Translate this page into:
Clinical profile and outcome of cerebral venous sinus thrombosis at tertiary care center
Address for correspondence: Dr. Virendra C. Patil, Department of Medicine, Krishna Institute of Medical Sciences University Karad, Satara - 415 110, Maharashtra, India. E-mail: virendracpkimsu@rediffmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Thrombosis of the cerebral venous sinuses (CVST) is an uncommon form of stroke, usually affecting young individuals. Clinical features of CVST are diverse, and for this reason, high degree of clinical suspect is mandatory to diagnose the conditions.
Materials and Methods:
This study was conducted over a period of 1 year (Jan 2011 to Dec 2011). This was a retrospective, observational, and noninterventional study. This study was conducted in the Department of Medicine at a tertiary care teaching center. Total 50 patients where diagnosis of CVST was confirmed by computed tomography/magnetic resonance imaging brain venogram were included in this study. All patients with diagnosis of CVST were treated according to the standard protocol and guidelines.
Statistical Analysis:
The mean and standard deviation were obtained. The Chi-square test was used to analyze the data and P < 0.05 was considered as statistically significant.
Results:
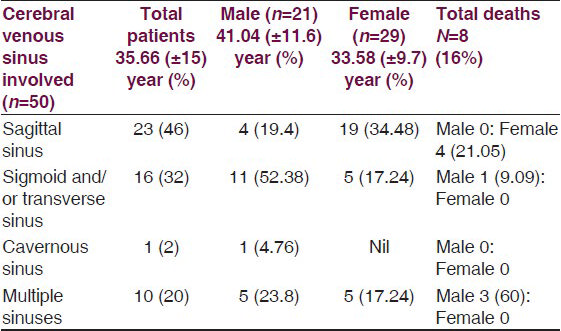
Of total 50 patients with diagnosis of CVST, 21 (42%) were males and 29 (58%) were females with 39 ± 10 years and 29 ± 7 years, respectively. Total 45 (90%) patients presented with symptoms of headache and vomiting, 13 (26%) had seizures, 12 (24%) had hemiplegia, and 19 (38%) had fever. A total of 13 (26%) patients had papilledema on fundoscopy. Total 9 (31%) out of 29 patients had diagnosis of CVST during peripartum period. Total 12 (24%) patients had hyperhomocysteinemia. Total 23 (46%) patients had sagittal sinus thrombosis, 10 (20%) had multiple sinus thrombosis, 16 (32%) had sigmoid/transverse sinus thrombosis. There was 1 (2%) patient who had bilateral cavernous sinus thrombosis, who presented with bilateral proptosis, conjunctival congestion, and external ophthalmoplegia with a history of acute or chronic maxillary and sphenoid sinusitis. Total 38 patients had evidence of infection in the form of fever, paranasal sinus (PNS) infections, Chronic suppurative otitis media (CSOM). Total 19 (38%) patients had a history and evidence of dehydration. Total 8 (16%) patients died during the course of treatment and 42 (84%) were discharged with partial and/or total recovery. Three (6%) patients required neurosurgical intervention in the form of decompressive craniotomy. Eight (16%) patients died with cerebral edema with transtentorial herniation. The mean age of death in male was significantly greater than in female patients with P < 0.02. Majority of patients succumbed had sigmoid, transverse, and/or multiple sinus involvement. Patients with multiple sinus thrombosis had greater case fatality rate.
Conclusions:
The current study highlights the burden of CVST in the study population with headache and vomiting, which was the most common presenting complaint. The superior sagittal sinus thrombosis was the most common and bilateral cavernous sinus thrombosis was the uncommon affection in CVST. One third of female population was affected in peripartum period. The infection and/or dehydration was the most commonly associated precipitating event for development of CVST and more than one fifth of the population had evidence of hyperhomocysteinemia. Mortality was more in patients with affection of sigmoid, transverse, and/or multiple sinus involvement in male patients and superior sagittal sinus thrombosis in female patients. The treatment of CVST has to be aggressive as morbidity and mortality is relatively minimal compared with the arterial stroke.
Keywords
Hyperhomocysteinemia
peripartum
sagittal sinus thrombosis
thrombosis of the cerebral venous sinuses
Introduction
Cerebral venous sinus thrombosis (CVST) is one of the common causes of stroke in young people. CVST is a disease with potentially serious consequences and usually affecting young to middle-aged people. Strokes in the young account for nearly 30% of all cases of stroke in India and cerebral venous thrombosis (CVT) accounts for 10-20% of these cases. Two-thirds of them develop the same in the postpartum period. There has been a drastic reduction of infection as a causative agent for CVST in recent years. Primary or idiopathic CVST are mainly caused by hypercoagulable state commonly from puerperium or from dehydration. Puerperal CVST may account for approximately 15%-20% of stroke victims of younger age. CVST can be caused by a number of prothrombotic states and disorders of clotting system such as inherited cause is Protein C resistance secondary to Factor V Leiden polymorphism, Protein C and S resistance, and antithrombin III deficiency. Other vasculitis such as Systemic lupus erythematosus (SLE) and polyarteritis nodosa (PAN) are also relevant in young adults. Dehydration is still most common cause puerperal CVST in our country. The purpose of this study was to analyze the characteristics of CVT in a rural hospital. CVST is an uncommon form of stroke, usually affecting young individuals. CVST represents 0.5%-1% of all strokes. Multiple factors have been associated with CVST, but only some of them are reversible.[12] No population studies have reported the incidence of CVST. Hyperhomocysteinemia is a risk factor for deep vein thrombosis (DVT) and stroke but has not been clearly associated with an increased risk of CVST. The objectives were to study the clinical profile of the patients with CVST and to assess the risk factors involved.
Materials and Methods
This study was conducted over a period of 1 year (Jan 2011 to Dec 2011). This was a retrospective, observational, and noninterventional study. This study was conducted in the Department of Medicine at a tertiary care teaching center. The study was approved by the ethical committee of KIMS, Karad. All the patients included in the current study have documented CVST on magnetic resonance imaging (MRI) venogram. The information of all the patients fulfilling the criteria of CVST of both genders was entered in a data entry sheet. All the patients were treated in the intensive care unit under standard guidelines and protocols. Patients with diagnosis of CVST were treated in intensive care unit. Patients with diagnosis of CVST were treated with intravenous fluids to correct dehydration, decongestive agents, anticonvulsant drugs, antibiotics, low–molecular weight heparin (LMWH) (if not contraindicated), decompressive craniotomy, methylcobalamin and folic acid supplementations, and so on. All 50 patients in whom the diagnosis of CVST was confirmed by computed tomography/MRI brain venogram were included in this study. All patients underwent basic investigations, such as hemogram, electrolytes, blood sugar levels, renal function tests, and chest radiographs. Liver function tests, coagulation studies, inflammatory markers, and homocysteine levels were done in selected patients because of financial constraints. Cerebral venous system was classified into two major groups: (1) Sagittal sinuses and cortical veins draining superficial surfaces of both cerebral hemispheres. (2) Deep system comprises lateral sinus, straight sinus, and sigmoid sinus along with draining deeper cortical veins. We excluded the trauma as a factor for development of CVST from history.
Statistical analysis
SPSS software version 11 was used to analyze the data.[134] The mean, standard deviation, and Chi-square test was used to analyze the data and P < 0.05 was considered as statistically significant.
Result
A total of 50 patients were included in this retrospective observational study with age more than 15 years and with diagnosis of CVST. Of the total 50 patients with CVST, 21 (42%) were males and 29 (58%) were females with 39 ± 10 years and 29 ± 7 years, respectively.
Clinical presentation
Forty-five (90%) patients presented with symptoms of headache and vomiting, 13 (26%) had seizures, 12 (24%) had hemiplegia, and 19 (38%) had fever. A total of 13 (26%) patients had papilledema on fundoscopy. Headache and vomiting were the most common presenting features in patients with CVST (P < 0.002) and next was hemiplegia and seizures [relative risk (RR): 2.36; odds ratio (OR): 14.68] [Table 1].

Causative factor for CVST
Nine (31%) out of 29 patients had diagnosis of CVST during peripartum period (RR: 1.29; OR: 1.42). Nineteen (38%) patients underwent test for serum homocysteine level. Total 12 (24%) patients had hyperhomocysteinemia of whom 8 (27.58%) were females and 4 (19.04%) were male patients (RR: 1.44; OR: 1.61). Total 39 patients had evidence of infection in the form of fever, paranasal sinus (PNS) infections, and/or chronic suppurative otitis media (CSOM). Total 19 (38%) patients had a history and evidence of dehydration due to fluid loss, poor intake due to some or other reasons [Table 2 and Graph 1].


- Risk factors for the development of cerebral venous sinus thrombosis
Type of sinus involved in CVST
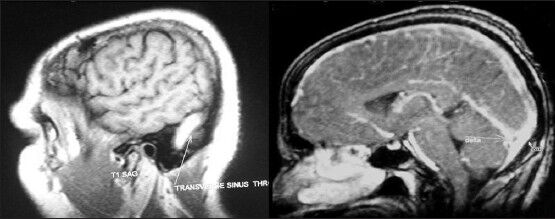
Total 23 (46%) patients had sagittal sinus thrombosis (RR: 1.49; OR: 1.91), 10 (20%) had multiple sinus thrombosis, and 16 (32%) had sigmoid/transverse sinus thrombosis. There was 1 (2%) patient who had bilateral cavernous sinus thrombosis, who presented with bilateral proptosis, conjunctival congestion, and external ophthalmoplegia with a history of acute or chronic maxillary and sphenoid sinusitis. The mean duration of stay of patients admitted with CVST was 8 ± 3 days [Tables 3 and 4; Figures 1 and 2].
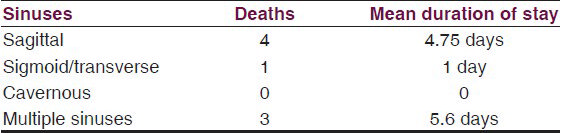
- Magnetic resonance imaging brain venogram showing transverse sinus thrombosis and superior sagittal sinus thrombosis evidenced by empty delta sign
- Magnetic resonance imaging brain venogram showing superior sagittal sinus thrombosis and hemorrhagic conversion of venous infarct and computed tomography brain showing superior sagittal sinus thrombosis evidenced by empty delta sign
Outcome of patients with CVST
Forty-two (84%) patients were discharged with partial and/or total recovery from illness in the form of hemiplegia or monoplegia. Of the 3 (6%) patients who underwent decompressive surgery, 2 patients improved and 1 succumbed. Eight (16%) patients died with cerebral edema with transtentorial herniation. Case fatality rate was more with sagittal sinus thrombosis [females n = 19 (34.48%); death = 4 (21.05%)] in female and multiple sinus [male n = 5 (23.8%); death 3 (60%)] (RR: 0.709; OR: 0.622) involvement in male patients. Total 4 (19.04%) male patients (58.5 ± 9 yrs) and 4 (13.79%) female (39.25 ± 11.5yrs) patients succumbed. Mean age of death in male was significantly greater than in female patients with P < 0.02. Mortality rate was relatively more in male patients. A total of 3 (6%) patients required neurosurgical intervention in the form of decompressive craniotomy. Majority of patients who succumbed had sigmoid, transverse, and/or multiple sinus involvement. Patient with multiple sinus thrombosis had greater case fatality rate followed by patients with sagittal sinus thrombosis (RR: 0.57; OR: 0.4912). [Table 5 and Graph 2].
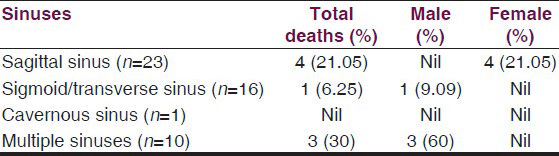

- Type of cerebral venous sinus thrombosis and mortality
Discussion
CVST is reported to be more common in developing countries, and has been linked to pregnancy, multiparity, dehydration, and infection. Developments in imaging, diagnostic laboratory investigations, and genetics have provided valuable information about risk factors and clinical spectrum of CVST. We compared our experience of CVST, highlighting its diverse clinical presentations, predisposing factors, and neuroimaging with other studies from India and abroad. CVST represents 0.5%-1% of all strokes. According to the largest cohort study, 78% cases occurred in patients younger than 50 years. One pathological study found a prevalence of CVT of 9.3% among 182 consecutive autopsies. No population studies have reported the incidence of CVT. Hyperhomocysteinemia is a risk factor for DVT and stroke but has not been clearly associated with an increased risk of CVT.[1] Twenty-four percent of our population had hyperhomocysteinemia and more predominantly in female population. Lath et al.[5] stated that the mortality in CVST, in addition to progressive thrombosis, is related to elevated intracranial pressure causing transtentorial herniation. They reported a mortality of 27%. These findings are comparable with our result with a low mortality of 16%. Lath et al. reported that the decompressive surgery for patients with large cerebral venous infarcts is a life-saving procedure. Similarly, in our study, 3 (6%) patients underwent decompressive surgery of whom 2 patients improved and 1 succumbed. Pfefferkorn et al.[4] studied 32 patients with CVST with headache (81%) being common presenting symptom. Out of 32 patients, 9 (28%) had deep cerebral venous system thrombosis (DCVST) and 23 (72%) had non-isolated DCVST. Similarly, in our study 45 (90%) patients presented with symptoms of headache and vomiting with deep venous system thrombosis in 16 (32%) (sigmoid and/or transverse sinus) and 23 (46%) patients had superficial system (superior sagittal sinus) thrombosis. Azin et al.[6] studied 61 patients with CVST where male-to-female ratio was 1/3.1. The mean age of patients was 35.6 ± 12.1 years. Headache was seen in 91.8% of the patients. The most frequent risk factor was oral contraceptive consumption (62.2%). Involvement of superior sagittal sinus and lateral sinus was 80.3% and 41%, respectively. The fatality rate was 14.7%. Similarly, headache in 45 (90%) patients was the most common presenting feature in our study. Infection dehydration hyperhomocystemia and peripartum state were the important precipitating or risk factors, either individually or in combination for development of CVST in our study with mortality of 16%. In our study, 23 (46%) (RR: 1.49; OR: 1.91) patients had sagittal sinus, 16 (32%) had sigmoid and/or transverse sinus, and 10 (20%) had multiple sinuses involvement. Prakash et al.[2] reported that the most common involvement in CVST was superior sagittal sinus (72%), similarly in our study 46% patients had superior sagittal sinus thrombosis. Khealani et al.[7] stated that the obstetric CSVT has a different course and carries favorable prognosis as compared with CVT unrelated to pregnancy. There is evidence that mortality can be altered favorably by anticoagulation. Favorable outcome has been reported from 60% to 76% of cases. Favorable outcome in obstetric CVT has been attributed to the assumption that the occlusion is limited and transient with rapid recanalization or by development of collaterals. Similarly, in our study all 9 female patients in peripartum period were recovered with no mortality. Nagaraja et al.[8] reported that strokes in the young account for nearly 30% of all cases of stroke in India and CVT accounts for 10%-20% of these cases. Two-thirds of them develop the same in the postpartum period. Similarly, in our study about one third of female population had CVST in peripartum period. Nagarajan et al.[9] studied total 25 patients with CVST with mean age 35.7 years with a male-to-female ratio of 13:12. Headache (84%) and convulsions (47%) were the most common clinical features. Focal neurological deficits were observed in 60% of the patients and hemiparesis was the common deficit (28%). Infection was present in 28% cases. Superior sagittal sinus was the most frequent sinus involved. Similarly, in our study of the 50 patients with CVST, 21 (42%) were males and 29 (58%) were females with 39 ± 10 years and 29 ± 7 years, respectively, and 90% patients presented with symptoms of headache and vomiting with 24% having hemiplegia. Total 23 (46%) of the patients had superior sagittal sinus thrombosis, 39 (78%) patients had evidence of infection, and 38 (76%) patients had dehydration. Similar findings were reported by Appenzeller et al.[10] in their study of 24 patients (18 women, 6 men) with mean age of 29.5 years with headache (75%) and vomiting (33%); pregnancy or puerperium in six (25%), and inherited thrombotic risk factors in four (17%) patients. Pai et al.[11] studied 612 (354 men, 219 women, and 39 children) patients with CVT with papilledema (62%), headache (62%), hemiparesis (48%), seizures (31%), and cranial nerve palsy (7%). Superior sagittal sinus thrombosis was the most common site (74%) associated with dehydration, sepsis, pregnancy, and puerperium, Death due to CVT was 13%. These findings are comparable with our study. Haghighi et al.[12] studied 465 patients in the age group 29.5-43.8 years with ratio of female to male being 2.79. Headache (80%-97%), sensory/motor deficits (39%-64%), and seizure (20%-62%) were the most common clinical presentations with mortality rate of 11.4%. Similarly, our study had a mortality rate of 16%. Mehndiratta et al.[13] reported that headache (80%) is the most frequent symptom in patients with CVT with 75% being female population. The mean age among females was 27.75 years and among males was 41.5 years. Of the 4 females, 2 were postpartum. Of 2 males, 1 had hyperhomocysteinemia and one had hyperlipidemia. Similarly in our study approximately one fifth of the population had hyperhomocysteinemia predominantly in female population and about one third of the population had CVST in peripartum period. Nagaraja et al.[3] (2007) stated that the pregnancy and puerperium increase the risk of thrombotic events, and these risks are likely to be increased in women who are carriers of thrombophilic gene polymorphisms. Prothrombin G20210A variant is reported to be the second most frequent prothrombotic polymorphism in Whites. Kalita et al.[14] reported that the CVST more often occurs during pregnancy, multiparity, and infection. In their study of 33 patients with CVST, mean age 37.5 years (range 16-76); 23 were female with superior sagittal sinus in 23, the lateral sinus in 19, straight sinus in 3, inferior sagittal sinus in 1, and deep venous system in 1. Seventeen patients had multiple sinus involvements. Predisposing factors could be identified in 16 patients, and included pregnancy and puerperium in 6, infection in 6, oral contraceptive in 2, and dehydration in 1 each. Most CVST studies from India are of puerperal. These findings are comparable with our results. Koopman et al.[15] stated that CVST was more frequently associated with oral contraceptive use, pregnancy, or puerperium. CVT was relatively more common in women and hormonal factors may predispose to CVT. Coutinho et al.[16] in their study of 624 patients, 75% were women with significantly younger, with better outcome compared with male patients with CVST. These findings are comparable with our study in which death was relatively more in male than female (OR: 0.68; CI: 0.149: 3.099). Martinelli et al.[17] in their case–control study found that the hyperhomocysteinemia is associated with a 4-fold increased risk of CVT. These findings are comparable with our study in which 24% patients found to have hyperhomocysteinemia predominantly in female population (female-to-male ratio, 2:1). Ahmad et al.[18] stated that inherited thrombophilias with concomitant acquired risk factors such as surgery, trauma, prolonged immobilization, pregnancy and puerperium, oral contraceptives, antiphospholipid antibodies, and hyperhomocysteinemia increase the risk of CSVT. Aaron et al.[19] in their study of 41 patients reported that 34% had hyperhomocysteinemia with a 17% mortality. Similarly in our study, 24% of the population had hyperhomocysteinemia with an overall mortality rate of 16%. Shen et al.[20] reported a case of familial hyperhomocysteinemia-related CVST and pulmonary embolism in a 21-year-old man with elevated serum homocysteine level, that is, 46.23 μM/L. They concluded that the cause of CVT and pulmonary embolism in this young patient was most likely related to familial hyperhomocysteinemia, precipitated by a preceding systemic infection. Pillai et al.[21] in their study with CVST state that the most common risk factor was use of oral contraceptive pills (38.4%), peurperium (23%) and one case was of recent surgery. Eleven out of 15 patients tested for homocysteine levels had increased levels, of whom 14 were males. There were 4 deaths, out of which 2 were males. These findings are comparable with our study. Akhtar et al.[22] stated that hyperhomocysteinemia is responsible for both arterial and venous thrombosis and it should be considered as an important risk factor for atherosclerotic vascular and venous thromboembolic diseases. Nagaraja et al.[3] stated that hyperhomocysteinemia is a known risk factor for venous thrombosis. Hyperhomocysteinemia is associated with an increased risk of puerperal CVST occurring in Indian women and low folate levels contribute significantly to hyperhomocysteinemia. Nutritional folate and vitamin B12 deficiency can cause hyperhomocysteinemia and pregnancy may contribute to this deficiency. Rajput et al.[23] in their case report of CVST found that acquired hyperhomocysteinemia, presumably due to nutritional deficiencies, and was treated with LMWH, followed by warfarin, vitamin B12, vitamin B6, and folic acid, and recovered successfully. Fernández-Moreno et al.,[24] in their case report, stated that persistent high homocysteine levels was found in patients with CVST. Seventy percent of the patients with thrombosis of the cerebral venous sinuses present hypercoagulable states, including moderate hyperhomocysteinemia. These findings are comparable with our results. Cantu et al.[25] in their study of 45 patients found that there was a higher frequency of MTHFR mutation in patients with CVST (22%) with high plasma concentrations of homocysteine, and low plasma folate levels were associated with an increased risk of CVST. Similarly in our study 24% patients had hyperhomocysteinemia (23.5 ± 6.3 μmol/L). Hassan et al.[26] reported that methylcobalamin, pyridoxine, and folic acid supplementation resulted in fall in homocysteine to 16.50 μmol/L (5.46-16.2 μmol/L). The present study highlighted the clinical profile, causative/risk factors, and outcome of patients with CVST.
Conclusion
We concluded that the treatment of CVST has to be aggressive as morbidity and mortality is relatively minimal. The present study revealed significant number of patients affected by CVST in 2nd and 3rd decade of life, predominantly affecting female population, approximately one third. Most common sinus affected in male was sigmoid and transverse sinus thrombosis. Sagittal sinus was most commonly affected in female population. Affections of sigmoid, transverse, and multiple sinus thrombosis had more mortality and morbidity with longer duration of stay and residual significant neurodeficit. Headache and vomiting were the most common presenting symptoms and next was seizure. Significant proportion of individual with CVST had hyperhomocysteinemia. Acute gastro enteritis, fluid loss, and presence of infection were the precipitating factors for development of CVST. Infection and dehydration are the common precipitating factors for development of CVST in developing countries, including India. The difference in the incidence is probably due to the differences in genetic makeup of different ethnic groups and race as well. Prevention and proper management of infection and dehydration with supplementation of folic acid methylcobalamin, and pyridoxine are mandatory for prevention and management of CVST along with LMWH, anticonvulsant, and decongestive drugs. Peripartum period is vulnerable for development of CVST due to the presence of infection and dehydration. Significant number of patients had CVST in their peripartum period. The meticulous intensive care management is mandatory for better outcome in patients with CVST. Methylcobalamine, folic acid, and pyridoxine supplements to the patient with hyperhomocystenemia will be helpful in the prevention of CVST. CVT is an underdiagnosed condition for acute or slowly progressive neurological deficit. Newer imaging procedures have led to easier recognition of venous sinus thrombosis, offering the opportunity for early therapeutic measures. CVST is less frequent than arterial thrombosis.
Limitations of study
Because of resource limitations, the evaluation of genetic prothrombotic factors and uncommon hematological conditions were not possible to evaluate.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- American Heart Association Stroke Council and the Council on Epidemiology and Prevention. Diagnosis and management of cerebral venous thrombosis: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42:1158-92.
- [Google Scholar]
- The prothrombin gene G20210A variant and puerperal cerebral venous and sinus thrombosis in South Indian women. J Clin Neurosci. 2007;14:635-8.
- [Google Scholar]
- Clinical features, course and outcome in deep cerebral venous system thrombosis: An analysis of 32 cases. J Neurol. 2009;256:1839-45.
- [Google Scholar]
- Decompressive surgery for severe cerebral venous sinus thrombosis. Neurol India. 2010;58:392-7.
- [Google Scholar]
- Cerebral venous sinus thrombosis—Clinical features, predisposing and prognostic factors. Acta Neurol Taiwan. 2008;17:82-7.
- [Google Scholar]
- Characteristics of cerebral venous thrombosis in a South Indian Rural Hospital. Int J Med Health Sci. 2013;2:298-304.
- [Google Scholar]
- Cerebral venous thrombosis: Influence of risk factors and imaging findings on prognosis. Clin Neurol Neurosurg. 2005;107:371-8.
- [Google Scholar]
- Hereditary thrombophilia in cerebral venous thrombosis: A study from India. Blood Coagul Fibrinolysis. 2013;24:540-3.
- [Google Scholar]
- Cerebral venous sinus thrombosis in Iran: Cumulative data, shortcomings and future directions. Iran Red Crescent Med J. 2012;14:805-10.
- [Google Scholar]
- Cerebral venous thrombosis--clinical presentations. J Pak Med Assoc. 2006;56:513-6.
- [Google Scholar]
- Cerebral venous sinus thrombosis in a tertiary care setting in India. QJM. 2006;99:491-2.
- [Google Scholar]
- Risk factors for cerebral venous thrombosis and deep venous thrombosis in patients aged between 15 and 50 years. Thromb Haemost. 2009;102:620-2.
- [Google Scholar]
- Underlying prothrombotic states in pregnancy associated cerebral venous thrombosis. Neurol India. 2010;58:555-9.
- [Google Scholar]
- Familial hyperhomocysteinemia-related cerebral venous sinus thrombosis and pulmonary embolism: A case report. Acta Neurol Taiwan. 2007;16:98-101.
- [Google Scholar]
- Cerebral venous thrombosis: An experience with anticoagulation with low molecular weight heparin. Indian J Crit Care Med. 2005;9:14-8.
- [Google Scholar]
- Haematologic disorders and cerebral venous thrombosis. J Pak Med Assoc. 2006;56:498-501.
- [Google Scholar]
- Central venous sinus thrombosis in a young woman taking norethindrone acetate for dysfunctional uterine bleeding: Case report and review of literature. J Obstet Gynaecol Can. 2008;30:680-3.
- [Google Scholar]
- Hyperhomocysteinemia-related cerebral venous thrombosis. Rev Neurol. 2003;37:1040-3.
- [Google Scholar]
- Hyperhomocysteinemia, low folate and vitamin B12 concentrations, and methylene tetrahydrofolate reductase mutation in cerebral venous thrombosis. Stroke. 2004;35:1790-4.
- [Google Scholar]
- Reversible diencephalic dysfunction as presentation of deep cerebral venous thrombosis due to hyperhomocysteinemia and protein S deficiency: Documentation of a case. J Neurosci Rural Pract. 2013;4:193-6.
- [Google Scholar]






