Translate this page into:
Cystic mature teratoma of the thoracic region in a child: An unusual case
Address for correspondence: Dr. Askin Esen Hasturk, Department of Neurosurgery, Oncology Training and Research Hospital, Vatan Caddesi, 06200 Demetevler, Ankara, Turkey. E-mail: aehasturk@yahoo.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Cystic mature teratomas of the spinal cord are rare lesions. Teratomas account for up to 0.1% of all spinal cord tumors. Teratomas include tissues that originate from the three germ layers. Several congenital disorders may accompany the teratoma. Teratomas are classified as mature, immature or malignant type according to their histological characteristics. Thoracic spinal teratomas are uncommon in the pediatric age group. More than half of the patients are adults. We present herein a five-year-old male patient who was referred to our clinic with cystic mature teratoma at the T12 level.
Keywords
Mature teratoma
spinal tumor
thoracic region
treatment
Introduction
Cystic mature teratomas of the spinal cord are rare lesions. Teratomas account for up to 0.1% of all spinal cord tumors. Teratomas include tissues that originate from the three germ layers.[1–3] Several congenital disorders may accompany the teratoma. Teratomas are classified as mature, immature or malignant type according to their histological characteristics.[3–5]
Case Report
A five-year-old male patient who experienced increasing pain in his waist and legs with accompanying numbness and gait disability was referred to our clinic. Numbness and weakness in the legs of the patient became particularly evident in the last 10 days. In addition, urinary incontinence and gait disability were seen in the clinical table. Neurological examination revealed paraparesis and loss of sensation in the dermatome under the T12 level. A pronounced decrease was seen in the deep tendon reflex; no other pathologies were present in the systemic examinations. In the spinal magnetic resonance imaging (MRI), an intradural and extramedullary capsular cystic mass measuring 40 × 17 × 16 mm was detected at the T12 level and was observed to be pressing on the right side of the cord, with no large amount of contrast. The spinal duct was detected to be large at that site [Figure 1a, b]. No additional pathologies were determined in the radiological imaging of the spinal axis and cranial region. The patient was operated according to these findings and signs. Laminoplasty was performed for this tumor. After midline incision of the dura, the mass was removed. Pathological evaluation was positive for cystic mature teratoma diagnosis. The histopathological examination revealed a cystic formation covered by columnar epithelial tissue in some regions and with a pseudostratified appearance in some regions as well. Mucous gland formations, mature cartilage tissue and vessel and nerve sections were also detected in the cyst wall [Figure 2a, b]. Postoperative follow-up showed a dramatic recovery in the neurological table [Figure 3a, b]
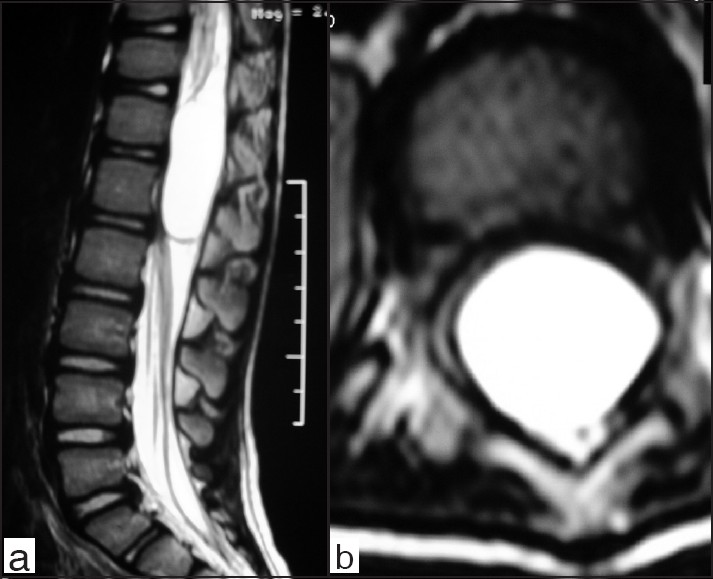
- (a) Sagittal (b) axial T2-weighted MR images showing an intradural extramedullary mass lesion compressing the dural sac.
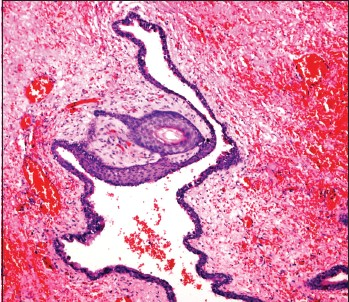
- Squamous epithelium in hemorrhagic background (H and E ×100)
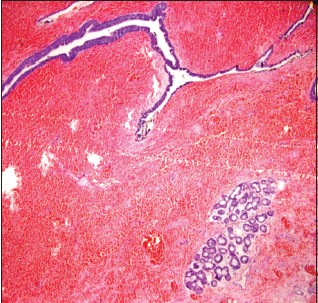
- Mucous glands beneath the squamous epithelium (H and E×100)
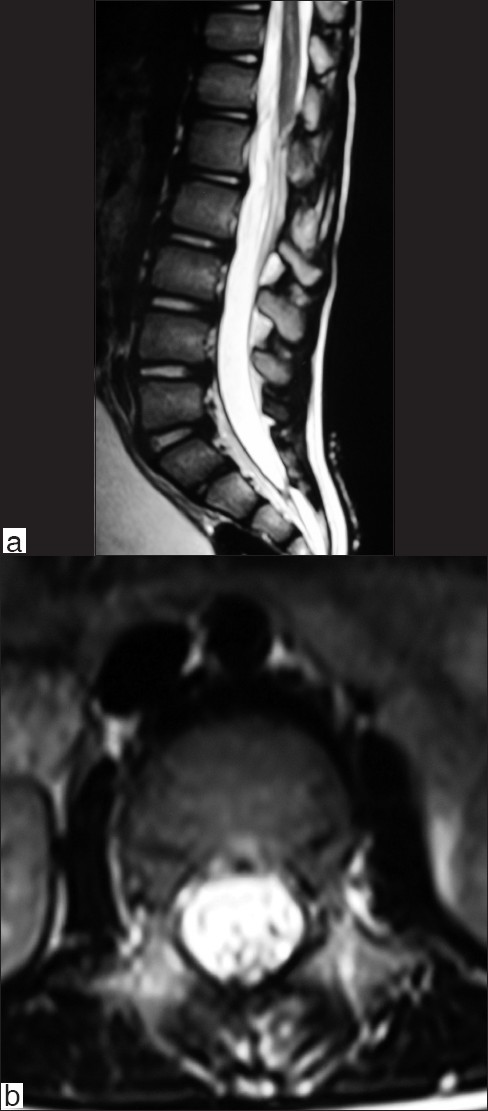
- (a) Sagittal (b) axial T2-weighted MR images do not revealing any residual or recurrent mass lesion postoperatively.
Discussion
Spinal teratomas are rarely seen and occur as a result of a combination of cells, which originate from the three germinal layers; however, endodermal layers do not always accompany the tumor. The tumors arising from only two germinal layers are called “teratoid” or “bigerminal teratoma”. Teratomas are also referred to as teratomatous cyst, cystic teratoma, teratoid tumor, or atypical teratoma.[2–4] While the pathogenesis of spinal teratoma remains controversial, there are some theories regarding its development, the most accepted of which is based upon the fact that the primordial germ cells that originate from the yolk sac are located at a different site due to alteration during cell migration in early embryogenesis.[145] The first patient was reported to be diagnosed in 1863 by Virchow.[46] Intradural spinal teratomas account for up to approximately 0.1% of all the spinal tumors, and they may be extradural, intradural or intramedullary.[1267] Poeze determined 83 patients with spinal teratoma in 1999, of which 31 (37%) were intramedullary teratoma, and 58% of teratomas were detected in adult patients.[89] Other abnormalities such as diastematomyelia, myelomeningocele and tethered cord may accompany spinal teratoma.[236] Therefore, when the final diagnosis of a spinal teratoma is established, the spinal cord should be examined completely in order to determine the possible abnormalities accompanying spinal dysraphism. Teratomas are divided into three groups histologically as mature, immature and malignant teratoma.[357] The detection of immature sections in case of teratoma is important for the diagnosis and the disease course. Benign lesions mainly include mature tissues such as cartilage, squamous epithelium, gland formations, mucosa, and neural sections. The most frequently seen immature type is the primitive cells of the neuroepithelial cell line, from which the majority of the recurrences arise. The prognosis is poor in malignant teratomata.[1367] Computed tomography (CT) and MRI are the basic methods in the detection of intraspinal teratoma. Both methods can easily show the heterogeneous tumor. However, neither MRI nor CT examination is definitive for the final diagnosis. The signs and findings of the teratoma may mimic the other spinal masses or demonstrate the acutely increasing or intermittently increasing characteristics. Computed tomography (CT) can show calcifications, fat and soft tissue densities. MRI is the gold standard diagnostic technique for preoperative diagnosis of teratomas as for other intraspinal tumors. MRI can show different tissues and the finding of mixed high- and low-intensity signals reflects the cystic and solid compositions of the tumor. Presence of enhancing soft tissue components and its relation to surrounding structures are best demonstrated by the MRI. The presence of a cystic lesion showing fluid, fat and calcifications are diagnostic of teratoma.[2389] The final diagnosis is only established with histological examination. The tumor may be hypointense in T1-weighted sections, while it is hyperintense in T2-weighted sections in some cases. However, due to excessive fat in some cases, it may be hyperintense in T1-weighted sections and hypointense in T2-weighted sections.[1–3] Because of the combination of factors like calcification, soft tissue, fat tissue, and cyst, a complex appearance may be obtained with MRI. If cysts accompany the teratoma, then it is called a teratomatous cyst, and they are frequently small in size. Larger cysts are formed by the combination of numerous small-sized cysts and should not be considered as a different pathological entity.[2356] The objective of the surgical operation in spinal teratoma is the total resection of the mass to the extent possible. The total surgical resection establishes the major prognostic factor together with the histological diagnosis of the tumor. Although these tumors are frequently covered by a capsule, they generally are adhered to nerve roots and the spinal cord.[2467] We performed laminoplasty for tumor. Laminoplasty has been developed to prevent the formation of adhesion surrounding tissue, membrane of laminectomy, instability and kyphosis in intraspinal patology after laminectomy. Replacement of laminar roof with this technique is safe, well-suitable and offers distinct advantages over laminectomy. The role of radiotherapy in case of mature teratoma is limited. Radiotherapy and chemotherapy may be applied in the treatment of malignant and immature teratoma. MRI follow-up is suggested if radical surgery is not indicated for the mature intramedullary teratoma.[1259] In the event of recurrence, a second operation may be performed. Although teratomas are generally benign tumors histologically, research shows a recurrence rate of 10%, since the tumor may not be radically removed.[368] Recurrence periods up to nine years after the surgical intervention have been reported. The long latent follow-up periods are associated with the gradual growth of the tumor. The survival rates of the spinal mature teratomata are good, while the patients with malignant or immature teratoma die within one year after the surgery.[1289]
Conclusions
In conclusion, thoracic spinal teratomas are uncommon in the pediatric age group. The tumor is generally located at the conus site in adult patients, while it is frequently larger sized in children and located at thoracic and cervical sites. Should the tumor not be removed radically, the survival without recurrence may be extended.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Clinicopathological study of spinal teratomas. A series of 10 cases. J Neurosurg Sci. 2003;47:95-100.
- [Google Scholar]
- Spinal teratomas: A clinicopathological study of 27 patients. Acta Neurochir. 2009;151:245-52.
- [Google Scholar]
- Intradural spinal teratoma: Evidence for a dysembryogenic origin. J Neurosurg. 1998;89:844-51.
- [Google Scholar]
- Cystic mature teratoma of the filum terminale in an adult. Case report and review of the literature. Neurocirugia (Astur). 2004;153:290-3.
- [Google Scholar]
- Central nervous system germ cell tumors: Classification, clinical features, and treatment with a historical overview. J Child Neurol. 2009;24:1439-45.
- [Google Scholar]
- Clinicopathological study of seven cases of spinal cord teratoma: A possible germ cell origin. Histopathology. 1998;32:51-6.
- [Google Scholar]
- Intramedullary spinal teratoma presenting with urinary retention: Case report and review of the literature. Neurosurgery. 1999;45:379-85.
- [Google Scholar]
- Spinal teratoma: Is there a place for adjuvant treatment. Two cases and a review of the literature? Br J Neurosur. 2000;14:482-8.
- [Google Scholar]






