Translate this page into:
Herpes zoster ophthalmicus associated with abducens palsy
Address for correspondence: Dr. Nibrass Chaker, Boulevard 9 avril 1006, Bab Saadoun Tunis, Tunisia. E-mail: chaker_nibrass@yahoo.fr
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The extraocular muscle palsies associated with herpes zoster ophthalmicus (HZO) are transient, self-limiting conditions, usually seen in elderly patients. There are different treatment recommendations for paralytic complications, but prognosis has generally reported to be favorable. A 75-year-old male patient presented with diplopia. Clinical history revealed left facial vesicular eruptions and pain treated by oral aciclovir 1 week following symptom onset. On examination, we observed cicatricial lesions with crusts involving left hemiface, a limitation in abduction of the left eye, and a superficial punctuate keratitis (SPK) with decreased visual acuity (4/10). Examination of the right eye was unremarkable. Hess screen test confirmed left six nerve palsy.
Keywords
Abducens nerve
external ophthalmoplegia
Herpes zoster ophthalmicus
Introduction
Herpes zoster ophthalmicus (HZO) is a disease in which varicella-zoster virus (VZV) replicates and produces neural inflammation and epidermal facial lesions in areas supplied by sensory branches of the ophthalmic division of the trigeminal nerve. HZO can also cause a variety of ocular manifestations. Extraocular muscle palsies are rare complications occurring in seven to 31% of HZO, usually seen in elderly patients and characterized by self-limited resolution.[1] We present herein a case of HZO complicated by sixth nerve palsy and we discuss the etiology of this complication.
Case Report
A 75-year-old man without significant medical history presented with diplopia. Clinical history revealed left facial vesicular eruptions and pain. Treatment commenced with oral acyclovir (2 g daily) 1 week following symptom onset. On physical examination, cicatricial lesions were observed with crusts involving the left hemiface, and limited left eye abduction [Figure 1]. Visual acuity was 4/10 with conjunctival hyperemia, superior superficial punctuate keratitis (SPK), and normal intraocular pressure (IOP). Pupil size was 5 mm, with prompt pupillary light reflex, a posterior intraocular lens, and a normal fundus of the left eye. In the right eye, corrected visual acuity along with unremarkable examination of the anterior and posterior segments.

- Cicatricial lesions on the left hemiface and limited abduction
The Hess chart demonstrated that abduction of the left eye was severely limited [Figure 2]. A brain magnetic resonance imaging (MRI) ruled out possible brain lesions.
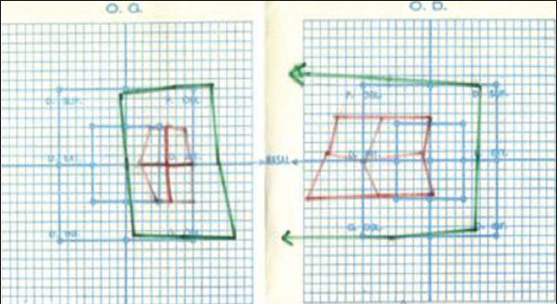
- Severely limited abduction on the Hess chart
Vesicular eruptions resolved within 1 week, although diplopia was still present. Six weeks later, abducens nerve palsy had improved without additional treatment [Figures 3 and 4].

- Clinical improvement of the abducens nerve palsy
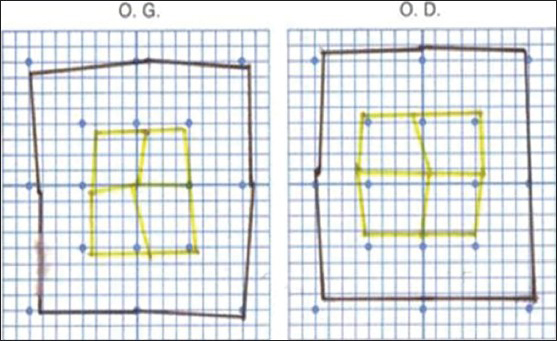
- Improvement of the abducens nerve palsy on the Hess chart
Discussion
Herpes zoster (HZ) is a common disease mainly affecting elderly patients due to reduction in the level of T-cell immunity to VZV following initial infection and senescence.[2] HZ occurs by reactivation of latent virus in ganglions following primary infection with varicella zoster (chicken pox) and occurs mostly in thoracic and cranial sensory ganglia.[34] HZ is a localized disease characterized by unilateral radicular pain and a vesicular eruption. In addition to sensory neurons, HZ may also affect motor neurons in rare cases.[1]
When the ophthalmic division of the trigeminal nerve is affected, the condition is referred to as HZO which occurs in 10-25% of HZ[5] with 50% of these cases infecting the eye.[34]
Ocular signs can be acute, chronic, and relapsing; and include conjunctivitis, keratitis (commonly epithelial followed by nummular and disciform), episcleritis, scleritis, uveitis, secondary glaucoma, cataract, and retinal necrosis.[345] Mucus plaque keratitis and mucus-secreting conjunctivitis can also occur in chronic cases.[6] HZO may cause extraocular muscle palsies of the third, fourth, and sixth cranial nerves in 7-31% of patients.[1] The third nerve is the most common site among them and the fourth the least.[1478] Complete ophthalmoplegia is a very rare complication of HZO; only few cases have been reported in the literature.[910]
The extraocular muscle palsies usually appear 2-4 weeks after the rash, but sometimes occurs simultaneously with the rash or more than 4 weeks later.[1] Our patient presented with a sixth nerve palsy 1 week after the vesicular rash.
The pathogenesis of ophthalmoplegia is controversial and several mechanisms have been postulated: The first is a direct cytopathic effect from the virus itself on the surrounding neural tissue. The second is an immune response of the central nervous system to the virus. The third attributes it to an occlusive vasculitis induced by the virus. A fourth theory suggests that the VZV activates another latent neuropathic virus within the brain.[3]
Kreibig et al., postulated that the extraocular palsies were due to perivasculitis-myositis, rather than to a neural origin.[1] Muscle ischemia remains a strong possibility, as does a combination of cortical nerve and muscle inflammation.[1] Therefore, isolated abducens nerve palsy might be caused by circumscribed orbital myositis or a lymphocytic cranial motor neuropathy.[1]
The therapeutic goal is to limit the severity of acute and chronic pain, hasten the healing process, and reduce the chances of dissemination.[4]
Treatment consists of administration of an antiviral agent that crosses the blood-brain barrier (acyclovir, famciclovir, valacyclovir).[3]
Antiviral therapy is substantially more effective if begun within the first 72 h of rash onset.[2] Antiviral treatment induces prompt resolution of skin lesions, diminishes viral shedding, lessens lesion formation, and decreases corneal and uveal involvement. Treatment with nucleotide analogues may prevent the direct cytotoxic effect of the virus, the immune response of the surrounding neural tissue, and the initiation of a secondary vasculitis by inhibiting initial viral replication limiting duration and severity of infection.[2] The use of systemic corticosteroids may be effective to prevent occlusive vasculitis, but there is a risk of suppressing the immune system in viral infections with corticosteroid use.[3]
There are different suggestions about treatment of paralytic lesions that complicate HZ. Some authors have examined the effectiveness of antiviral therapy and adrenal cortex hormones.[11] As the paralytic lesions tend to resolve spontaneously, effects of specific treatment are unclear.[11]
A live attenuated HZ vaccine for individuals older than 60 years has recently been proposed. The efficacy of the vaccine in preventing HZ is 70% for subjects 50-59 years of age, 64% for persons 60-69 years of age, 41% in subjects aged 70-79 years, and 18% in individuals aged > 80 years.[212] However, there is a risk of developing HZ in patients who receive the vaccine who have never been infected with VZV.
The prognosis of ophthalmoplegia is generally favorable. It was reported that duration of diplopia associated with ocular motor palsy was between 2 and 23 months. However, 87.5% of diplopia cases recovered within 1 year.[3]
Conclusion
Ophthalmoplegia as a complication of HZO may have various origins; the efficacy of antiviral agents and corticosteroids in treating the oculomotor palsy remains controversial since the spontaneous recovery of palsy has been reported.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- A case of complete ophthalmoplegia in herpes zoster ophthalmicus. Korean J Ophthalmol. 2005;19:302-4.
- [Google Scholar]
- Complete ophthalmoplegia with pupillary involvement as an initial clinical presentation of herpes zoster ophthalmicus. J Am Osteopath Assoc. 2008;108:615-21.
- [Google Scholar]
- A case of herpes zoster ophthalmicus associated with multiple ocular and extraocular manifestations. Neuro-Ophthalmology. 2008;32:75-9.
- [Google Scholar]
- Clinical Ophtalmology. A systemic approach. (5th ed). London: Butterworth-Heinemann; 2003. p. :111-4.
- [Google Scholar]
- External ocular motor palsies in ophthalmic zoster: A review. Br J Ophtalmol. 1977;61:677-82.
- [Google Scholar]
- Herpes zoster ophthalmicus as a cause of Horner syndrome. J Clin Neuroophthalmol. 1993;13:250-3.
- [Google Scholar]
- Complete unilateral ophthalmoplegia in herpes zoster ophthalmicus. J Neuroophthalmol. 2009;29:325-37.
- [Google Scholar]
- Herpes zoster guideline of German Dermatology Society. J Clin Virol. 2003;26:277-89.
- [Google Scholar]






