Translate this page into:
Absence status seen in an adult patient
Address for correspondence: Dr. Hasan H. Ozdemir, Bismil State Hospital Neurology, Diyarbakır, Turkey. E-mail: drhasanh@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Absence status epilepticus (ASE) is a type of nonconvulsive status epilepticus in which continuous or recurrent generalized epileptiform discharges are associated with a varying grade of consciousness impairment. Absence status epilepticus may be obtained during progress of many epileptic syndromes, in several metabolic disturbances and related to use of several drugs. Absence status epilepticus is generally seen in childhood; rarely it can be seen in adulthood. In this paper, the case which has never diagnosed until now in spite of many absence seizures for years, applied for absence seizures to our clinic and diagnosed for juvenile absence epilepsy, has been discussed.
Keywords
Absence status
juvenile absence epilepsy
valproic acid
Introduction
Epileptic seizures may manifest themselves in a variety of clinical forms. Absence seizures occur as temporary loss of consciousness without any marked convulsion. Absence status is not synonymous with nonconvulsive status epilepticus, which also encompasses complex partial status epilepticus. Petit mal status and various other synonyms have also been used in the past.[1] Absence status, on the other hand, is a clinical condition where many etiological factors observed mainly in the childhood are blamed. It is extremely rare in adult patients.
Juvenile Absence Epilepsy (JAE) is one of the diseases causing absence seizures. It is commonly seen in childhood and generally accompanied by generalized tonic clonic seizures (GTC) and myoclonic jerks. JAE may last for years and usually responds well to treatment. However, absence status may rarely occur in the course of the disease. The present article discusses a case who had not been diagnosed with epilepsy before and who did not have any type of seizures except for absence seizures in the light of literature.
Case Report
A 43-year-old woman was referred to our clinic by the psychiatrist for indifference to her surroundings and failure to answer the questions posed to her for the last two days. She was reported mild impairment of consciousness manifests as slow reaction, behavior, and mental functioning. These impairment of consciousness periods occur about 10 times an hour, each lasting for 10-20 seconds. A detailed examination of the patient's history showed that her complaints started when she was 10 years old and occurred 2-3 times a week for 10 seconds each. During these periods of absentmindedness, the patient stared at a certain point, did not answer any questions, and after a period of 10-15 seconds, she resumed whatever she was doing before the seizure. Her coordination was impaired and she was uncooperative. The patient was admitted to hospital.
Hematological estimations and serum biochemical analyses were normal. Cranial MRI was evaluated as normal. Her EEG revealed 3-Hz diffuse spike-and-slow wave activity [Figure 1]. The patient was evaluated as absence status epilepticus and administered valproic acid (20 mg/kg/IV loading followed by 2 mg/kg/IV infusion for 24 hours on end). Her seizures stopped after 8 hours. The EEG taken 1 day later was evaluated as normal [Figure 2]. The EEG taken 1 day later was evaluated as normal [Figure 2]. It was found out that the patient did not suffer from any GTC or myoclonic seizures in her history and did not receive any medical treatment. She was diagnosed juvenile absence epilepsy and put on 1000 mg/day oral valproic acid treatment. The patient was found seizure-free in the clinical follow-up. Follow-up EEGs were also evaluated as normal.
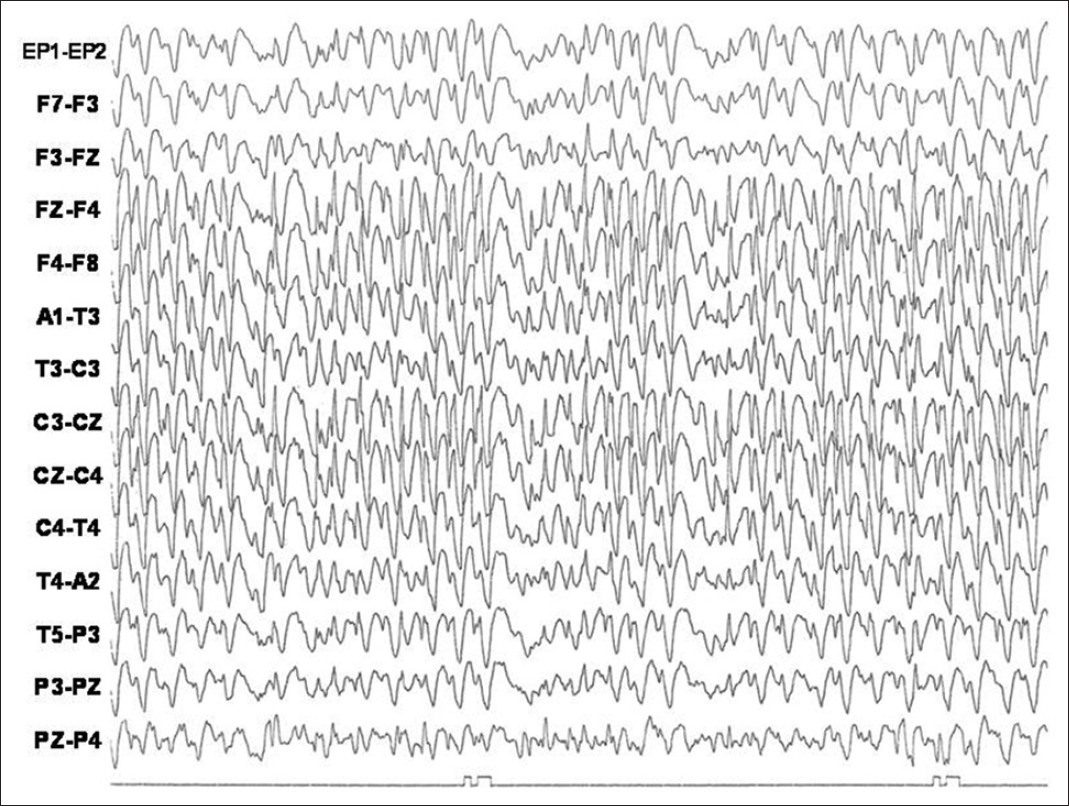
- 3-Hz diffuse spike-and-slow wave activity
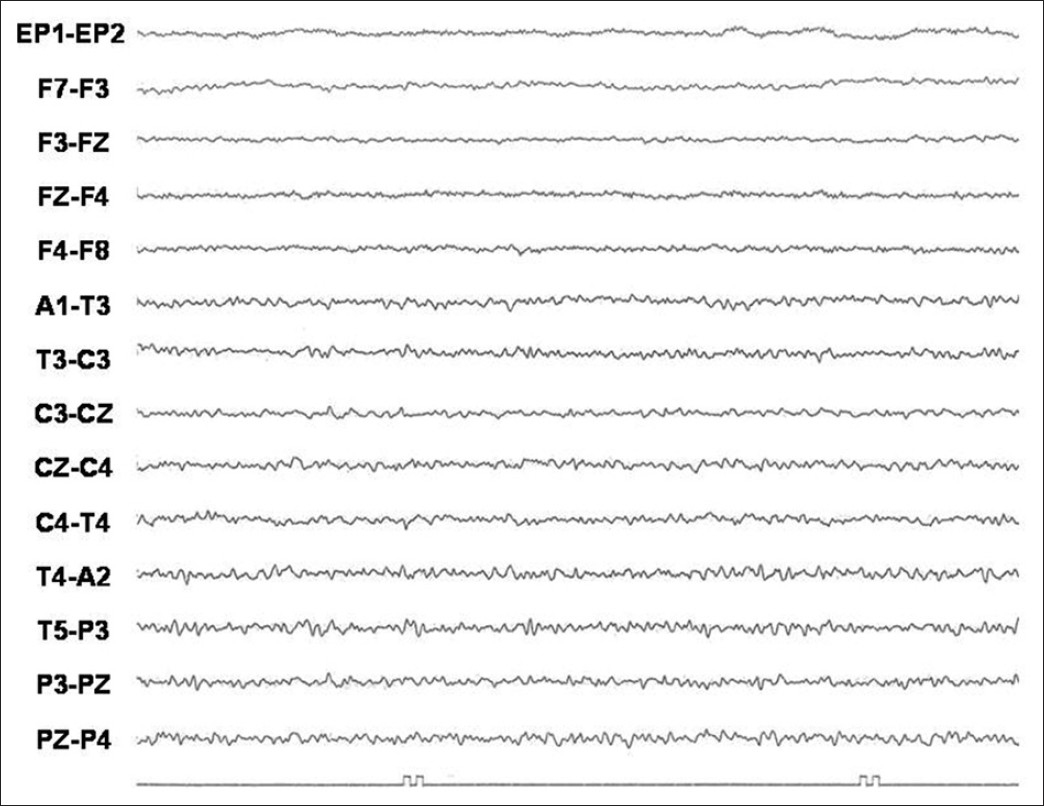
- Normal EEG
Discussion
Absence seizures are more commonly seizures of the childhood classified among idiopathic generalized epilepsies.[1] Marked clinical characteristics of absence seizures are openly correlated with EEG activity. A typical absence seizure has an abrupt onset, lasts for 10-30 seconds and involves sudden loss of consciousness, sometimes together with minor motor signs such as blinking and lip-pursing. The seizures do not have any aura and no postictal symptoms after them. The spike-and-wave EEG pattern affects all cerebral areas simultaneously with normal background activity before and after. There may be a very short 3 Hz bilaterally synchronous symmetric spike – slow wave activity without any evident clinical symptom in childhood absence seizures.[2]
Nonconvulsive status is a condition which is accompanied by a change in mental status, abnormal behavior, impairment of the ability of comprehension and loss of conscience. In the nonconvulsive status, the seizure activity lasting for more than 30 minutes or is recurrent can be shown on the EEG.[3] The diseases in which a nonconvulsive status may manifest itself include idiopathic generalized epilepsy, hypoxic-anoxic encephalopathy, cancer, drugs (psychotropic, antidepressant drugs), autoimmune diseases, Creutzfeldt–Jacob disease, peritoneal dialysis, some infections, cerebral trauma, and cerebral hamartoma.[34]
Absence status is considered in the context of nonconvulsive status. The cardinal symptom of ASE is the altered content of consciousness. Therefore, absence SE is often misdiagnosed as focal status epilepticus, confusional nonepileptic condition, or epileptic prodrome. Most of patients with ASE suffer from idiopathic generalized epilepsy, but ASE may also appear de novo. The etiology of “de novo” (late onset) ASE starting in adulthood in particular should be investigated. It may occur in the course of several epileptic syndromes, in metabolic impairments and as a result of the use of some drugs. On the other hand, ASE often occurs because of ill-advised antiepileptic drug treatment such as carbamazepine, oxcarbazepine, tiagabine, vigabatrin, gabapentin, pregabalin.[1] Thomas et al. found in their case series with late-onset absence status that sudden interruption of benzodiazepines was the most common cause of the absence status. They reported that other causes included use of psychotropic drugs, hypocalcemia, hyponatremia, and chronic alcoholism.[5] Due to the difficulty in diagnosing the status, emergent EEG monitorization may be necessary. The EEG patterns of the status include generalized slow spike-wave or multiple spike-wave paroxysms. Benzodiazepines, valproic acid or combined therapies are recommended in the treatment of ASE.[6]
Juvenile absence epilepsies (JAE) constitute the 10.2% of idiopathic generalized epilepsies and 13.3% of absence cases.[7] The age of onset is between 7 and 16 years, and the disease peaks at 10-12 years of age. It is equally common in both sexes. The seizures may recur 1-10 times a day and generally last for 4-30 seconds. Of the JAE patients, 80% experience GTC seizures and 15-25% suffer from myoclonic jerks. GTC seizures mainly occur after waking up. They are common after alcohol consumption and exhaustion. Myoclonic jerks are usually mild and irregularly scattered throughout the day. Valproate is the treatment of first choice in the treatment of JAE accompanied by GTC seizures. It contains all seizures in 70-80% of the patients. If the patient does not properly respond to treatment with valproate, then addition of lamotrigine or ethosuccimide (particularly when absence seizures are resistant) is recommended. The treatment should continue for a lifetime. Discontinuation of the drugs may lead to a reappearance of seizures in cases whose seizures have been contained for years. Additionally, hyperventilation may induce generalized bursts of spikes in such patients even after the treatment for JAE. In our case follow-up EEGs with activation procedures (especially hyperventilation) never induced abnormal responses after onset of VPA treatment, as reported in some cases.[7]
The etiological investigations in our case suggested JAE as the cause of the absence status. The status was treated with valproic acid and no side effects were observed. The present case report discussed ASE in the light of literature. Etiological factors that may cause absence status in adulthood should be extensively examined and idiopathic generalized epilepsies which have not been diagnosed should be taken into consideration.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Treatment of typical absence seizures and related epileptic syndromes. Paediatr Drugs. 2001;3:379-403.
- [Google Scholar]
- Typical absence status epilepticus as late presentation of idiopathic generalised epilepsy in an elderly patient. Seizure. 2009;18:82-3.
- [Google Scholar]
- ‘de novo’ absence status of late onset: report of 11 cases. Neurolog. 1992;42:104-10.
- [Google Scholar]
- Absence status epilepsy: Delineation of adistinct idiopathic generalized epilepsy syndrome. Epilepsia. 2008;49:642-9.
- [Google Scholar]






