Translate this page into:
Advanced Age and Higher National Institutes of Health Stroke Scale Score as Predictors of Poor Outcome in Ischemic Stroke Patients Treated with Alteplase: A Study from a Tertiary Care Centre in Rural North-west India
Address for correspondence: Dr. Sunil Kumar Raina, Department of Community Medicine, Dr. RPGMC, Tanda, Kangra, Himachal Pradesh, India. E-mail: ojasrainasunil@yahoo.co.in
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Thrombolytic therapy in acute ischemic stroke has been approved for treatment of acute stroke for past two decades. However, identification of predictors of poor outcome after the intravenous (IV) alteplase therapy in acute stroke patients is a matter of research. The present study was conducted with the aim of identifying poor prognostic factors in patients of acute ischemic stroke patients.
Methods:
The data of 31 acute stroke patients treated with alteplase were gathered to identify the factors that were independent predictors of the poor outcome. Outcome was dichotomized using modified Rankin scale (mRS) score and National Institutes of Health Stroke Scale (NIHSS) score at 3 months after treatment into good outcome mRS – 0–2 and poor outcome mRS – 3–6. Predictors of poor outcome were analyzed.
Results:
Good outcome (mRS – score 0–2) was seen in 15 (48.4%) patients with median age of (60) and poor outcome (mRS – score 3–6) was seen in 16 (51.6%) patients median age of 75 years, which was statistically significant with the P = 0.002. The presence of risk factors such as hypertension, diabetes, dyslipidemia, smoking, alcohol intake, history of stroke, coronary artery disease, and rheumatic heart disease among the two groups did not seem influence outcome. The severity of stroke as assessed by NIHSS score at the time of presentation was significantly higher among the patients with poor outcome, with P = 0.01.
Conclusion:
Advance age and higher NIHSS score at the time of onset of stroke and are the independent predictors of the poor outcome after thrombolysis with IV alteplase treatment in acute ischemic stroke patients.
Keywords
Alteplase
ischemic stroke
National Institutes of Health Stroke Scale Score
poor outcome
predictors
INTRODUCTION
Stroke is the leading cause of serious long-term disability worldwide.[1] A review of the literature on stroke reveals that ischemic stroke may account for about 85% of all strokes.[2] Current strategies of acute ischemic stroke management include intravenous tissue plasminogen activator (IV-tPA) and endovascular intervention.[3] The thrombolytic therapy in acute ischemic stroke has to be administered within 4.5 h after symptom onset.[4] Time from onset of stroke symptoms to treatment with thrombolysis is crucial for outcome after ischemic stroke.[5] There are various factors which predict the outcome in acute stroke patients treated with IV alteplase therapy. The clinical characteristics of the patient, such as age, gender, severity of stroke, diabetes, hypertension, and cardiovascular comorbidities, are the known risk factors of stroke and predictors of poor outcome in untreated patients.[6]
The outcome is also determined by factors such as age, gender, stroke severity at the time of presentation as assessed by National Institutes of Health Stroke Scale (NIHSS) score.[678]
Alteplase has been approved for treatment of acute stroke for the past two decades and has shown favorable outcome in stroke patient.[910] However, this treatment modality has been introduced in our rural medical college only in the last year. There were studies which have shown higher in-hospital mortality in acute stroke patient receiving alteplase therapy[11] and various independent predictors of the good outcome after the IV alteplase therapy in acute stroke patients has also been characterized.[1213]
An extensive review of literature reveals paucity of data on studies predicting poor outcome after the IV alteplase therapy in acute stroke patients. Therefore, the objective of the current analyses was to determine poor prognostic factors after IV alteplase for acute ischemic stroke patients.
METHODS
Study design and participants
This prospective study was carried out among 31 stroke patients undergoing thrombolysis at a tertiary care center in a rural area of North-west India. For establishing inclusion in the study, all patients identified as presenting to or referred to emergency department with a suspected stroke underwent a computed tomography (CT) scan. Out of these patients, those who had presented within the window period of 4.5 h and with no intracranial bleed were included in this study.
The study participants were shifted to the Intensive Care Unit of hospital and a protocol for thrombolysis was followed. A follow-up for these patients was established (as detailed below) for evaluation of poor outcome using NIHSS scoring.
Details of the procedure
The study participants were thrombolysed with IV-tPA alteplase, provided free of cost to the patient by the State Government. Thrombolysis was done with IV-tPA alteplase after reconstitution as per the manufactures guideline at a dose of 0.9 mg/kg. Ten percent of total dose was given intravenously as bolus over 1 min and the rest 90% was given as infusion with electronic injection perfuser over 1 h. The patient was monitored during the procedure for any adverse reaction and complication. Vitals were monitored every 15 min during the procedure followed by every hour for 2 h and every two hourly for next 24 h.
The data of these patients were entered in a Pro forma for the purpose of evaluation. The presence of risk factors and comorbidities were determined for each patient from the data obtained.
The various risk factors determined were age, gender, hypertension, diabetes, dyslipidemia, smoking, alcohol, history of stroke, coronary artery disease (CAD), and history of rheumatic heart disease (RHD). In addition to details on risk factors, details regarding the knowledge about stroke, mean of transportation, treatment patient taking, time of onset, interventions, etc., were also recorded in the Pro forma. Prehospital and in-hospital time delay in management of stroke patients was calculated for each patient.
Blood pressure, pulse rate, and its character, especially irregularity of pulse, and blood sugar at the time of presentation was determined. Mean of transport from the site of the event to the hospital was determined for each patient. The time elapsed between deficits to hospital admission, between hospital admission and CT head, between hospital admission and thrombolysis, between deficit and start of thrombolysis, and between hospital admission and start of thrombolysis were determined for each patient.
Outcome
Outcome was determined using modified Rankin scale (mRS) score and NIHSS score at 3 months after treatment. Good outcome was determined as mRS score 0–2 and poor outcome as mRS score 3–6.
Statistical analysis
The data summarized as proportions were compared using Chi-square test and those presented as means were compared using the unpaired Student's t-test. The level of significance was set at the level 5%.
RESULTS
The study cohort comprised 31 patients (21 males and 10 females). Table 1 compares the risk factors and clinical character associated with the good and poor outcome. Good outcome (mRS – score 0–2) was seen in 15 (48.4%) patients with median age of (60) and poor outcome (mRS – score 3–6) was seen in 16 (51.6%) patients median age of 75 years, which was statistically significant with the P = 0.002. There were 21 males, 11 (52.4%) had good outcome and 10 (47.1%) had poor outcome, and out of 10 females, 4 (40%) had poor outcome whereas 6 (60%) had good outcome. There was not much difference in the body mass index (BMI) among the two groups with median BMI of 21.01 in good outcome and 22.3 in poor outcome group. There was not much difference in the risk factors such as hypertension, diabetes, dyslipidemia, smoking, alcohol intake, history of stroke, CAD, and RHD among the two groups.

The severity of stroke as assessed by NIHSS score at the time of presentation was significantly higher among the patients with poor outcome, with P = 0.01.
The basic parameters such as education, awareness, means of transportation, and blood pressure at the time of presentation of the patient at hospital was not significantly different between poor outcome group and good outcome group.
The mean duration of deficit at the time of presentation to the hospital from the onset of deficit was 99 min in good outcome group and 87 min in poor outcome group [Table 2].
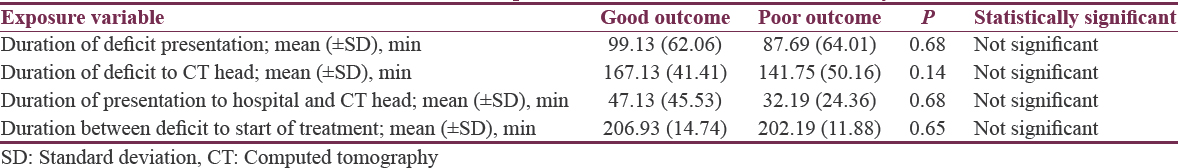
Moreover, mean duration of deficit at the time of start of treatment was 206 min and 202 min in good outcome group and poor outcome group.
DISCUSSION
There are various factors which predict the outcome in acute stroke patients treated with IV alteplase therapy. The clinical characteristics of patient, such as age, gender, severity of stroke, diabetes, hypertension, and cardiovascular comorbidities, are the known risk factors of stroke and predictors of poor outcome in untreated patients.[6] In the present study, we analyzed these risk factors and their relation with the outcome at 3 months after treatment, in patients with acute stroke treated with IV alteplase within 4.5 h of onset.
Studies have shown that every 10 years increase in age are associated with 3.6-fold decrease in the good outcome.[14] Our study also found that acute stroke patients with advanced age have poor outcome at 3 months after thrombolysis with alteplase. The findings are consistent with studies which showed that advanced age is an independent factor associated with the poor outcome.[14]
The time of treatment from the onset of deficit to start of treatment was inversely related to the outcome in an earlier study.[15] However, we did not find any difference between the good and poor outcome in our study with respect to start of treatment. This may be because majority of our patients were thrombolysed within 3–4 h of stroke onset in our study.
NIHSS score is a score of severity of the stroke. We have found that patients with higher NIHSS score at the time of treatment have poor outcome 3 months after treatment with IV alteplase therapy. The difference between the good and poor outcome was statistically significant. These findings again are consistent with studies that showed that higher NIHSS score at the time of presentation is associated with the poor outcome and NIHSS score >16 is associated with more probability of death or severe disability and score <6 has good prognosis.[6]
CONCLUSION
From this study, a higher NIHSS score at the time of onset of stroke and advance age in acute ischemic stroke patients are independent predictors of poor outcome after thrombolysis with IV alteplase. Patients with lower NIHSS score and of young were more likely to be benefited from therapy.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Oxidative stress and its role in the pathogenesis of ischaemic stroke. Int J Stroke. 2009;4:461-70.
- [Google Scholar]
- Modern medical management of acute ischemic stroke. Methodist Debakey Cardiovasc J. 2014;10:99-104.
- [Google Scholar]
- Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359:1317-29.
- [Google Scholar]
- Time to treatment with intravenous alteplase and outcome in stroke: An updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials. Lancet. 2010;375:1695-703.
- [Google Scholar]
- Poor outcome after first-ever stroke: Predictors for death, dependency, and recurrent stroke within the first year. Stroke. 2003;34:122-6.
- [Google Scholar]
- Sex differences in the clinical presentation, resource use, and 3-month outcome of acute stroke in Europe: Data from a multicenter multinational hospital-based registry. Stroke. 2003;34:1114-9.
- [Google Scholar]
- Community hospital-based stroke programs: North Carolina, Oregon, and New York. III. Factors influencing survival after stroke: Proportional hazards analysis of 4219 patients. Stroke. 1986;17:294-9.
- [Google Scholar]
- Intravenous tissue-type plasminogen activator for treatment of acute stroke: The standard treatment with alteplase to reverse stroke (STARS) study. JAMA. 2000;283:1145-50.
- [Google Scholar]
- Effectiveness of t-PA in acute ischemic stroke: Outcome relates to appropriateness. Neurology. 2000;54:679-84.
- [Google Scholar]
- Use of tissue-type plasminogen activator for acute ischemic stroke: The Cleveland area experience. JAMA. 2000;283:1151-8.
- [Google Scholar]
- Identifying patients at high risk for poor outcome after intra-arterial therapy for acute ischemic stroke. Stroke. 2009;40:1780-5.
- [Google Scholar]
- Predictors of a good outcome after endovascular stroke treatment with stent retrievers. ScientificWorldJournal. 2015;2015:403726.
- [Google Scholar]
- Early stroke treatment associated with better outcome: The NINDS rt-PA stroke study. Neurology. 2000;55:1649-55.
- [Google Scholar]
- Baseline NIH stroke scale score strongly predicts outcome after stroke: A report of the trial of Org 10172 in acute stroke treatment (TOAST) Neurology. 1999;53:126-31.
- [Google Scholar]






