Translate this page into:
Retrograde thromboembolism and recurrent stroke in an adolescent boy with bilateral cervical rib
*Corresponding author: Manas Ranjan Behera, Departments of Pediatrics, Kalinga Institute of Medical Sciences, Bhubaneswar, Odisha, India. drmrb73@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Behera MR, Mohapatra M, Das P, Reddy A, Gyandeep G. Retrograde thromboembolism and recurrent stroke in an adolescent boy with bilateral cervical rib. J Neurosci Rural Pract. 2024;15:399-401. doi: 10.25259/JNRP_385_2023
Dear Editor,
Arterial ischemic stroke is the predominant form of stroke seen in children. The major risk factors are infections, congenital heart disease, sickle cell disease, trauma, malignancy, and congenital or acquired hypercoagulable states.[1] The cervical rib is a rare skeletal anomaly, which can compress the neurovascular structures exiting from the thorax and give rise to a constellation of symptoms and signs, termed “thoracic outlet syndrome” (TOS). Chronic pressure on the subclavian artery (SCA) can lead to thrombosis, diminished or absent radial and brachial pulses, claudication, gangrenous changes at fingertips, and rarely cerebral stroke.[2,3]
A 13-year-old boy presented with a left-side weakness for two days, which was sudden in onset, progressive, and associated with same-side facial weakness. There was a history of intermittent headache, pain, and tingling sensation in the left upper limb aggravated by exertion and relieved by rest and analgesic medications for the past two months. There was no history of vomiting, loose stools, abnormal body movements or diplopia.
On physical examination, right radial and brachial pulses were not palpable, and blood pressure was also not recordable on that side. On the left, the radial artery pulse was 82/min, and blood pressure was 124/80 mmHg. On local examination of the right upper limb, it was found to be slightly cold with delayed capillary refilling time without any loss of function. Neurological examination was suggestive of dysarthria, left upper motor neuron type facial palsy, and left-side hemiparesis.
In view of the presence of pulselessness and hemiparesis, a diagnosis of “Takayasu arteritis with stroke” was made and investigated. He had normal blood counts; erythrocyte sedimentation rate and C-reactive protein were normal. Liver and renal function tests, lipid profile, procoagulant work-up (protein C, protein S, anti-thrombin III, factor V Leiden, and MTHFR mutation), and vasculitis profile were normal. He had no clinical or laboratory evidence of sickle cell disease or tuberculosis. A 2D echocardiography was also normal. Computed tomography (CT) brain showed acute infarct in the right corona radiata with few foci of subacute to chronic infarct in the left temporal lobe, pons, left cerebellar hemisphere, and basal ganglia. A CT angiogram of the brain showed complete occlusion of the distal part of the basilar artery suggestive of thrombosis, non-visualization of the M2 segment of the right middle cerebral artery [Figure 1] and infarction as described before. Imaging of the aorta was normal without any evidence of arteritis or dissection. The CT angiogram of the neck showed a bilateral cervical rib (left longer than right) and thrombosis of the right SCA, which is seen to course just below the right cervical rib. Right upper limb angiography showed complete occlusion of right SCA, axillary, and brachial arteries along with collaterals [Figure 2]. He was initially managed conservatively followed by low molecular weight heparin and later started on aspirin. There was a significant improvement in weakness and facial palsy. Surgical excision of the cervical rib was deferred as the patient was recovering. He was discharged with aspirin and is currently on follow-up.
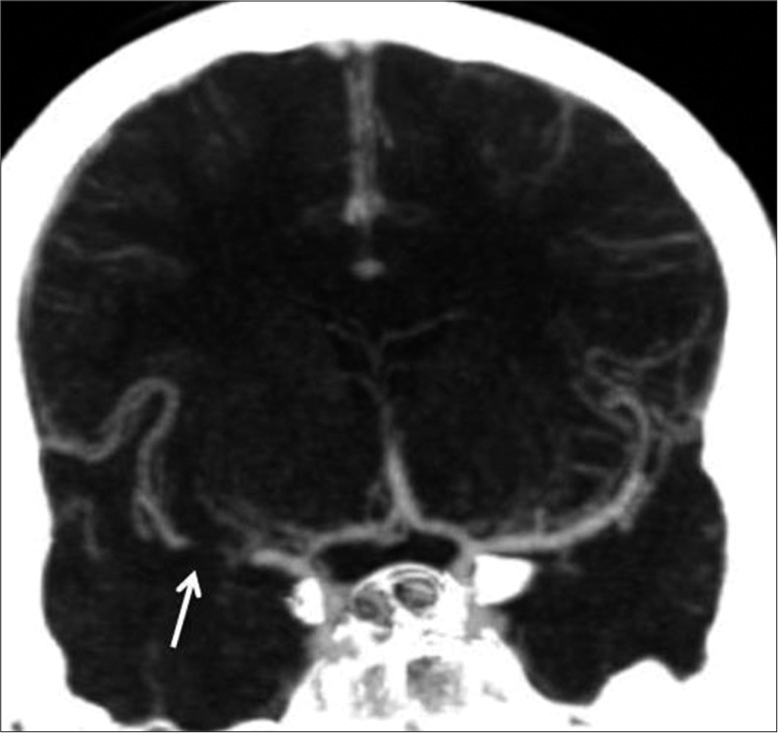
- Coronal computed tomography angiography maximum intensity projection image showing occlusion (thin arrow) of proximal right middle cerebral artery.
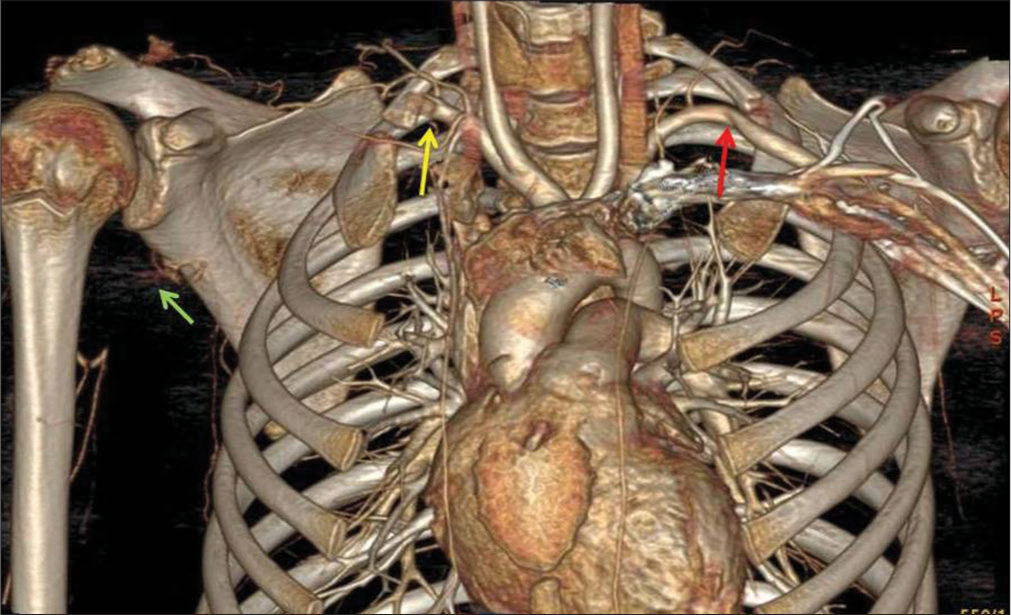
- Three-dimensional volume-rendered computed tomograph angiographic image showing occlusion of right subclavian artery (yellow arrow) below the cervical rib, collaterals in the arm (green arrow), and mild narrowing of left subclavian artery (red arrow).
The TOS is classified into arterial (subclavian and axillary artery compression, 1%), venous (subclavian and axillary vein compression, 4%), and neurogenic (brachial plexus compression, 95%).[4] Arterial TOS is characterized by potential life-threatening and limb-threatening thromboembolic complications.
The cervical rib also known as “Eve’s rib” is an anomalous, supernumerary rib that arises from the seventh cervical vertebra. The prevalence varies from 0.58% to 6.2%.[5] They can be unilateral or bilateral, usually asymmetrical, and may be found to be attached to the first rib. They are asymptomatic in 90% of the cases; more common in females and are one of the major causes for TOS. Our case had bilateral cervical ribs attached to the first ribs on both sides. Compression of the SCA by the cervical rib at the base of the interscalene triangle, chronic arterial spasm induced by the pressure, and turbulent flow at the site causing shearing stress of the arterial wall leading to intimal injury are the triggering factors for thrombus formation.[6] Further, stenosis at the compression site with post-stenotic dilatation and aneurysm formation predisposes to thrombosis, and the thrombus can embolize both distally and proximally.
The clinical symptoms due to vascular occlusion and antegrade embolization include loss of peripheral pulse, paresthesia and mild discoloration of hand, claudication, coldness, digital ischemia, and gangrene. Ischemic symptoms may be diminished by the formation of collaterals.
Overhead abduction and rotation of the arm can cause complete occlusion of the SCA leading to retrograde flow from SCA to common carotid and vertebral arteries (CCA and VA) resulting in thromboembolism and stroke. Stroke is more common on the right side due to the common origin of the CCA and VA from the brachiocephalic trunk.[7] Further, anterior circulation strokes are more commonly described to be associated with cervical rib, which may be due to larger caliber and lesser resistance in the CCA.[8] Our case had involvement of both anterior and posterior circulation, which is very rare.
A few plausible explanations have been put forward by some authors to explain the mechanism of retrograde embolism, namely, positional flow reversal in SCA, upstream mobilization of lesser dense thrombus, the venturi effect, and the Bernoulli principle. In our case, the boy had narrowing of both the right and left subclavian arteries and evidence of thrombotic occlusion on the right side. We presume that the infarctions of the brain at multiple sites can be due to retrograde embolization from the thrombus in the right SA at different times affecting both anterior and posterior circulation.
Anticoagulant therapy should be started as the first line of management in patients presenting with thrombosis. Removal of the cervical rib in the presence of SA thrombosis can cause the collapse of the thrombus and additional embolization to the brain. Further, due to the lack of enough evidence in children, surgery is usually deferred until the end of skeletal growth in pre-adolescents.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Arterial ischemic stroke in children: Risk factors and etiologies. Curr Neurol Neurosci Rep. 2014;14:422.
- [CrossRef] [PubMed] [Google Scholar]
- Recurrent stroke in young: Rule out a cervical rib! Ann Indian Acad Neurol. 2021;24:286-8.
- [CrossRef] [PubMed] [Google Scholar]
- Stroke caused by arterial thoracic outlet syndrome in an adolescent. Child Neurol Open. 2022;9:2329048X221105743.
- [CrossRef] [PubMed] [Google Scholar]
- Current management of thoracic outlet syndrome. Curr Treat Options Cardiovasc Med. 2009;11:176-83.
- [CrossRef] [PubMed] [Google Scholar]
- The epidemiological, morphological, and clinical aspects of the cervical ribs in humans. Biomed Res Int. 2016;2016:8034613.
- [CrossRef] [PubMed] [Google Scholar]
- An unusual case of the syndrome of cervical rib with subclavian artery thrombosis and cerebellar and cerebral infarctions. BMC Neurol. 2012;12:48.
- [CrossRef] [PubMed] [Google Scholar]
- The syndrome of cervical rib with subclavian arterial thrombosis and hemiplegia due to cerebral embolism-report of a case. N Engl J Med. 1942;226:942-4.
- [CrossRef] [Google Scholar]
- Acute basilar artery occlusion in a patient with left subclavian artery occlusion due to first rib anomaly: Case report. Neurol Med Chir (Tokyo). 2008;48:355-8.
- [CrossRef] [PubMed] [Google Scholar]





