Translate this page into:
Acute Disseminated Encephalomyelitis Presenting as an Isolated Mesodiencephalic Junction Lesion
Address for correspondence: Dr. Kondanath Saifudheen, Department of Neurology, Malabar Institute of Medical Sciences, Govindapuram, Kozhikode - 673 016, Kerala, India. E-mail: drsaifu@yahoo.co.in
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
A 32-year-old woman presented with 4-week history of diplopia and forgetfulness and unsteadiness on walking. Two weeks previously she had had upper respiratory tract infection. There were no other systemic manifestations. Clinical examination showed impaired episodic memory, vertical gaze palsy in both up and down gaze, right eye abduction deficits (likely pseudoabducens palsy), and normal pupil reaction. She had impaired tandem walking, normal power, and deep tendon reflexes. Her fundus examination was normal, and meningeal signs were absent.
Magnetic resonance imaging (MRI) of the brain showed symmetric hyperintensities in fluid-attenuated inversion recovery sequences, involving thalami and midbrain [Figure 1]. These lesions were hypointense on T1-weighted and did not show any diffusion restriction. Enhancing foci noted in thalami, periventricular region of the third ventricle, and periaqueductal region [Figure 2]. MR angiography, venography, and MRI of the spine were normal. Visual evoked potentials were normal.
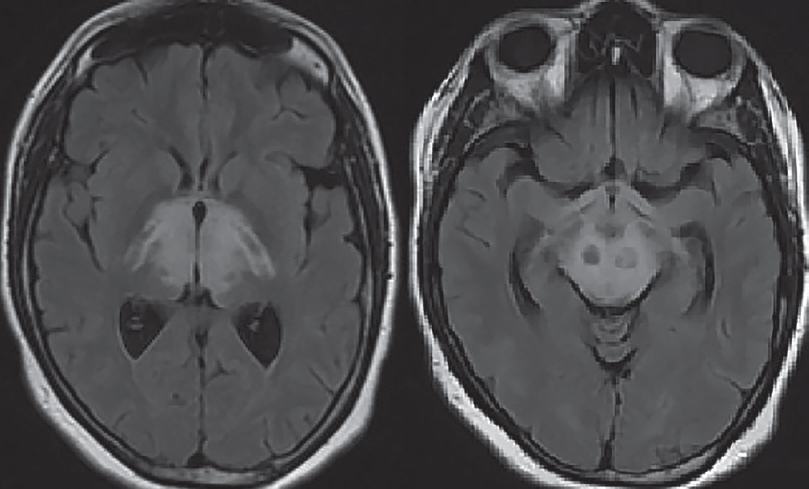
- Axial fluid-attenuated inversion recovery image showing symmetric hyperintensities involving thalami and midbrain
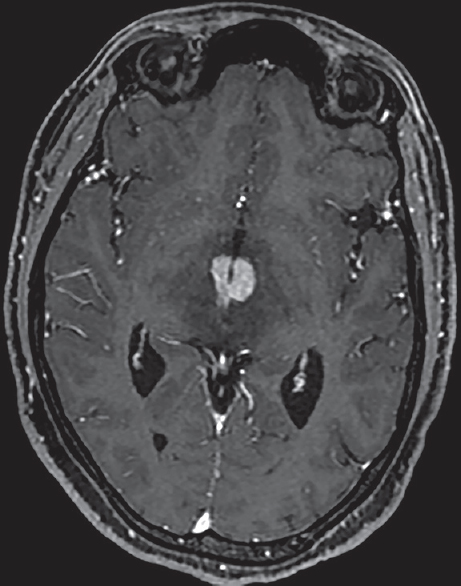
- Axial T1-weighted contrast image showing enhancing foci in thalami, periventricular region of the third ventricle, and periaqueductal region
Cerebrospinal fluid (CSF) study showed elevated protein (60 mg/dl), normal sugar, and 5 lymphocytes/mm3. Gram's stain did not yield any organism. Vasculitic workup, serological testing for human immunodeficiency virus, hepatitis B surface antigen, and aquaporin-4 (anti-neuromyelitis optica) antibody were negative, and serum and CSF venereal disease research laboratory test were negative. Cytological analysis of the CSF yielded no malignant cells. Other parameters of blood counts and urine examination were within normal limits. Pathergy test was negative. The chest X-ray and ultrasonography of the abdomen and pelvis were normal. Based on the clinical picture, imaging findings, and after ruling out other possible etiologies, a final diagnosis of possible acute disseminated encephalomyelitis (ADEM) was made. The patient was treated with intravenous methylprednisolone 1 g once daily for 5 days. The neurological deficits resolved in 1 week. Repeat MRI done 3 months later showed complete resolution of the lesions [Figure 3]. Last clinical follow-up after 1 year showed no fresh neurological symptom and signs.
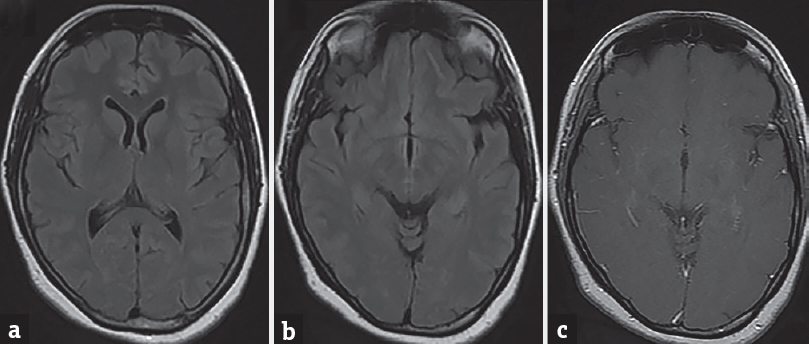
- Axial fluid-attenuated inversion recovery (a and b) and contrast (c) showing complete resolution of lesion
Isolated mesodiencephalic junction (MDJ) involvement is rare and atypical for ADEM diagnosis. ADEM is a monophasic inflammatory demyelinating disease of the central nervous system, characterized by scattered focal or multifocal (disseminated) inflammation of the brain and/or spinal cord. Although no specific MRI criteria have been identified for ADEM, certain patterns are generally recognized. Four patterns of cerebral involvement have been proposed to describe the MRI findings in ADEM: (1) ADEM with small lesions (5 mm); (2) ADEM with large, confluent, or tumefactive lesions, with frequent extensive perilesional edema and mass effect; (3) ADEM with additional symmetric bithalamic involvement; and (4) acute hemorrhagic encephalomyelitis, when some evidence of hemorrhage can be identified in the large demyelinating lesions.[1] However, less characteristic cases may cause a diagnostic dilemma and delay in treatment. Our case was peculiar in that demyelination was limited to MDJ. There is a broad spectrum of central nervous system disorders, with considerable overlap in presenting symptoms and imaging of MDJ, leading to diagnostic uncertainty. These disorders include Neuro-Behcets disease,[2] Anti-Ma2-positive paraneoplastic brainstem encephalitis,[3] Wernicke encephalopathy,[4] lymphoma,[5] neurosarcoidosis,[6] and infectious brain stem encephalitis and vasculitis.[1]
As the ADEM is a treatable disease, even the MRI is atypical, it is important to manage as early as possible because delay in treatment may cause complications such as axonal loss and further progression of disease, which can be catastrophic, especially the lesions involve crucial locations such as MDJ where biopsy is not always performed due to the poor accessibility of the lesion and morbidity associated with it. If one is in doubt, the diagnosis has to be made by exclusion of a number of likely differential diagnoses. Sequential MRI during the follow-up period plays an important role in establishing the diagnosis of ADEM.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Isolated brain stem lesion in children: Is it acute disseminated encephalomyelitis or not? AJNR Am J Neuroradiol. 2013;34:217-20.
- [Google Scholar]
- CNS involvement in neuro-behçet syndrome: An MR study. AJNR Am J Neuroradiol. 1999;20:1015-24.
- [Google Scholar]
- Wernicke encephalopathy: MR findings at clinical presentation in twenty-six alcoholic and nonalcoholic patients. AJNR Am J Neuroradiol. 2007;28:1328-31.
- [Google Scholar]
- B Cell lymphoma of the brain stem masquerading as myasthenia. J Neurol Neurosurg Psychiatry. 2002;72:271-3.
- [Google Scholar]
- Imaging of neurosarcoidosis: Common, uncommon, and rare. Clin Radiol. 2016;71:96-106.
- [Google Scholar]





