Translate this page into:
Adherence to Antiepileptic Therapy in Adults
Address for correspondence: Dr. Sarala Narayana, Department of Pharmacology, Sri Devaraj Urs Medical College, Sri Devaraj Urs Academy of Higher Education and Research, Tamaka, Kolar - 563 101, Karnataka, India. E-mail: n_sarala@rediffmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Context:
Epilepsy is a neurological disorder affecting 70 million worldwide. The high incidence of relapse can be attributed to nonadherence, thus increasing the incidence of refractory epilepsy to 10%–20%.
Aims:
This study was planned to determine rate of adherence and factors affecting adherence using Antiepileptic Adherence Questionnaire and Baseline Adherence Questionnaire.
Materials and Methods:
A cross-sectional, questionnaire-based study was carried out at a rural hospital from May to September 2015. Patients of either gender aged 18–60 years, diagnosed with epilepsy were interviewed after they consented. Patient details, responses to questionnaires were collected and analyzed using descriptive statistics.
Results:
Among the participants, 67.8% were males and 32.2% were females with the mean age of 38.3 ± 13.9 years. The response rate was 75% (90/120). The majority were literate (64.4%) and employed (58.9%). The duration of disease was <5 years in most individuals; 50% were highly, 21.1% moderately, and 28.9% nonadherent to treatment. Among the highly adherent, 66.7% never skipped medications because they had knowledge of the disease and treatment. More than 97% were satisfied with the social support, and 89% expressed that their family and friends reminded them to take medications. Patients who were nonadherent to treatment attributed it to the lack of knowledge of the disease (57%) and treatment (96%). Reasons for nonadherence were patients assumed drug was harmful, felt cured of the disease, and wanted to avoid side effects.
Conclusion:
Nearly, 70% expressed the lack of satisfactory support from the social circle. We observed that nearly seventy percent epileptic patients were moderate-highly adherent. Nonadherence was attributed to patient feeling cured of disease and assuming medications to be harmful. Counseling of patients will help in adherence to treatment.
Keywords
Adherence
antiepileptics
questionnaire
INTRODUCTION
Epilepsy is the second most common neurological disorder affecting 70 million individuals worldwide,[1] with an annual incidence of approximately 0.2–0.6/1000 population per year in India.[2] Therapy reduces the frequency of seizures which offers a better quality of life. There still exists a high incidence of refractory epilepsy (10%–20%)[3] and nonadherence maybe one of the common factors.
Adherence is the primary determinant of the effectiveness and defined as “the extent to which an individual's behavior regarding taking medications, following a diet, and performing lifestyle changes follows agreed recommendations from a health-care provider.”[4] The current rate, especially for chronic illnesses with long-term therapy in developing countries is <50%, epilepsy is one of them.[45] Nonadherence which can be described as either incorrect dosage, forgetfulness, or discontinued medication can interfere with disease progression and treatment and thus alter the improvement in patient's health. It can lead to increased medical resource utilization and health-care costs along with increased the risk of death.[6]
Although there exists no gold standard for measuring adherence,[4] evaluations can be performed through self-report, pill counts, prescription refill rates, use of adherence scales, questionnaires or biological markers, including serum, urine, and saliva to quantify medications or their metabolites. The ability of patients to follow optimal treatment is compromised by more than one barrier; hence, this study was planned to determine rate of adherence and identify the factors affecting adherence to antiepileptic drug treatment using questionnaire which includes patient-related, therapy-related, condition-related, socioeconomic, and health-care determinants.
MATERIALS AND METHODS
A cross-sectional study was conducted among the rural population of Kolar, by the Departments of Pharmacology and Medicine. The protocol was approved by the Institutional Ethics Committee. All patients of either gender aged between 18 and 60 years, diagnosed with epilepsy and with no change in antiepileptic drug therapy in the last 3 months, attending the outpatient Departments of Medicine, Neurology, inpatients of medical wards or those presenting to the emergency room of a tertiary care hospital were recruited after obtaining informed consent. The data were collected between May and September 2015.
The patients were interviewed by the investigator and details collected as per the proforma which included educational status, socioeconomic status, duration of illness and treatment, medication details, and comorbid conditions if any. Following this, they were also interviewed for two structured questionnaire tools namely, Antiepileptic Adherence Questionnaire (AAQ) and Baseline Adherence Questionnaire (BAQ) in English which included eight and thirty questions, respectively. These questionnaires were self-designed after reviewing existing literature, validated by postgraduates, faculty, and peers; the suggested modifications were incorporated. They comprised questions to obtain information regarding adherence rate, reasons for missed medication, patient knowledge and habits, psychometric analysis, and social support. The responses for the questionnaire were obtained orally from the illiterates and written from the rest of the patients.
The questionnaire tools were devised to obtain data regarding patient's adherence, subjective health status, medication-related variables, perceived barriers, knowledge and beliefs of the patient and family regarding the disease and treatment, adverse effects of the drugs if any experienced and psychological status due to the chronic illness or long-term therapy. The data obtained were analyzed using descriptive statistics. Multiple stepwise logistic regression analysis was used to identify the factors influencing adherence. Statistical Package for Social Sciences Version 22.0, manufactured by International Business Management Corporation was used for statistical analysis. P < 0.05 was considered statistically significant.
RESULTS
A total of 120 patients who complied with the inclusion criteria were approached to be a part of the study, of which only ninety consented to participate, and most of them were males and belonged to the age group of 30–49 years [Table 1]. The majority were literate (64.4%) and employed (58.9%). More than 65% of patients were on phenytoin [Table 2], and 47.8% consumed two tablets per day. Eleven and ten percent of patients had a history of smoking and alcohol consumption.


As per the AAQ, 50% were highly adherent, 21.1% moderately, and 28.9% nonadherent to treatment. The rate of adherence was the highest among male patients, those in the age group of 18–29 years and in patients consuming one tablet per day. Illiterates, unemployed individuals or those employed with craft and related trade work, elementary occupations revealed nonadherence [Table 3]. Duration of illness was <5 years in the majority of patients (48/90) and adherence was least in them as compared to patients with prolonged illness [Figure 1].

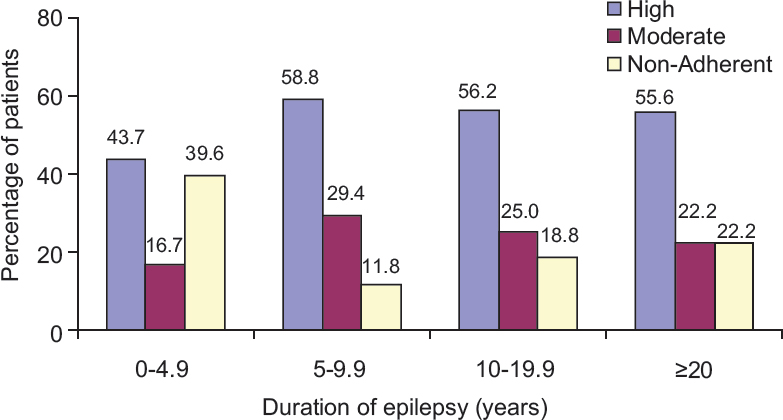
- Comparison of duration of illness with level of adherence
Among the highly adherent patients as per BAQ, more than 90% had knowledge about the disease and treatment. Nearly, 66.7% of patients had never skipped medications. More than 97% were satisfied with the social support, and 89% expressed that their family and friends reminded them to take medications. Patients who were moderately adherent had more knowledge about the treatment (89.5%) as compared to the disease (68.4%). In more than 50% of these patients, the reasons for missing medications were to avoid side effects, ran out of medications or they felt cured of the disease [Figure 2]. Although 94% admitted that they were somewhat satisfied with support from their family and friends, only 74% received their help in taking medications and thus improving adherence. Nonadherent patients had some knowledge of the disease (42.3%) and were ignorant about the treatment (3.8%). Nearly, 85% had missed medications in the recent past. Reasons for nonadherence were patients assumed drug was harmful (n = 32, 35.5%), felt cured of the disease and wanted to avoid side effects. They expressed a lack of satisfactory support from the social circle (69%), and more than 70% experienced that relatives and friends avoided them. Among these nonadherent patients, 27% and 23% were depressed and had difficulty in concentrating, respectively, and more than 50% experienced disturbed sleep. Multiple stepwise logistic regression analysis revealed that the factors such as time since last missed medication (P = 0.0001), beliefs of the patient about the toxicity of the drug (P = 0.0001), family and social support (P = 0.004), gender (P = 0.016), educational status (P = 0.022), occupation of the patient (P = 0.006), forgetfulness (P = 0.0001), and knowledge about the disease (P = 0.031) were the factors that predicted 83.4% variance in the adherence rate (R2 = 0.834, P = 0.0001).
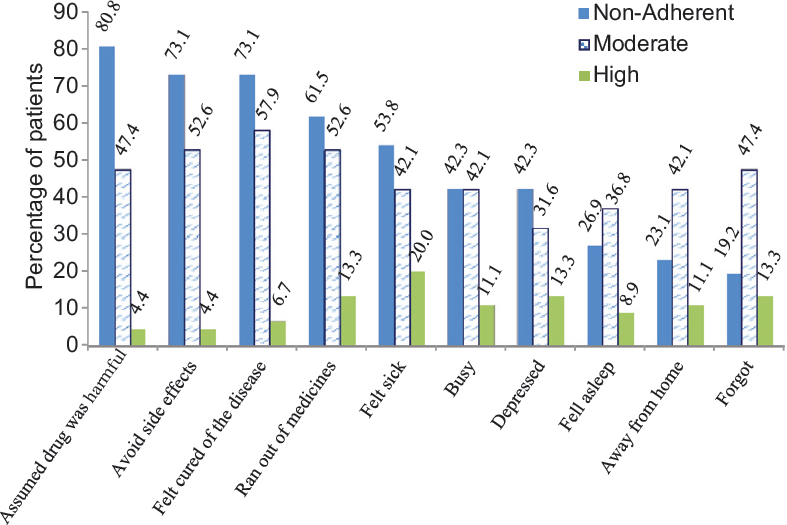
- Reasons for missed medication in epileptic patients
DISCUSSION
Treatment of epilepsy is necessary to alleviate the global burden of such chronic illness. This study highlights pertinent factors affecting adherence to treatment in patients living with epilepsy in a rural background in India. About seventy percent of patients showed moderate-high adherence to therapy which was similar to other studies conducted in Asia[78] but comparatively higher than those conducted in other continents, where moderate to low adherence was predominant.[910] Males, literates, and employed patients were found to be highly adherent as compared to their other counterparts, signifying that these sociodemographic parameters allowed them to gain better access to treatment and provided greater motivation to continue therapy. Patients with relative recent onset epilepsy exhibited lower adherence as they did not fear the occurrence of recurrent seizures, which usually occurs in noncompliance to treatment. As the number of patients who admitted to social habits such as smoking and alcohol consumption were meager, their association has not been studied. Knowledge about the disease and treatment has shown to have a strong association with the rate of adherence. Social support received by patients has been consistently reported as an important factor affecting health outcomes and behaviors,[6] and the same is observed in our study. A study showed that an in-depth understanding of the social and cultural dimensions would prove to break barriers in treatment, to make them effective and sustainable.[11]
Nonadherent patients were significantly more likely to have negative perceptions about the treatment and expressed stronger concerns about potential harm due to drug. Most often a seizure-free period, lack of accessibility to medicines, side effects of the drug, and forgetfulness refrained them from continuing therapy. Chapman et al. also reported nonadherence was related to similar beliefs of the patient, perceptions of medications, and proposed patient-centered interventions to improve the same.[12] Depression and difficulty in concentration although seen in <15% of the total study population, could not be acclaimed as either a cause or effect of adherence.
Our findings indicate that there are several factors which attribute to patient's treatment compliance such as prevailing beliefs, lack of knowledge and motivation from social groups. These factors may result in poor health status in epileptic patients, despite advanced treatment options.
CONCLUSION
In the current study nearly 70% epileptic patients were moderate-highly adherent to treatment. Nonadherence was attributed to patient feeling cured of disease and assuming the medications to be harmful. Health-care providers play an important role in optimizing adherence by counseling the patients and caretakers.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Estimation of the burden of active and life-time epilepsy: A meta-analytic approach. Epilepsia. 2010;51:883-90.
- [Google Scholar]
- Epilepsy in India I: Epidemiology and public health. Ann Indian Acad Neurol. 2015;18:263-77.
- [Google Scholar]
- WHO, Adherence to Long-Term Therapies: Evidence for Action. Available from: http://www.who.int/chp/knowledge/publications/adherence_full_report.pdf
- E-Health Interventions and Improvement in Treatment Adherence. Available from: http://www.ntvg.nl/artikelen/e-healthinterventies-en-verbetering-van-therapietrouw
- Assessing adherence-based quality measures in epilepsy. Int J Qual Health Care. 2012;24:293-300.
- [Google Scholar]
- Depression and anxiety are associated with reduced antiepileptic drug adherence in Chinese patients. Epilepsy Behav. 2015;50:91-5.
- [Google Scholar]
- An evaluation of factors affecting adherence to antiepileptic drugs in patients with epilepsy: A cross-sectional study. Singapore Med J. 2017;58:98-102.
- [Google Scholar]
- Factors associated with treatment non-adherence in patients with epilepsy in Brazil. Seizure. 2013;22:384-9.
- [Google Scholar]
- Psychosocial factors associated with medication adherence in ethnically and socioeconomically diverse patients with epilepsy. Epilepsy Behav. 2015;46:242-5.
- [Google Scholar]
- The reasons for the epilepsy treatment gap in Kilifi, Kenya: Using formative research to identify interventions to improve adherence to antiepileptic drugs. Epilepsy Behav. 2012;25:614-21.
- [Google Scholar]
- Patients’ perspectives on antiepileptic medication: Relationships between beliefs about medicines and adherence among patients with epilepsy in UK primary care. Epilepsy Behav. 2014;31:312-20.
- [Google Scholar]






