Translate this page into:
Bilateral cystic glioblastoma multiforme
Address for correspondence: Dr. Amit Handa, Department of Neurosurgery, St. Stephen's Hospital, Tis Hazari, Delhi - 110 054, India. E-mail: dramithanda@yahoo.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Cystic glioblastoma multiforme (GBM) is a rare disease whose exact prevalence is unknown. Glioblastoma is usually seen as a unilateral solid tumor more commonly in the supratentorial compartment. The presence of cyst in the GBM is rare. Bilateral large cystic GBM is still rarer and we report such a case. An 83-year-old female was admitted with right hemiparesis and inability to speak for the last 4 days. There was no history of headache or seizures. On examination, there was increased tone on the right side with hemiparesis and aphasia. Magnetic resonance imaging revealed large enhancing cystic lesions measuring 4 × 2.8 × 3 cm and 4.5 × 4 × 3.5 cm in the right and left frontal regions respectively with surrounding edema [Figure 1]. Radiological possibilities suggested were glioma with differential diagnosis of abscess and metastasis. Burr-hole aspiration revealed hemorrhagic fluid and biopsy of the cyst wall confirmed the diagnosis of GBM. Attendants were explained the prognosis and did not give consent for definitive surgery. Patient died within 5 months of discharge from the hospital.
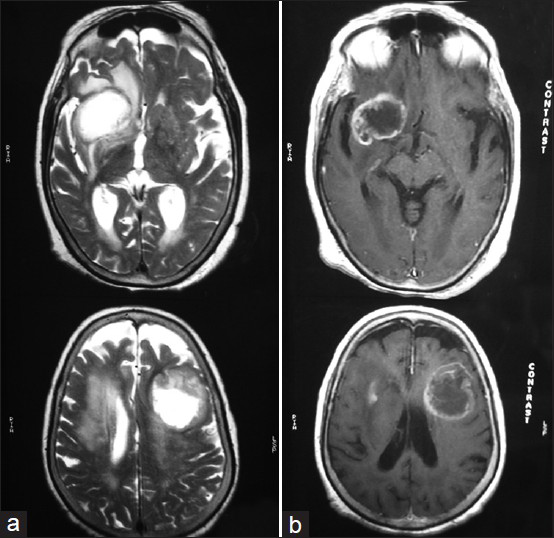
- (a) Axial T-2 weighted magnetic resonance image showing cystic glioblastoma multiforme in both frontal regions and (b) axial contrast enhanced T-1 weighted magnetic resonance image showing ring enhancing bifrontal lesions
GBM is the most malignant form of astrocytoma and associated with a poor prognosis. Cysts are commonly found in low-grade astrocytoma especially pilocytic astrocytoma. Cyst also develops in high grade tumors, but the presence of large cysts in GBM is extremely rare.[1] Cystic GBM may be primary or secondary. Secondary cystic GBM are due to malignant transformation in primary undiagnosed cystic low-grade gliomas and usually occur in younger patients whereas primary cystic GBM occur de novo. Other hypothesis put forward regarding cyst formation are necrotic degeneration of the tumor tissue, central hemorrhage and subsequent liquefaction, entrapment of adjacent cerebrospinal fluid space and blood brain disruption.[2]
A GBM is said to be multifocal when there are multiple lesions and there is an established route of spread or dissemination between these lesions and multicentric if there is no established route of spread between the two lesions.[34] Our patient belongs to the multicentric category.
GBM have a relatively narrow pericystic rim of the glioma with limited infiltration of the surrounding neuropils indicating that cystic GBM may be less infiltrative than non-cystic ones. This fact may be responsible for longer survival and lower recurrence, which could not be corroborated in our patient as she was not subjected to definitive surgery. Maldaun et al. reported median survival time after surgery to be 18.7 months in patients with cystic GBM, whereas it was 14.3 months in patients with non-cystic GBM, but the difference in overall survival was not statistically significant.[5]
The management of GBM remains controversial. The lesion should be surgically removed whenever possible and some authors recommend early aggressive surgical removal of easily accessible tumors with a mass effect. Hassaneen et al. advocated multiple craniotomies in the same sitting for multiple GBM without any added mortality or morbidity.[6] Review of literature suggests that most patients die approximately 6-8 months after the onset of symptoms, although in some studies the outcome was worse ranging from 2.8 to 4.8 months.
References
- Pathological and clinical features of cystic and noncystic glioblastomas. Brain Tumor Pathol. 2006;23:29-34.
- [Google Scholar]
- Primary and secondary glioblastomas: From concept to clinical diagnosis. Neuro Oncol. 1999;1:44-51.
- [Google Scholar]
- Pediatric multifocal glioblastoma multiforme with fulminant course. J Neurosci Rural Pract. 2012;3:174-7.
- [Google Scholar]
- Cystic glioblastoma multiforme: Survival outcomes in 22 cases. J Neurosurg. 2004;100:61-7.
- [Google Scholar]
- Multiple craniotomies in the management of multifocal and multicentric glioblastoma. Clinical article. J Neurosurg. 2011;114:576-84.
- [Google Scholar]





