Translate this page into:
A randomized controlled trial of nurse-led Brief Focused Intervention for patients with alcohol use-related mild traumatic brain injury in the emergency and casualty services of a tertiary hospital
*Corresponding author: Prasanthi Nattala, Department of Nursing, National Institute of Mental Health and Neuro Sciences, Bengaluru, Karnataka, India. paidi89@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Pavalur R, Nattala P, Kandasamy A, Shukla DP. A randomized controlled trial of nurse-led Brief Focused Intervention for patients with alcohol use-related mild traumatic brain injury in the emergency and casualty services of a tertiary hospital. J Neurosci Rural Pract. 2024;15:103-10. doi: 10.25259/JNRP_381_2023
Abstract
Objectives:
Driving under the influence of alcohol is one of the leading causes of road traffic accidents in India. Individuals with acute injuries often present to emergency hospital services. Carrying out brief interventions in the emergency can prevent further injury and even progression to severe patterns of drinking. However, there are no known studies from India examining the effectiveness of such interventions in emergency settings. Against this background, the objective of this randomized controlled trial was to evaluate the effectiveness of a nurse-led Brief Focused Intervention (BFI) in comparison with the minimal intervention for patients with mild Traumatic Brain Injury (TBI) reporting to the emergency and casualty services of a tertiary hospital in Bengaluru, South India, who screened positive for alcohol use.
Materials and Methods:
The BFI comprised a video portraying the effects of alcohol on the brain and muscles and brief advice on how to reduce or avoid alcohol use. Subjects (N = 90) were randomly allocated to two groups: BFI (n = 45) or Minimal Intervention Group (MIG) (n = 45). Standardized tools were used to assess both groups on specific outcomes for up to six months following discharge from the emergency and casualty services. At the end of six months, complete data wasavailable for 73 patients.
Results:
Participants’ (N = 73) mean age was 35 years (standard deviation [SD]-11). Over the six-month follow-up, the BFI group reported significantly lesser quantity of alcohol consumption (Alcohol Use Disorder Identification Test [AUDIT] Score – 5.03, SD 4.09, 95% confidence interval [CI] = 3.70, 6.35) compared to MIG (AUDIT Score – 9.76, SD 2.96, 95% CI = 8.73, 10.80), and fewer alcohol use-related problems in BFI group (Mean – 4.18, SD 3.21, 95% CI = 3.14, 5.22) compared to MIG (Mean – 5.88, SD 2.59, 95% CI = 4.98, 6.79). Results of logistic regression showed that being in MIG as well as baseline hazardous use of alcohol were associated with unfavorable outcomes at the end of six months follow-up.
Conclusion:
Findings provide the first known evidence from India for the effectiveness of nurse-led BFI in the emergency and casualty services in improving post-discharge outcomes for patients with alcohol use-related mild TBI. While the findings of the study are statistically significant, these findings also have significant clinical relevance, as they have shown that the BFI improved clinical outcomes. Thus, brief interventions should be implemented for these patients whenever possible in the Emergency setting.
Keywords
Brief focused intervention
Alcohol use
Traumatic brain injury
Emergency and casualty services
INTRODUCTION
Alcohol consumption is an important risk factor in different types of injuries including intentional injuries (violence and suicide) and unintentional injuries (road traffic accidents, falls, buns, and poisoning). Alcohol being a neurotoxin and central nervous system depressant, its acute consumption (even at low to moderate levels) has been shown to affect several crucial functions required for driving including impairments in balance, visual focus, reaction time, judgement, and cognitive functions, which in turn may increase the risk of injury.[1] In 2016, of all deaths attributable to alcohol consumption worldwide, 28.7% were due to injuries and about 40% of alcohol-attributable disability-adjusted life years were due to injuries.[2] In India, prior studies have shown alcohol use to be implicated with road traffic accidents and deaths, physical violence, and injuries occurring while operating machinery.[3-6] Consumption of any amount of alcohol 6 h before the injury significantly increases the risk of injury, and high blood alcohol levels are known to be associated particularly with TBI.[7] Further, prior studies found that alcohol use-related TBI was a significant predictor for future TBI occurring under the influence of alcohol.[8,9]
Prior authors have observed that it is advisable to counsel the patients through brief interventions, preferably when the patient is still feeling the symptoms attached to the TBI,[8] which is considered as a “teachable moment.”[10] Brief interventions have been in use and are highly advantageous, as they can be delivered in a variety of clinical settings. Systematic reviews as well as a series of randomized trials conducted in various healthcare settings have demonstrated that brief interventions have shown significant reduction in alcohol consumption, repeated visits to the emergency and other favorable outcomes, in the target population.[11-16]
In general, considering the high burden of alcohol use-related injuries, the previous authors have observed that harm reduction philosophy needs to be embraced widely including measures aimed at prevention of driving under the influence of alcohol.[3] In this context, nurses are among the best-suited healthcare personnel to deliver brief interventions, as they play a crucial role in delivering or assisting in the delivery of life-saving interventions in the emergency. There is growing evidence that brief interventions delivered by nurses in general medical settings as well as trauma settings are effective in reducing alcohol use in hazardous and harmful users.[17,18] However in India, there is a scarcity of such interventions to reduce harmful and hazardous alcohol use in patients attending emergency hospital services with TBI.
Against the above background, the present study was conducted with the primary objective of evaluating the effectiveness of a nurse-led Brief Focused Intervention (BFI) in comparison with minimal intervention for patients with mild TBI reporting to the emergency and casualty services of a tertiary hospital in South India, who screened positive for alcohol use. We hypothesized that patients, who undergo the BFI (vs. Minimal Intervention Group [MIG]) would show significantly improved outcomes in terms of decreased alcohol use, fewer consequences related to alcohol use, and decreased incidence of re-injuries.
MATERIALS AND METHODS
Setting
We conducted the study at the emergency and casualty services of the National Institute of Mental Health and Neuro Sciences (NIMHANS), Bengaluru, a dedicated center for Neurological, Neurosurgical, and Psychiatric services. The trial was approved by the Institutional Ethics Committee and registered with the Clinical Trials Registry of India (#CTRI/2020/04/024737).
Procedure
Sample size
Using R-software (version R-3.2.1), we calculated the sample size to be 35 × 2, based on the mean scores of pre- (mean: 10.8, standard deviation [SD] = 7.7) and post-interventions (mean: 7.1, SD = 7.4) scores of alcohol use quantity assessed by Alcohol Use Disorders Identification Test (AUDIT).[19] Expecting a 25% attrition in both groups, we estimated the sample size as 90 (45 in each group) at alpha of 0.05 and power of 80%.
Recruitment
The consolidated standards of reporting trials flow diagram for the study is shown in Figure 1. The participants were patients admitted to emergency and casualty services with history of TBI related to use of alcohol, which was defined by any one of the two criteria: (1) reported alcohol use within 6 h prior the injury; and (2) tested positive on breath-alcohol analyzer. Participants were considered for inclusion in the study if they met the following criteria: (a) aged 18 years or above; (b) sustained mild TBI as indicated by a Glasgow Coma Scale score of 13 or more at the time of admission, with or without loss of consciousness; (c) cleared post-traumatic amnesia (PTA); (d) were willing and able to provide informed consent; and (e) were available by phone for follow-up. Patients with history of diagnosed alcohol dependence and patients with severe multiple injuries were excluded from the study.
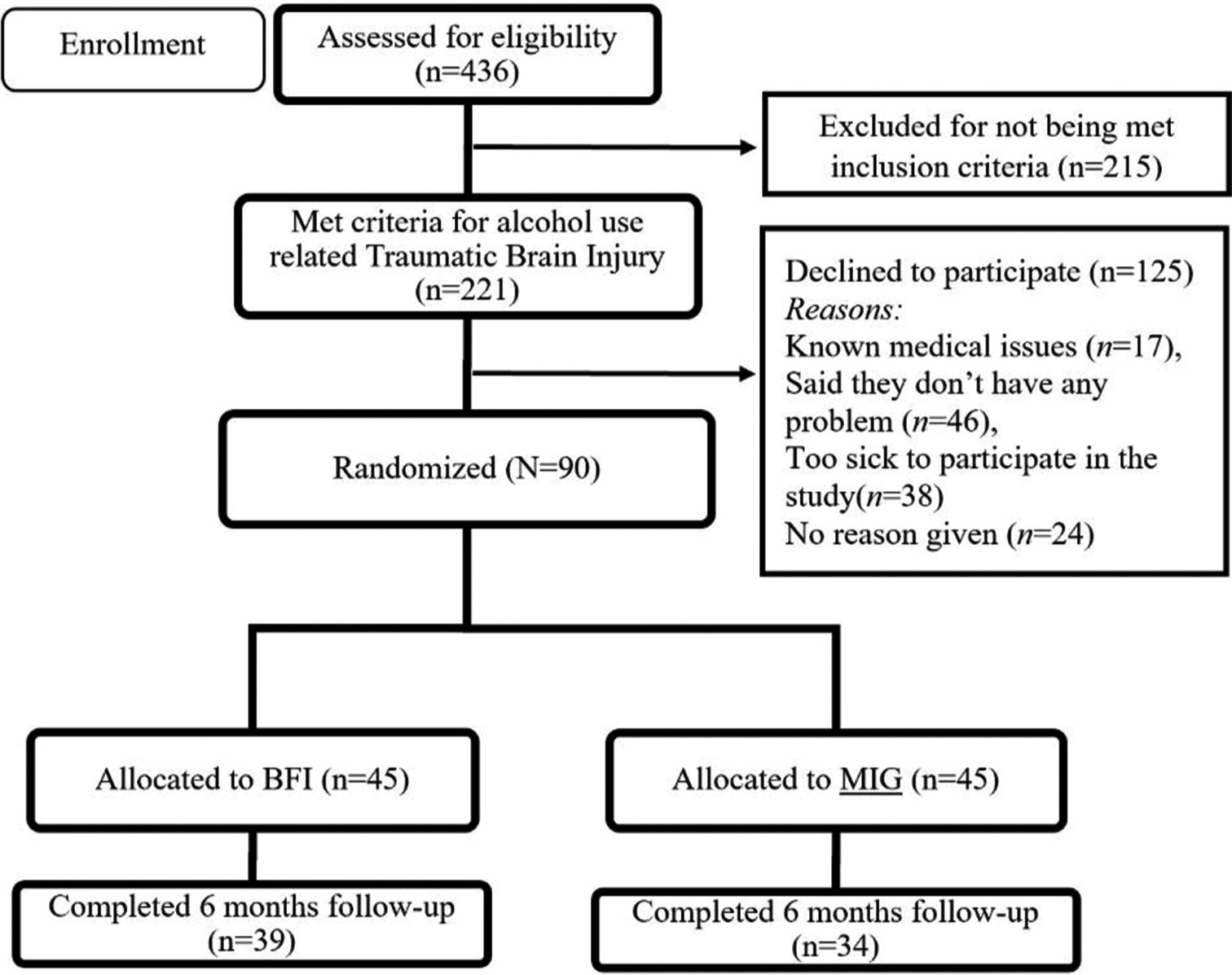
- The consolidated standards of reporting trials flow diagram for the study. BFI: Brief focused intervention, MIG: Minimal intervention group.
The participants were recruited over seven months from July 2021 to January 2022. After screening for eligibility, participants were randomly allotted to one of two groups (BFI/MIG) by the first author using computer-generated random numbers, which were generated with the help of the statistician. The relevant interventions (BFI/MIG) were then provided to the participants by the first author. Of the 90 participants randomized, 73 completed six-month follow-up after discharge until July 2022 (81% follow-up rate).
Interventions provided to each group
Interventions were provided by the first author, who is a registered psychiatric nurse with extensive experience in the field of mental health and addiction psychiatric nursing and had completed online certification programs: (a) SBIRT-Screening, Brief Interventions, and Referral to Treatment at clinical tools, Inc (CTI), National Institute on Drug Abuse (https://sbirt.clinicalencounters.com/) and (b) alcohol training including Brief Intervention And Motivational Interviewing for alcohol use (https://lift.clinicalencounters.com/ce-activity/alcohol/). In addition, she was also trained by the addiction management specialists at the center for addiction medicine, NIMHANS.
MIG
Participants in MIG received the regular treatment protocol offered at the emergency and casualty services of the tertiary care hospital where the study was conducted. This consisted of baseline assessment including screening for alcohol use, provision of emergency care for the injury, providing minimal advice to quit alcohol, and referral to addiction treatment as needed. In addition to this, in the present study, based on the AUDIT score and the result of the serum gamma-glutamyl transferase (GGT) test, feedback was provided to the participants. Further, an educational leaflet containing information about how alcohol use leads to injuries, the benefits of quitting alcohol and tips to quit was given to all the participants in the MIG. Participants were then informed that they would be followed up for up to six months after discharge from the emergency and casualty services.
BFI
We developed the BFI based on the traditional FRAMES (abbreviation for Feedback, Responsibility, Advise, Menu of Options, Empathy and Self efficacy) model.[11] Feedback was based on the AUDIT score and the results of serum GGT. We developed a video with vivid portrayal of the effects of alcohol use on the brain and muscles using computer graphics and brief advice on how to reduce or avoid alcohol use. Participants were encouraged to weigh the pros and cons of their alcohol use behavior, and clear-cut personalized advice was given to stop alcohol use. A menu of options to deal with the high-risk situations was explained with examples. The BFI duration was 7–10 min, which was provided at the time of discharge from the emergency and casualty services to avoid interference with the medical treatment for mild TBI. Following discharge, the first author provided telephonic booster sessions to participants in the BFI group during the 3rd and 5th month with a review of the initial intervention along with reinforcement of any positive behavior change.
Measures
At baseline, sociodemographic details were obtained from the participants. Breath alcohol analyzer test and serum GGT were performed to confirm the presence of alcohol. The GGT is the most commonly used biomarker for alcohol intake, and an elevated level may indicate recent heavy drinking when correlated with the history of drinking.[20]
The PTA was assessed using the Abbreviated Westmead PTA scale (A-WPTAS).[21] Participants with a score of 16 and above were considered to be cleared of PTA.
The AUDIT was used to assess alcohol use in the participants. The AUDIT was developed by the WHO[22,23] and has been extensively used in Asia. Questions 1–3 of the 10-item questionnaire provide information regarding hazardous alcohol use, and Questions 7–10 suggest harmful use of alcohol. Questions 1, 2, and 3 indicate frequency of alcohol use, quantity of alcohol use, and frequency of binge drinking, respectively. The maximum possible score on the AUDIT is 40 with a score of < 8 indicating low-risk drinking.
Consequences of alcohol use were assessed using the short index of problems (SIP-2R)[24,25] with 15 items assessing the consequences in five domains: Impulse control, social responsibility, interpersonal, intrapersonal, and physical.
We assessed the occurrence of re-injury at the end of six months of follow-up as a secondary outcome by enquiring with the patient and corroborating with family members if the patient had any injury after discharge from the emergency and casualty services.
Statistical analysis
We analyzed the data using the statistical Package for the Social Sciences (SPSS-28). Chi-square and Fisher’s exact tests were used to evaluate the associations of group status (BFI vs. MIG) with the discrete measures including education, occupation, marital status, reason for injury, and incidence of loss of consciousness after the injury. For continuous measures (age, monthly income, and GGT values), the non-parametric Wilcoxon signed-rank test was used, as they were not normally distributed. The effectiveness of the intervention was evaluated in terms of changes in the following outcome measures from baseline to six months follow-up: (a) alcohol use measured by AUDIT; (b) consequences related to alcohol use; and (c) incidence of re-injury (secondary outcome). Wilcoxon signed-rank test and Mann–Whitney U test were used to test for statistical significance with regard to the outcome measures (alcohol use and consequences of alcohol use).
Separate binomial regression models were run with significant parameters to examine the predictors for unfavorable outcomes (defined as AUDIT score of ≥ 8). Predictors were identified by examining their association with demographic variables and injury-related parameters. In addition, variables that were found to be significantly associated with unfavorable outcomes in prior studies such as baseline frequency and quantity of alcohol use, frequency of binge drinking, hazardous and harmful use of alcohol, and alcohol-related consequences[26-28] were also included in the model. The final model included the following variables: age, education, baseline AUDIT score, baseline hazardous use of alcohol, baseline frequency of alcohol use, and group status (BFI/MIG).
RESULTS
Baseline characteristics
Baseline characteristics of participants (N = 73) by groups are presented in Table 1. Both the groups were comparable in baseline characteristics.
| Total (N=73) | MIG (n=34) | BFI (n=39) | P-value1 | |
|---|---|---|---|---|
| Age in years [mean (SD)] | 35 (11) | 36 (12) | 34 (10) | 0.47 |
| Education | ||||
| Illiterate (%) | 24.7 | 29.4 | 20.5 | 0.693 |
| Primary and secondary education (%) | 31.5 | 29.4 | 33.3 | |
| Higher secondary education (%) | 43.2 | 41.2 | 46.2 | |
| Occupation | ||||
| Private employee (%) | 38.4 | 32.4 | 43.6 | 0.347 |
| Daily wage worker/others (%) | 61.6 | 67.6 | 56.4 | |
| Monthly income | ||||
| Mean (SD) | 11782.25 (5001.61) | 10176.47 (4999.82) | 11782.05 (4945.48) | 0.173 |
| Median (IQR) | 10000.00 (8000.00) | 8000.00 (5750.00) | 10000.00 (7000.00) | |
| Married (%) | 63.0 | 67.6 | 59.0 | 0.476 |
| Cause of injury | ||||
| RTA (%) | 72.6 | 67.6 | 76.9 | 0.436 |
| Loss of consciousness after injury (%) | 63.0 | 61.8 | 28.2 | 1.000 |
| Breath alcohol positive (%) | 82.2 | 85.3 | 79.5 | 0.557 |
| GGT (IU/L) | ||||
| Mean (SD) | 112.42 (45.47) | 110.35 (44.55) | 114.23 (46.77) | 0.719 |
| Median (IQR)] | 107.00 (42) | 95.50 (59) | 113.00 (39) | |
| AUDIT score | ||||
| Mean (SD) | 12.05 (3.12) | 11.88 (3.22) | 12.21 (3.06) | 0.613 |
| Median (IQR) | 12.00 (5) | 11.50 (4) | 12.0 (6) | |
| Alcohol use-related consequences | ||||
| Mean (SD) | 12.78 (4.02) | 12.59 (4.07) | 12.95 (4.02) | 0.686 |
| Median (IQR) | 13.00 (6) | 12.00 (5) | 13.00 (6) | |
| Hazardous alcohol use | ||||
| Mean (SD) | 5.93 (1.54) | 5.92 (1.59) | 5.94 (1.51) | 0.924 |
| Median (IQR) | 6.00 (2) | 6.00 (2) | 6.00 (2) | |
| Harmful alcohol use | ||||
| Mean (SD) | 6.16 (1.95) | 6.41 (1.88) | 5.88 (2.02) | 0.178 |
| Median (IQR) | 6.00 (4) | 6.00 (4) | 5.50 (3) |
SD: Standard deviation, IQR: Interquartile range, MIG: Minimal Intervention Group, BFI: Brief focused intervention, RTA: Road traffic accident, GGT: Glutamyl transferase, AUDIT: Alcohol use disorder identification test. 1Chi-square and Fisher’s exact test for frequencies, Mann–Whitney U-test for continuous variables, N: Total number of participants
Study outcomes
Primary outcomes
Change in alcohol consumption assessed by AUDIT score (baseline vs. 6 months)
Changes in alcohol consumption are presented in Table 2. At the end of six months, there was a significant change in the AUDIT score in both groups. However, the BFI group when compared with MIG reported a significant decrease in alcohol consumption in terms of AUDIT score (5.03 [4.09] vs. 9.76 [2.96]; P < 0.001).
| Outcome | Total (N=73) | MIG (n=34) | BFI (n=39) | P-value1 |
|---|---|---|---|---|
| AUDIT score | ||||
| Mean (SD) | 7.23 (4.30) | 9.76 (2.96) | 5.03 (4.09) | <0.001* |
| Median (IQR) | 8.00 (7) | 11.00 (4) | 5.00 (9) | |
| CI | 8.73, 10.80 | 3.70, 6.35 | ||
| Alcohol use-related consequences | ||||
| Mean (SD) | 4.99 (2.87) | 5.88 (2.59) | 4.18 (3.21) | <0.001* |
| Median (IQR) | 5.00 (4) | 5.00 (3) | 3.00 (3) | |
| CI | 4.98, 6.79 | 3.14, 5.22 |
Changes in the alcohol-related consequences assessed by SIP-2R score (baseline vs. 6 months)
A significant difference in alcohol-related consequences (SIP-2R score) between baseline to six months follow-up was seen in both groups. However, the difference was higher in the BFI group when compared with the MIG (4.18 [3.21] vs. 5.88 [2.59]), suggesting that BFI group participants experienced significantly lesser consequences related to alcohol use (<0.001). Further, details are provided in Table 2.
Secondary outcome
There were no re-injuries among the study participants in both the groups at the end of six months follow-up.
Predictors for unfavorable outcome
Results of separate logistic regression analysis for the individual groups showed that age (odds ratio [OR] = 1.225, confidence interval [CI] = 1.009, 1.486) was associated with unfavorable outcome in the MIG while baseline AUDIT score (OR = 1.282, CI = 1.001, 1.642) and hazardous use (OR = 1.868, CI = 1.127, 3.098) were associated with unfavorable outcome in BFI group.
Results of logistic regression for the total sample showed that baseline frequency of alcohol use and hazardous use was associated with unfavorable outcomes. Further, not being in the BFI group was five times more likely to be associated with unfavorable outcome at the end of six months follow-up [Table 3].
| OR | 95% CI | P value | |
|---|---|---|---|
| Group1 | 4.797 | 1.682–13.679 | 0.003* |
| Frequency of alcohol use at baseline | 10.014 | 1.569–63.913 | 0.015* |
| Hazardous alcohol use at baseline2 | 1.538 | 1.083–2.184 | 0.016* |
DISCUSSION
To the best of our knowledge, this is the first study in India evaluating the effectiveness of a nurse-led BFI for patients, who presented to the emergency and casualty services with alcohol use-related TBI. We developed the BFI with the aim of educating patients in an easily understandable manner about the adverse impact of alcohol use in terms of impaired driving skills due to the involvement of the brain and musculoskeletal system leading to injuries. Since participants with mild TBI may be under stress and find it difficult to concentrate, the BFI was largely video-based to facilitate better understanding and be more acceptable to the patients. With regard to the content of the video, the effects of alcohol on driving were portrayed with relevant real-life situational illustrations in the local language. The BFI was provided on a one-to-one basis to facilitate better comprehension and response from the patients.
Our study has shown that the BFI was effective in reducing the quantity and frequency of alcohol use, alcohol use-related consequences, which is supported by overseas studies.[14,15,29,30] In our study, there were no re-injuries in either BFI and MIG groups; however, prior studies in emergency settings have indicated that re-injuries reduced post-intervention.[31,32] Further, our study, which involved a nurse-led intervention, was effective in reducing alcohol use and related consequences in the patients, which is in line with several prior studies involving nurse-delivered brief interventions in different populations.[16,17,30]
In our study, we also sought to determine the predictors for unfavorable outcomes in terms of AUDIT score (≥8) at the end of six months. The findings showed that receiving BFI significantly lowered the risk of unfavorable outcomes during follow-up. In addition, baseline frequency of alcohol use and hazardous use were significantly associated with unfavorable outcomes at the end of six months, which finds support in previous studies.[26,27,33] This reinforces the need for emergency-based brief interventions to improve outcomes following TBI.
The above findings, while statistically significant, can be considered to be highly relevant from a clinical point of view as well as they show that it is feasible to carry out brief interventions for this population (viz., patients with alcohol use-related mild TBI) in the emergency setting and that such interventions can be effective. It should also be borne in mind that it is not possible to define a minimal clinically important difference with such interventions. However, given that there are no known structured interventions in India that have been tested for effectiveness in patients, who present to emergency services with alcohol use-related mild TBI, the present study’s findings can be considered promising.
In addition, we found that participants in MIG also had changes in outcome measures in terms of a decrease in AUDIT score and alcohol use-related consequences from baseline to six months, which might have been the result of being included in the study. The participants in MIG were given an educational leaflet and followed up for six months post-discharge, which may have accounted for these changes in outcome measures, which is also supported by a previous study by Désy et al.[18] Therefore, adapting these interventions into routine emergency care is recommended.
The challenges encountered during the study period were as follows: (a) patients were reluctant to enroll in the study due to stigma and legal implications, (b) extremely busy emergency and casualty services and fast turnover of patients leading to loss of sample before recruitment, and (c) difficulty conducting follow-up due to disconnected phones, and not coming for follow-up at the stipulated time. By the end of the study, 19% were lost to follow-up, which was however within the estimated attrition rate of 25%. The observed retention rate (81%) is much higher than previous studies.[17,34]
A major limitation of the study is that the first author was not blinded to the group allocation; however, group allocation was carried out strictly according to the random numbers. Hence, there was no way for the first author to know beforehand to which group each participant would get allotted to. Another limitation is that the intervention and follow-up assessments were conducted by the first author. Furthermore, the influence of other moderating factors such as family and peer support in improving outcomes was not verified.
Despite the above limitations, our study has some important implications: Firstly, in low- and middle-income countries, the burden due to alcohol use-related TBI is rising; however, interventions for reducing alcohol use are almost nonexistent. Hence, it is important to include interventions like BFI in routine emergency care to prevent further severe injuries. Second, nurses in the emergency and casualty services should be trained to screen for alcohol use and deliver these interventions. Third, nurse administrators should ensure that training for such interventions are integrated into the nursing curriculum as well as in-service education. Fourth, further research should be carried out with larger sample size and longer follow-ups as well as in multiple trauma care settings. Fifth, emergency and casualty services interventions require dedicated administrative support so that they become part of the organizational culture.
CONCLUSION
Our study has demonstrated that the nurse-led BFI for patients with alcohol use-related mild TBI in the emergency and casualty services was effective in reducing the patients’ alcohol use when compared to the MIG. The intervention developed is brief and simple with clear information and advice and can be integrated into routine emergency and casualty services. Thus, it has significant potential in terms of reducing alcohol use-related TBI and visits to emergency and casualty services when integrated into routine emergency care.
Ethical approval
The research/study is approved by the Institutional Ethics Committee, number NIMH/DO/IEC (BEH. Sc. DIV)/2020, dated 24th March, 2020.
Patient consent declaration
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Dose-related effects of alcohol on cognitive functioning. PLoS One. 2012;7:e50977.
- [CrossRef] [PubMed] [Google Scholar]
- Magnitude of substance use in India New Delhi: Ministry of Social Justice and Empowerment, Government of India; 2019.
- [Google Scholar]
- Road accidents in India 2019 In: Ministry of housing and urban affairs. India: MORTH; 2019. p. :1-97.
- [Google Scholar]
- Burden, pattern and outcomes of road traffic injuries in a rural district of India. Int J Inj Contr Saf Promot. 2016;23:64-71.
- [CrossRef] [PubMed] [Google Scholar]
- Characteristics associated with alcohol consumption among emergency department patients presenting with road traffic injuries in Hyderabad, India. Injury. 2016;47:160-5.
- [CrossRef] [PubMed] [Google Scholar]
- Alcohol intake and the pattern of trauma in young adults and working aged people admitted after trauma. Alcohol Alcohol. 2005;40:269-73.
- [CrossRef] [PubMed] [Google Scholar]
- Recurrent traumatic brain injury is predicted by the index injury occurring under the influence of alcohol. Brain Inj. 2008;22:780-5.
- [CrossRef] [PubMed] [Google Scholar]
- Head trauma sustained under the influence of alcohol is a predictor for future traumatic brain injury: A long-term follow-up study. Eur J Neurol. 2014;21:293-8.
- [CrossRef] [PubMed] [Google Scholar]
- Alcohol counseling in hospital trauma: Examining two brief interventions. J Couns Dev. 2018;96:243-53.
- [CrossRef] [Google Scholar]
- Brief interventions for alcohol problems: A review. Addiction. 1993;88:315-35.
- [CrossRef] [PubMed] [Google Scholar]
- A systematic review of emergency care brief alcohol interventions for injury patients. J Subst Abuse Treat. 2008;35:184-201.
- [CrossRef] [PubMed] [Google Scholar]
- Systematic review and meta-analyses of strategies targeting alcohol problems in emergency departments: Interventions reduce alcohol-related injuries. Addiction. 2008;103:368-76.
- [CrossRef] [PubMed] [Google Scholar]
- The cost-effectiveness of alcohol screening, brief intervention, and referral to treatment (SBIRT) in emergency and outpatient medical settings. J Subst Abuse Treat. 2015;53:1-8.
- [CrossRef] [PubMed] [Google Scholar]
- Investigation of the effectiveness of brief interventions to reduce alcohol consumption following traumatic brain injury. J Head Trauma Rehabil. 2012;27:331-41.
- [CrossRef] [PubMed] [Google Scholar]
- A randomized controlled trial of brief intervention for problem alcohol use in persons with traumatic brain injury. J Head Trauma Rehabil. 2012;27:319-30.
- [CrossRef] [PubMed] [Google Scholar]
- Nurse-delivered brief interventions for hazardous drinkers with alcohol-related facial trauma: A prospective randomised controlled trial. Br J Oral Maxillofac Surg. 2008;46:96-101.
- [CrossRef] [PubMed] [Google Scholar]
- Alcohol screening, brief intervention, and referral to treatment conducted by emergency nurses: An impact evaluation. J Emerg Nurs. 2010;36:538-45.
- [CrossRef] [PubMed] [Google Scholar]
- The effectiveness of brief intervention among injured patients with alcohol dependence: Who benefits from brief interventions? Drug Alcohol Depend. 2010;111:13-20.
- [CrossRef] [PubMed] [Google Scholar]
- Biomarkers of alcoholism: An updated review. Scand J Clin Lab Invest. 2008;68:81-92.
- [CrossRef] [PubMed] [Google Scholar]
- Validation of the abbreviated westmead post-traumatic amnesia scale: A brief measure to identify acute cognitive impairment in mild traumatic brain injury. Brain Inj. 2011;25:1198-205.
- [CrossRef] [PubMed] [Google Scholar]
- Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88:791-804.
- [CrossRef] [PubMed] [Google Scholar]
- AUDIT In: The alcohol use disorders identification test: Guidelines for use in primary health care. Geneva: World Health Organization; 2001.
- [Google Scholar]
- Psychometric properties of the short index of problems as a measure of recent alcohol-related problems. Alcohol Clin Exp Res. 2003;27:1436-41.
- [CrossRef] [PubMed] [Google Scholar]
- The Drinker Inventory of Consequences (DrInC): An instrument for assessing adverse consequences of alcohol abuse: Test manual United States: US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute on Alcohol Abuse and Alcoholism; 1995.
- [Google Scholar]
- How do risk factors work together? Mediators, moderators, and independent, overlapping, and proxy risk factors. Am J Psychiatry. 2001;158:848-56.
- [CrossRef] [PubMed] [Google Scholar]
- Severity of baseline alcohol use as a moderator of brief interventions in the emergency department. Alcohol Alcohol. 2009;44:486-90.
- [CrossRef] [PubMed] [Google Scholar]
- Family member involvement in relapse prevention improves alcohol dependence outcomes: A prospective study at an addiction treatment facility in India. J Stud Alcohol Drugs. 2010;71:581-7.
- [CrossRef] [PubMed] [Google Scholar]
- Screening and brief intervention for substance misuse among patients with traumatic brain injury. J Trauma. 2010;69:722-6.
- [CrossRef] [PubMed] [Google Scholar]
- Alcohol use at the time of traumatic brain injury: Screening and brief intervention in a community hospital. J Trauma Nurs. 2017;24:116-24.
- [CrossRef] [PubMed] [Google Scholar]
- Emergency department brief motivational interventions for alcohol with motor vehicle crash patients. Ann Emerg Med. 2005;45:620-5.
- [CrossRef] [PubMed] [Google Scholar]
- Alcohol interventions among underage drinkers in the ED: A randomized controlled trial. Pediatrics. 2015;136:e783-93.
- [CrossRef] [PubMed] [Google Scholar]
- Video-enabled cue-exposure-based intervention improves postdischarge drinking outcomes among alcohol-dependent men: A prospective study at a government addiction treatment setting in India. J Ethn Subst Abuse. 2018;17:532-47.
- [CrossRef] [PubMed] [Google Scholar]
- Effectiveness of brief interventions after alcohol-related vehicular injury: A randomized controlled trial. J Trauma. 2006;61:523-31.
- [CrossRef] [PubMed] [Google Scholar]






