Translate this page into:
Central nervous system tumors: Radiologic pathologic correlation and diagnostic approach
Address for correspondence: Dr. Ishita Pant, Department of Pathology, Institute of Human Behaviour and Allied Sciences, Dilshad Garden, Delhi - 110 095, India. E-mail: ishitapant@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective:
This study was conducted to formulate location-wise radiologic diagnostic algorithms and assess their concordance with the final histopathological diagnosis so as to evaluate their utility in a rural setting where only basic facilities are available.
Materials and Methods:
A retrospective analysis to assess the concordance of radiology (primarily MRI) with final histopathology report was done. Based on the most common incidence of tumor location and basic radiology findings, diagnostic algorithms were prepared.
Results:
For supratentorial intraaxial parenchymal location concordance was seen in all high-grade astrocytomas, low- and high-grade oligodendrogliomas, metastatic tumors, primitive neuroectodermal tumors, high-grade ependymomas, neuronal and mixed neuro-glial tumors and tumors of hematopoietic system. Lowest concordance was seen in low-grade astrocytomas. In the supratentorial intraaxial ventricular location, agreement was observed in choroid plexus tumors, ependymomas, low-grade astrocytomas and meningiomas; in the supratentorial extraaxial location, except for the lack of concordance in the only case of metastatic tumor, concordance was observed in meningeal tumors, tumors of the sellar region, tumors of cranial and paraspinal nerves; the infratentorial intraaxial parenchymal location showed agreement in low- as well as high-grade astrocytomas, metastatic tumors, high-grade ependymoma, embryonal tumors and hematopoietic tumors; in the infratentorial intraaxial ventricular location, except for the lack of concordance in one case of low-grade astrocytoma and two cases of medulloblastomas, agreement was observed in low- and high-grade ependymoma; infratentorial extraaxial tumors showed complete agreement in all tumors of cranial and paraspinal nerves, meningiomas, and hematopoietic tumors.
Conclusion:
A location-based approach to central nervous system (CNS) tumors is helpful in establishing an appropriate differential diagnosis.
Keywords
Algorithms
central nervous system tumors
pathology
radiology
Introduction
While interpreting the histopathology of central nervous system (CNS) tumors, radiological details are of particular relevance to histopathologists. Interpretation of histopathology details is greatly aided when viewed in the perspective of clinical, per-operative and radiological details. Neuroradiology, as practiced at advanced centers, has become a very sophisticated science. With the availability of MRI, perfusion imaging, diffusion-weighted imaging, MR spectroscopy, blood oxygen level-dependent (BOLD) imaging, the diagnostic yield has improved significantly. Details of neuroradiological findings in various CNS lesions are available in various sources of the medical literature. In spite of these rapid advances, diagnosis of CNS lesions remains a challenge for the neurosurgeons and pathologists in rural or primary health care settings. The only additional inputs often available are the MRI findings. The authors of this study have tried to develop simplified algorithms based on MRI findings which are mostly available. This location-wise algorithmic approach may be very helpful in the pathology reporting rooms of rural settings.
Materials and Methods
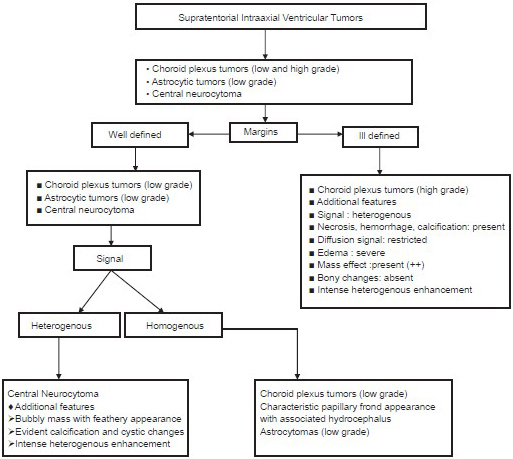
A retrospective analysis to assess the concordance of radiology (primarily MRI) with final histopathology report was done. Based on the most common incidence of tumor location and basic radiology findings, diagnostic algorithms were prepared according to six major locations (supratentorial intraaxial parenchymal, supratentorial intraaxial ventricular, supratentorial extraaxial, infratentorial intraaxial parenchymal, infratentorial intraaxial ventricular, infratentorial extraaxial) [Figures 1a–c and 2a–c]. The basic radiological features taken into consideration were: Margins (well defined, ill defined, and infiltrative), signal (homogenous and heterogeneous), contents (necrosis, hemorrhage and calcification), diffusion signal (restricted, not restricted, and partially restricted), edema (mild, moderate, severe, and absent), mass effect (present and absent), bony changes (with scalloping, erosion, and absent), and pattern of enhancement (homogenous, heterogeneous, and dural tail sign) [Figure 3]. Rare tumor locations and radiological findings were excluded. Differential diagnoses were arrived at based on these algorithms. A retrospective analysis to assess the concordance of radiology (primarily MRI) with final histopathology report was done in 204 cases of CNS tumors.
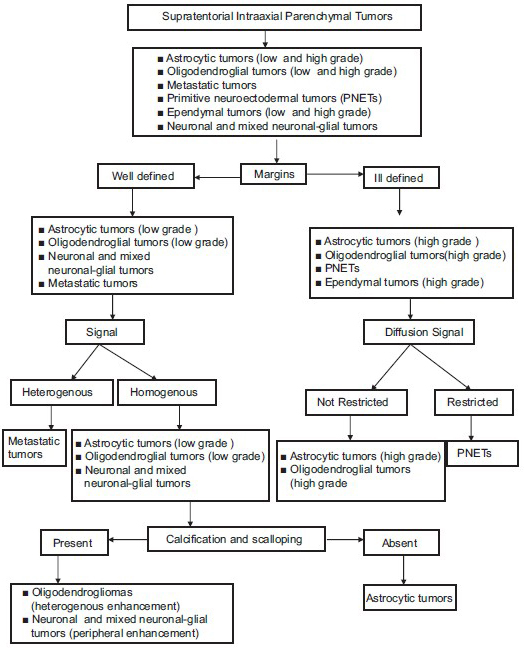
- Diagnostic algorithm for supratentorial intraaxial CNS tumors
- Diagnostic algorithm for supratentorial intraventricular CNS tumors
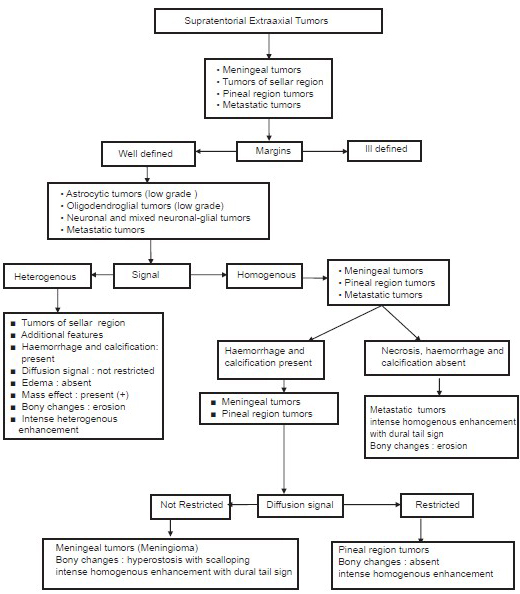
- Diagnostic algorithm for supratentorial extraaxial CNS tumors
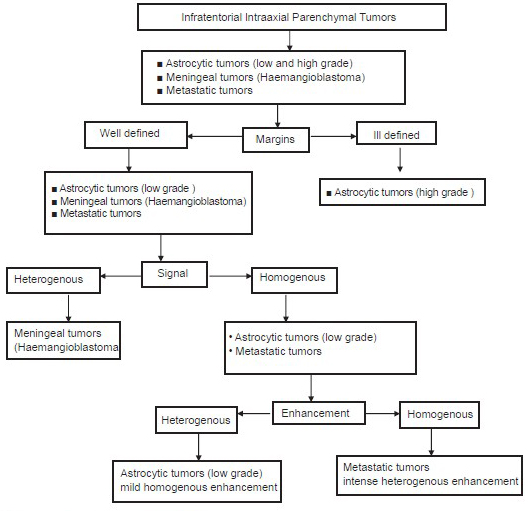
- Diagnostic algorithm for infratentorial intraaxial CNS tumors
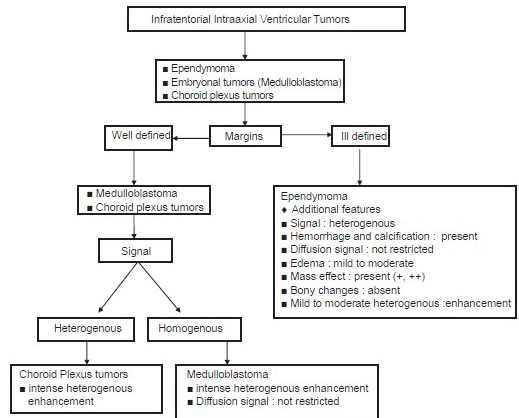
- Diagnostic algorithm for infratentorial intraventricular CNS tumors
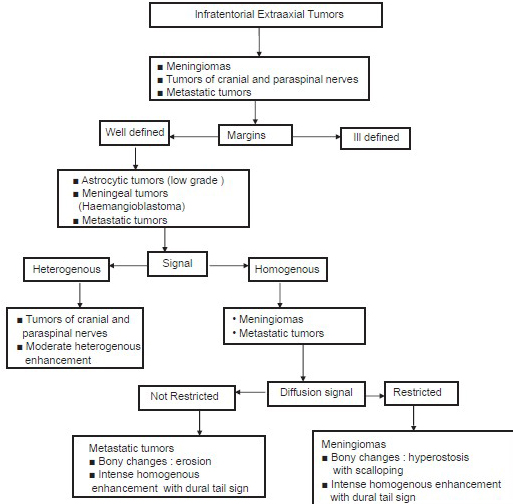
- Diagnostic algorithm for infratentorial extraaxial CNS tumors
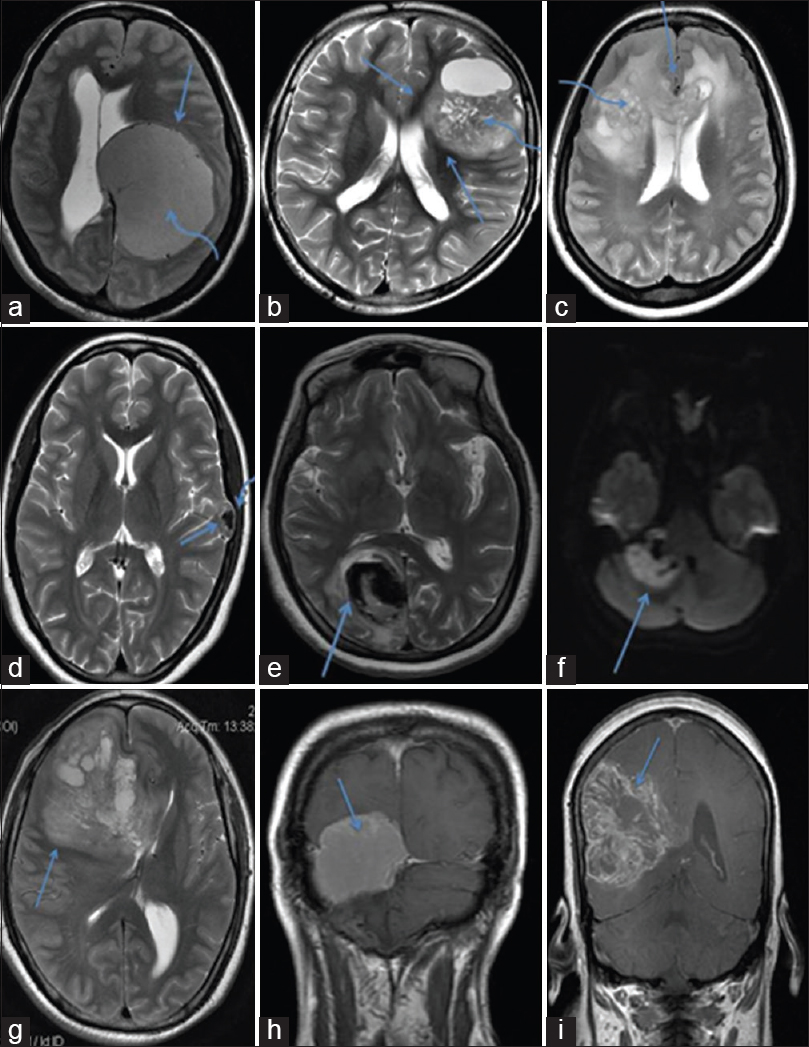
- (a) MR image showing well-defined margins (straight arrow) with homogenous signal (curved arrow), (b) ill-defined margins (straight arrow) and heterogeneous signal (curved arrow), (c) infiltrative margins (straight arrow) with necrotic areas (curved arrow), (d) calcified mass (straight arrow with bony scalloping (curved arrow), (e) hemorrhage, (f) restricted diffusion in an epidermoid cyst, (g) moderate perilesional edema with significant mass effect and midline shift, (h) intense homogenous contrast enhancement, (i) moderate heterogeneous contrast enhancement
Results
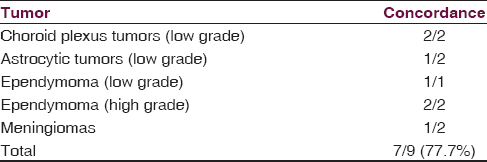
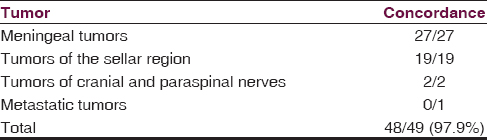
Location-wise radiology algorithms based on most common features were prepared and used to arrive at a provisional tumor diagnosis in the 204 cases received. Concordance with final histopathology diagnosis was then retrospectively evaluated. Concordance for the supratentorial intraaxial parenchymal location was 97.4%. Radiology-pathology concordance was seen in all high-grade astrocytomas, oligodendrogliomas (low and high grade), metastatic tumors, PNETs, high-grade ependymoma, neuronal and mixed neuro-glial tumors and tumors of the hematopoietic system. Lowest concordance was seen in low-grade astrocytomas, where out of 20 cases of low-grade astrocytomas, 2 cases were diagnosed as high-grade gliomas on radiology. In these two cases, though the radiological diagnosis regarding type of tumor was concordant with the histopathology but the radiological grading was discordant with the histopathology [Table 1]. The discordant histopathological diagnosis of these cases led to a reconsideration of the original radiological diagnoses. The MRI scans were studied retrospectively, and it was found that because of the heterogeneous signals and ill-defined margins, the diagnosis of high-grade gliomas was established in both the cases. This may be explained by the fact that even in low-grade gliomas, MRI may show heterogeneous signals and ill-defined margins. For the supratentorial intraaxial ventricular location, concordance was seen in 77.7% of cases; of the nine cases in this location, concordance was observed in low-grade choroid plexus tumors, low-grade and high-grade ependymomas. Low-grade astrocytomas and intra-ventricular meningiomas showed concordance in 50% of cases. The case of low-grade astrocytoma was diagnosed as choroid plexus papilloma on radiology, while the supratentorial intraaxial intraventricular meningioma was radiologically diagnosed as ependymoma [Table 2]. On retrospective analysis, it was found that radiological misdiagnosis occurred because of choroid plexus papilloma and low-grade astrocytoma being close differentials at this location, whereas the radiologic diagnosis of meningioma was not considered due to the extreme rarity of this entity at the supratentorial intraaxial intraventricular location. Concordance was 97.9% in the supratentorial extra-axial location; except for the lack of concordance in one case of metastatic tumor that was diagnosed as invasive meningioma on radiology, concordance was observed in meningeal tumors, tumors of the sellar region and tumors of cranial and paraspinal nerves [Table 3]. On retrospective radiologic analysis of the metastatic lesion, it was found that because of the lesion being solitary with bony involvement the diagnosis of invasive meningioma was established, although metastasis should have been considered as the first diagnosis on radiology.
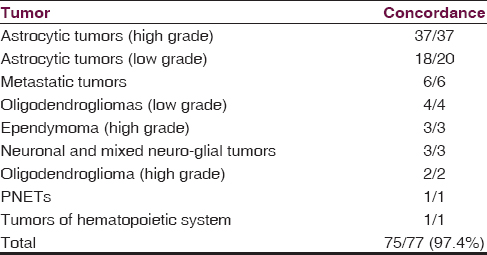
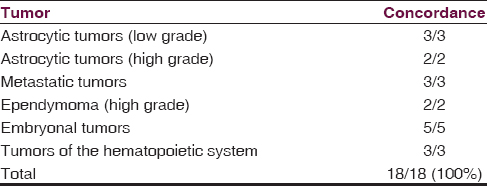
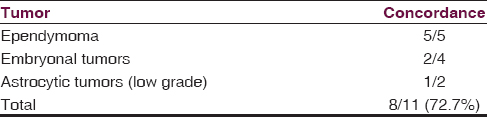
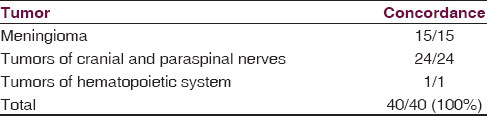
The infratentorial intraaxial parenchymal location showed 100% concordance with agreement in low-grade astrocytomas, high-grade astrocytomas, metastatic tumors, embryonal tumors, high-grade ependymomas and hemopoietic tumors [Table 4]. In the infratentorial intraaxial ventricular location, overall 72.7% concordance was observed, except for the lack of concordance in one case of low-grade astrocytoma and in two cases of medulloblastomas received, agreement was observed in low- and high-grade ependymomas. Both low-grade astrocytoma and medulloblastomas were diagnosed as ependymomas on radiology [Table 5]. Retrospective analysis revealed that the low-grade astrocytoma was misdiagnosed as ependymoma because of low-grade astrocytoma and ependymoma being the close differentials at this location; in addition, low-grade astrocytomas at this location are parenchymal rather than intraventricular. Radiologically medulloblastomas were misdiagnosed as ependymomas because of the areas of hemorrhage and the infiltrative growth pattern around Foramen of Magendie and Luschka suggesting ependymomas on radiology. Infratentorial extraaxial tumors showed 100% concordance in all tumors of cranial and paraspinal nerves, meningiomas and tumors of hematopoietic system [Table 6].
Discussion
Radiology findings are mentioned in the histopathology requisition forms as an essential practice at most of the centers, especially those dealing with neuropathology. These details can be used by the pathologists to narrow down the differential diagnoses and also in conjunction with the histopathology findings.[1] However, it has been our experience that pathologists are often unable to suitably interpret the radiology details at their disposal.
In an effort to make radiology more meaningful for the pathologists, simple algorithms based on the most common incidence of tumor location and basic radiology findings[2] were prepared to arrive at a radiologic provisional diagnosis.[34] Concordance with final histopathology diagnosis was then retrospectively analyzed.
The diagnostic algorithms were found maximally helpful in the infratentorial intraaxial parenchymal and infratentorial extraaxial regions (100%), followed by the supratentorial extraaxial region (97.9%), supratentorial intraaxial parenchymal region (97.4%), supratentorial intraaxial ventricular region (77.7%) and infratentorial intraaxial ventricular region (72.7%), respectively.
As far as tumor categories are concerned, concordance was maximal for high-grade astrocytomas, oligodendrogliomas (low and high grade), ependymomas (low and high grade), low-grade choroid plexus tumors, neuronal and mixed neuro-glial tumors, tumors of the hematopoietic system and tumors of the sellar region, tumors of cranial and paraspinal nerves (100%) followed by meningeal tumors (97.7%), metastatic tumors (90%), low-grade astrocytic tumors (85.1%) and embryonal tumors (80%). Among astrocytic tumors, high-grade astrocytomas showed maximal concordance but at the same time tumors in the category of low-grade astrocytomas showed a low concordance rate. This phenomenon was explained in a study by Iwama et al. where the authors had studied the histopathology of eight gliomas in correlation with MRI and CT findings. They mentioned that the signal intensities of gliomas on MRI did not correlate with the malignancy of the tumor.[5] In another study by Tovi et al., a comparative analysis between MRI findings and histopatholgy of malignant glial brain tumors was done. They concluded that though the degree of malignancy of the lesion as a whole can be assessed by MRI but it does not allow gliomas to be correctly delineated.[6]
These simplified radiology algorithms did provide clarity of thought and approach while interpreting radiology findings mentioned on the requisition forms. The narrowed down differential diagnoses is helpful while interpreting histopathological findings.
This approach can be used as an adjunct during histopathology reporting. However, it is important to bear in mind that such algorithms, at best, can serve only as a basic framework for the pathologists. There is no substitute to a detailed discussion with the radiologists.
Limitations of this study
Number of cases in few categories was too small, only common radiology features and locations were considered while preparing the algorithms.
Conclusion
A location-based approach to CNS tumors is helpful in establishing an appropriate differential diagnosis. The combination of a location-based algorithm with specific imaging findings, such as the type of margins and signal, nature of contents (necrosis, hemorrhage, and calcification), pattern of enhancement, presence or absence of edema, mass effect, bony changes, presence or absence of restriction on diffusion-weighted images, permits a narrowed differential diagnosis according to imaging findings.
It is hoped that this brief overview of radiology for the pathologists would be of help to the neuropathologists and, also, postgraduate students.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Radiologic-pathologic correlation of pediatric and adolescent spinal neoplasms: Part 2, Intradural extramedullary spinal neoplasms. AJR Am J Roentgenol. 2012;198:44-51.
- [Google Scholar]
- Does bony hyperostosis in intracranial meningioma signify tumor invasion? A radio-pathologic study. Neurol India. 2012;60:50-4.
- [Google Scholar]
- Diagnostic synergy in radiology and surgical neuropathology: Radiographic findings of specific pathologic entities. Arch Pathol Lab Med. 1998;122:620-32.
- [Google Scholar]
- Diagnostic synergy in radiology and surgical neuropathology: Neuroimaging techniques and general interpretation guidelines. Arch Pathol Lab Med. 1998;122:609-19.
- [Google Scholar]
- Correlation between magnetic resonance imaging and histopathology of intracranial glioma. Neurol Res. 1991;13:48-54.
- [Google Scholar]
- MR imaging in cerebral gliomas. Tissue component analysis in correlation with histopathology of whole-brain specimens. Acta Radiol. 1994;35:495-505.
- [Google Scholar]






