Translate this page into:
Recurrent meningitis in a child with intranasal encephalocele
Address for correspondence: Dr. Edwin Dias, Department Pediatrics, S-3, Casa Leila Apts, S.L. Mathias Road, Highlands, Mangalore – 575 002, Karnataka, India. E-mail: dredwindias@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Recurrent bacterial meningitis in children necessitates a need to search for an underlying cause, either altered immune status or a craniospinal defect. In the absence of immunodeficiency, anatomical anomalies must be investigated thoroughly to rule out an intranasal encephalocele, as it is one of the important causes. Most cases go unnoticed till late childhood due to the hidden nasal mass only to be diagnosed due to recurrent meningitis. In a their study on recurrent bacterial meningitis, Tebruegge highlights that around 59% of the cases were due to anatomical defects, 36% related to immunodeficiency's, and 5% parameningeal infections.[1] In addition, the bacterial specificity could leave significant clues: Pneumoccocus, H. influenzae suggests cranial dural defects, E. coli or other gram negative bacilli suggests spinal dural defects, and meningococci suggest immunologic deficiency.[2]
An 11-year-old girl presented to a rural hospital with an history of fever, neck stiffness, headache, vomiting, breathing difficulties, and intermittent watery discharge of 5 years duration from the right nostril more since 3 days prior to admission. The child had altered sensorium and two episodes of generalized tonic clonic seizures 3 h prior to admission. She had suffered similar complaints 1 year back where she was admitted, and treated with intravenous antibiotics. There was no history of prior head trauma or immunodeficiency. She was a product of a non-consanguineous marriage, normal intelligence, fully vaccinated, and unremarkable family history. The child was going to school regularly. On physical examination, she had fever; her weight was 33 kg, height 143 cm, and head circumference 53 cm which was normal for her age. She had marked hypertelorism with mild proptosis and widened root of the nose. There was a pulsating mass in the right nostril with mucopurulent discharge. Her nasal septum was deviated to the left. The mass was transilluminant. The nervous system examination revealed right upper motor neuron facial palsy with papilledema and signs of meningitis. The other systems were normal.
Laboratory investigations revealed leucocytosis with neutrophilia, increased CRP, decrease in glucose concentration and increased protein in the CSF sample, the cell count was 1700/mm3 and was predominantly neutrophilic. Gram's stain of the CSF revealed plenty of PMNL's with gram-positive cocci in pairs and short chains. Culture of the CSF grew Streptococcus Pneumoniae. X-ray paranasal sinus showed a mass in the right nostril. Cranial CT scan showed a large defect in the right transethmoidal region with a large mass filled with fluid [Figure 1]. The pediatric history (no trauma) and clinical symptoms indicate an inherited defect at the base of the skull with encephalocele. She was treated with Ceftriaxone 2 g IV for 14 days. She recovered completely. The patient was then operated for closure of encephalocele. At review, 6 months later she was doing well and her neurological development was normal.
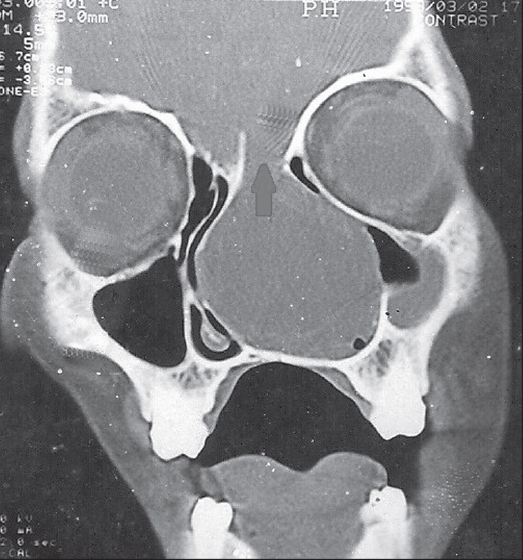
- Cranial CT scan showed a large defect in the right transethmoidal region with a large mass filled with fluid
Encephaloceles are rarely reported in the western countries, but South Asia has a higher incidence of 1:5000 live births.[3] There is one reported case of transethmoidal encephalocele from India.[4] The intranasal encephalocele is accompanied by a widened nasal route and increased intraocular distance until the occurrence of nasal obstruction, epistaxis or recurrent episodes of bacterial meningitis.[5] Since an intranasal encephalocele presents with a mass in the nose, it may be mistaken for a nasal polyp and removal can lead to potentially fatal outcome. Other differential diagnosis includes nasal glioma, dermoids or teratomas in the same region. Therefore, CT scan, MRI, and MR cisternography should be done in these patients prior to biopsy to confirm the diagnosis.[6] To minimize patient morbidity, mortality, and to provide excellent cosmetic result various surgeries like endoscopic sinus surgery[7] and one stage corrections with hemiorbital advancement[6] are available. In our patient the outcome was excellent as there were no other associated abnormalities, with no evidence of post operative hydrocephalus even on follow up.
References
- Epidemiology, etiology, pathogenesis, and diagnosis of recurrent bacterial meningitis. Clin Microbiol Rev. 2008;21:519-37.
- [Google Scholar]
- Diagnostic approach to recurrent bacterial meningitis in children. Chang Gung Med J. 2005;28:441-52.
- [Google Scholar]
- Geographical distribution of frontoethmoidal encephalocole. Br J Prev Soc Med. 1972;26:193-8.
- [Google Scholar]
- CSF rhinorrhea and recurrent meningitis caused by transethmoidal meningoencephalocele. Indian Pediatr. 2005;42:1033-4.
- [Google Scholar]
- Anterior encephalocoeles: A series of 103 cases over 32 years. J Clin Neurosci. 2006;13:536-9.
- [Google Scholar]





