care, improved operative skill, surgical equipment, and better intensive care support will most likely improve outcome in our patients in future.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Perioperative complications and neurological outcomes of first and second craniotomies among patients enrolled in the glioma outcome project. J Neurosurg. 2003;98:1175-81.
- [Google Scholar]
- The effect of pulse oximetry, age and ASA physical status on the frequency of patients admitted unexpectedly to a post operative intensive care unit and the severity of their anesthesia related complications. Anesth Analg. 1992;74:181-8.
- [Google Scholar]
- ASA physical Status and age predict morbidity after three surgical procedures. Ann Surg. 1994;220:3-9.
- [Google Scholar]
- Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2:81-4.
- [Google Scholar]
- Anaesthetic management and one year mortality after non cardiac surgery. Anesth Analg. 2005;100:4-10.
- [Google Scholar]






