Translate this page into:
Surgically Relevant Bony Anatomical Variations in Paraclinoid Aneurysms-Three-Dimensional Multi-Detector Row Computed Tomography-Based Study
Address for correspondence: Dr. K. Suprasanna, Department of Radiology, Kasturba Medical College, Attavar, Mangalore - 575 001, Karnataka, India. E-mail: suprasannadr@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective:
To evaluate the proportion of surgically relevant anatomical variations such as caroticoclinoid foramen, interclinoid osseous bridge, and anterior clinoid pneumatization in patients with paraclinoid aneurysms based on computed tomography (CT) cerebral angiography studies.
Materials and Methods:
Fifty-four CT cerebral angiography studies showing paraclinoid aneurysms involving the cavernous, clinoid, and supraclinoid internal carotid artery (ICA) were retrospectively evaluated. Source images were processed for three-dimensional reconstructions to evaluate the presence and type of caroticoclinoid foramen, interclinoid osseous bridge, and multiplanar reconstructions with bone algorithm to study the type of pneumatization.
Results:
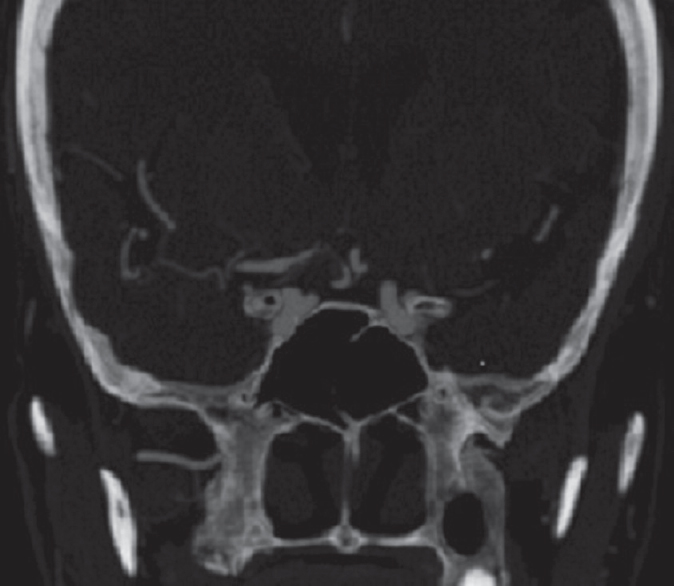
The study included 30 female and 24 male patients with mean age of 45.61 (10.47) years. Among the 108 sides studied in 54 patients, caroticoclinoid foramen was seen in 24 cases (22.22%), interclinoid osseous bridge was seen unilaterally in 1 case (0.9%), and pneumatization of anterior clinoid process occurred in 12 cases (11.11%). Incomplete caroticoclinoid foramen (11 cases) and Type I pneumatization (7 cases) were seen to be predominant subtypes. There was no statistically significant gender difference in the occurrence of caroticoclinoid foramen and anterior clinoid pneumatization. Seventy-four aneurysms were detected in 54 patients. Based on their location, 46 aneurysms involved supraclinoid ICA, 18 aneurysms in the clinoid segment, and 10 aneurysms in the cavernous segment. Caroticoclinoid foramen was most prevalent in clinoid aneurysms with 12 cases occurring in the clinoid segment.
Conclusion:
Notable proportions of caroticoclinoid foramen and pneumatization occur in cases of paraclinoid aneurysm. Radiological reports should emphasize on these surgically relevant bony anatomical variations.
Keywords
Caroticoclinoid
interclinoid osseous bridge
multi-detector computed tomography
paraclinoid
pneumatization
INTRODUCTION
Surgeries of paraclinoid aneurysms require wide operative exposure, which is facilitated by anterior clinoidectomy. Anatomical variations in paraclinoid region adversely affect anterior clinoidectomy with intra- and post-operative complications worsening the surgical outcome. These surgically relevant variations include caroticoclinoid foramen, interclinoid osseous bridge, and anterior clinoid pneumatization.
Caroticoclinoid foramen occurs due to fusion of the tips of the middle clinoid process and anterior clinoid process. The interclinoid osseous bridge is formed by the fusion of tips of the anterior and posterior clinoid processes. These structures restrict mobilization or retraction of internal carotid artery (ICA) complicating anterior clinoidectomy. Pneumatization of the anterior clinoid process with communication to sphenoid or ethmoid air cells is a potential risk factor for rhinorrhea after anterior clinoidectomy. Radiological reports in cases of paraclinoid aneurysms focus on the morphologic and topographic features of the aneurysm. However, preoperative detection of the bony anatomical variations in case of paraclinoid aneurysms by three-dimensional (3D) Multi-detector row computed tomography (MDCT) has a substantial role in avoiding surgical complications. Stull et al., in their study, has confirmed the accuracy and reliability of CT 3D rendered volume images in human autopsy remains.[1]
Various authors have proposed different classifications of ICA aneurysms. The present study terms the penetrating segment of ICA as the paraclinoid ICA, which includes the C4 (cavernous), C5 (clinoid), and C6 (ophthalmic) segments of ICA, as described by Bouthiller,[2] in accordance with a previous study.[3] The present study evaluates the presence of these surgically relevant bony anatomical variations in cases of paraclinoid aneurysms by 3D MDCT.
The aim of the study was to evaluate the proportion of surgically relevant anatomical variations such as caroticoclinoid foramen, interclinoid osseous bridge, and anterior clinoid pneumatization in patients with paraclinoid aneurysms based on CT cerebral angiography studies.
MATERIALS AND METHODS
CT cerebral angiography studies performed from January 2014 to June 2016 and showing the presence of paraclinoid aneurysms in patients of age groups 18–70 years were retrospectively evaluated. Proportions of caroticoclinoid foramen, interclinoid osseous bridge, and anterior clinoid pneumatization were assessed. Sample size of 54 patients was calculated based on an earlier study,[4] with a precision of 10% at 95% confidence interval. Source images of CT angiography studies taken in helical mode with section thickness of 0.625 mm using a 16 detector scanner (GE Brightspeed Elite 16, GE Healthcare, Chicago, USA) in patients with paraclinoid aneurysms were recorded. The technical parameters for cerebral CT angiography included a field of view of 22–25 mm, section thickness of 0.625 mm, tube voltage of 120 kV, dose of 320 mAs/section, and a helical pitch of 0.8. Images were then processed in bone algorithm with multiplanar reconstructions for the presence of anterior clinoid pneumatization and with 3D reconstructions for the presence of caroticoclinoid foramen and interclinoid osseous bridge by NEC Multisync LCD1990SXi.
Caroticoclinoid foramina were divided into complete, incomplete, and contact foramina. Incomplete foramen showed a gap at the fusion of the anterior and middle clinoid processes, whereas contact type was described when the anterior and middle clinoid processes were connected by an interclinoid suture. Pneumatization of the anterior clinoid process was classified according to the route of pneumatization as Type I (pneumatization occurring through the optic strut), Type II (through the anterior root), and Type III (via both the optic strut and the anterior root).[5] Cases which have undergone surgical intervention/endovascular treatment were excluded from the study. Cases with extensive vascular calcifications involving the cavernous and supraclinoid ICA hindering the visualization of paraclinoid region in 3D reconstructions were also excluded from the study. Since the study was retrospective in nature, radiation concerns were not an issue. Institutional Review Board approval was obtained.
Statistical analysis
Data analysis was done by SPSS 15.0 (SPSS for Windows, Version 15.0. Chicago, SPSS Inc) 15 for windows. Proportions of caroticoclinoid foramen and pneumatization were calculated. Statistical significance of variations between the genders was evaluated by Chi-square test. P < 0.05 was considered statistically significant.
RESULTS
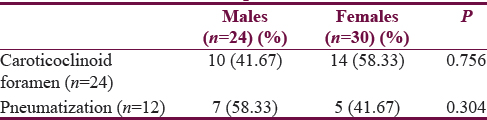
CT angiography studies of 54 patients with 3D reconstructions and volume rendering were evaluated which included 30 female and 24 male patients. The mean age of the patients was 45.61 years, with standard deviation of 10.27. (The minimum age in the study group was 25 years and the maximum age in the study group was 70 years.) Among the 108 sides studied in 54 patients, caroticoclinoid foramen was seen in 24 cases (22.22%) [Table 1 and Figure 1]. The interclinoid osseous bridge was seen unilaterally in 1 case (0.9%).
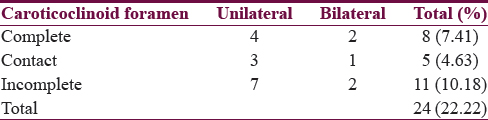
- (a) Caroticoclinoid foramen formed by the fusion of anterior and middle clinoid process is seen on the right side with a suture in between (contact type). The arrow points to the line of fusion. (b) Three-dimensional image showing the relation of the clinoid aneurysm to the anterior clinoid process in the axial view. Volume-rendered image of the skull has been superimposed on the three-dimensional image of the cerebral vessels. (c) Three-dimensional image of the cerebral vessels showing the presence of clinoid aneurysm. (d) Three-dimensional image showing the relation of the clinoid aneurysm to the anterior clinoid process in coronal view
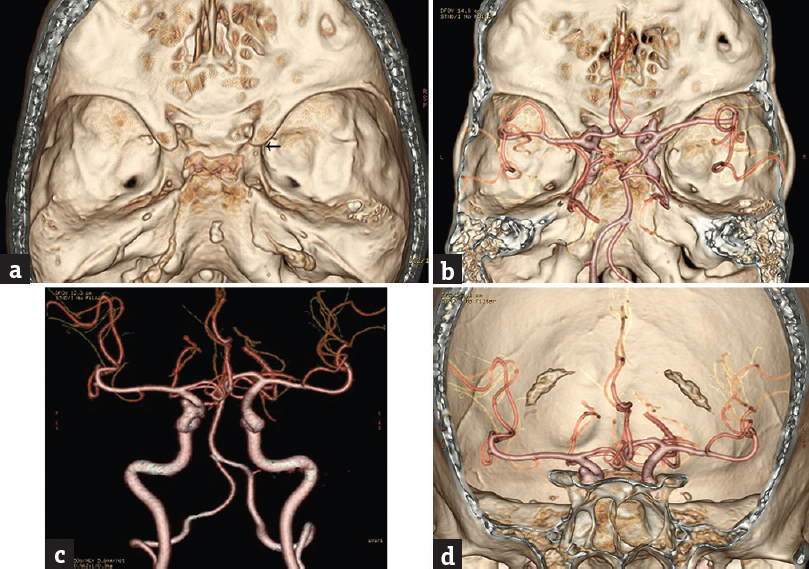
Twelve cases (11.11%) had pneumatization of the anterior clinoid process. Pneumatization was through the optic strut (Type I) in 7 cases and was through the anterior root (Type II) in 5 cases [Figures 2 and 3]. Type III pneumatization occurring through both the optic strut and anterior root was not recorded. Bilateral pneumatization occurred in 3 cases was only on the right side in 3 cases and only on the left side in 3 cases. There was no statistically significant gender difference in the occurrence of caroticoclinoid foramen and anterior clinoid pneumatization [Table 2].
- (a) Type I pneumatization occurring through the optic strut on the left side. (b) Type II pneumatization occurring through the anterior root on the right side. (c) Bilateral Type I pneumatization with communication to the sphenoid sinus. (d) Bilateral Type I pneumatization with communication to the ethmoid sinuses
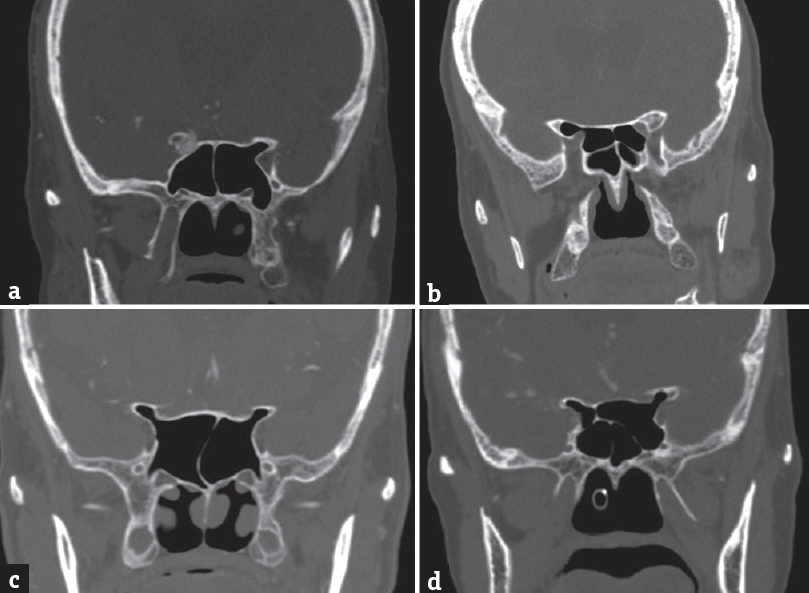
- Thick-slab computed tomography image showing the relationship of aneurysm to the pneumatized anterior clinoid process on the right side
A total of 74 aneurysms were detected in 54 patients, and 15 patients had multiple aneurysms. Based on their location, 46 aneurysms involved the supraclinoid ICA, 18 aneurysms were in the clinoid segment (between the level of clinoid undersurface to the clinoid roof or at the level of optic strut), and 10 aneurysms occurred in the cavernous segment. Caroticoclinoid foramen was most prevalent in clinoid aneurysms with 12 cases occurring in the clinoid segment.
DISCUSSION
Meticulous evaluation of anatomical variations in paraclinoid region preoperatively by imaging studies is a prerequisite in cases of paraclinoid aneurysms contemplating to undergo anterior clinoidectomy. Anterior clinoidectomy ensures adequate surgical exposure in paraclinoid surgeries but is a critical procedure with potential complications due to its deep location between the ICA and the second and third cranial nerves. Anatomical variations such as caroticoclinoid foramen, interclinoid osseous bridge, and anterior clinoid pneumatization further necessitate appropriate modifications in the procedure.
The incidence of caroticoclinoid foramen has been studied in normal population by various authors with results varying from 6.27%[6] to 35.67%.[7] Ota et al.[4] evaluated the occurrence of the caroticoclinoid foramen in patients with paraclinoid aneurysms to be present in 16.6% using MDCT. The present study observes a higher proportion of caroticoclinoid foramen (22%). The interclinoid osseous bridge was seen unilaterally only in a single case (0.9%), which is significantly lower as compared to the study by Ota et al. (2.77%).[4]
The proportion of pneumatization was 11.11%, which is slightly higher as compared to the study by Abuzayed et al., which showed the incidence as 9.6%.[8] Type I pneumatization occurring through the optic strut was seen to be most prevalent. The pneumatized anterior clinoid process has air cells which communicate with the sphenoid and/or ethmoid air cells. Removal of pneumatized anterior clinoid process would result in mucosal tear with the opening of these sinuses causing rhinorrhea. Furthermore, cerebrospinal fluid leaks may occur due to inadequate closure. Preoperative evaluation of anterior clinoid process pneumatization helps the surgeon in estimating the extent of drilling of the anterior clinoid process.
In the present study, caroticoclinoid foramen was most prevalent in cases of clinoid aneurysms (16.22%). The optic strut is a definitive anatomic landmark for differentiation of intradural and cavernous ICA (extradural) aneurysms and is well visualized in CT.[9] Aneurysm at the optic strut is considered to be involving the clinoid segment of ICA. Further studies with larger samples are required to establish the association between caroticoclinoid foramen and involvement of particular segment of ICA in aneurysms.
The presence of caroticoclinoid foramen should be looked for in unenhanced images in the bone window with 3D reconstructions. It is located lateral to the sella and cavernous sinus. The average transverse diameter of the foramen has been calculated to be 5.32 ± 0.52 mm in a previous study.[7]
The anterior clinoid process, which is the deeper extension of the medial aspect of sphenoid wing, hampers adequate visualization of the paraclinoid and parasellar region. Adequate surgical exposure of this region is crucial for achieving conclusive results in aneurysm clipping. Anterior clinoidectomy makes the surgical field more spacious facilitating the handling of microsurgical instruments with much more illumination of the operating microscope.[10] Furthermore, easier mobilization of the intracranial ICA and optic nerve is facilitated by anterior clinoidectomy. Morphometric studies evaluating quantification of exposure of C6 segment of ICA and optic nerve following anterior clinoidectomy show significant enlargement of the opticocarotid window, following anterior clinoidectomy.[11] Further, anterior clinoidectomy enables surgical treatment of intracavernous pathology by opening of the cavernous sinus after the procedure and is a component of transcavernous approach.[10] Various techniques and modifications of anterior clinoidectomy have been proposed.[12] Intradural en bloc removal of the anterior clinoid process has been advocated for clinoidectomy.[13]
Previous studies have assessed the bony variations of the paraclinoid region by anatomical evaluation[71415] and by MDCT in normal controls.[5816] The present study evaluates these variations in CT angiographic studies of paraclinoid aneurysms retrospectively. The limitations of the study are smaller sample size, retrospective nature of the study, and unavailability of surgical follow-up of the patients.
CONCLUSION
The proportions of caroticoclinoid foramen and anterior clinoid pneumatization in the cases of paraclinoid aneurysms were notable. The radiological reports and 3D reconstructions of aneurysms emphasize on the morphological features of the aneurysms. However, little importance is given to the anatomical bony variations, which can be easily detected in 3D reconstructions in the bone algorithm of unenhanced images. Preoperative assessment and radiological reporting of these variations are imperative in cases of paraclinoid aneurysms as they play a critical role in avoiding disastrous complications, and appropriate surgical modifications would ensure an improved surgical outcome.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Accuracy and reliability of measurements obtained from computed tomography 3D volume rendered images. Forensic Sci Int. 2014;238:133-40.
- [Google Scholar]
- Segments of the internal carotid artery: A new classification. Neurosurgery. 1996;38:425-32.
- [Google Scholar]
- Distinction between intradural and extradural aneurysms involving the paraclinoid internal carotid artery with T2-weighted three-dimensional fast spin-echo magnetic resonance imaging. J Korean Neurosurg Soc. 2010;47:437-41.
- [Google Scholar]
- Surgical microanatomy of the anterior clinoid process for paraclinoid aneurysm surgery and efficient modification of extradural anterior clinoidectomy. World Neurosurg. 2015;83:635-43.
- [Google Scholar]
- Anatomical variations in pneumatization of the anterior clinoid process. J Neurosurg. 2007;106:170-4.
- [Google Scholar]
- Anatomical variations of the clinoid process of the human sphenoid bone. Arq Cent Estud Curso Odontol. 1988-1989;25-26:9-11.
- [Google Scholar]
- Anatomy of the clinoidal region with special emphasis on the caroticoclinoid foramen and interclinoid osseous bridge in a recent Turkish population. Neurosurg Rev. 2004;27:22-6.
- [Google Scholar]
- Pneumatization degree of the anterior clinoid process: A new classification. Neurosurg Rev. 2010;33:367-73.
- [Google Scholar]
- Distinction between paraclinoid and cavernous sinus aneurysms with computed tomographic angiography. Neurosurgery. 2003;52:1131-7.
- [Google Scholar]
- How to perform selective extradural anterior clinoidectomy. In: Sindou M, ed. Practical Handbook of Neurosurgery. New York: Springer; 2009. p. :155-66.
- [Google Scholar]
- Evidence for the improved exposure of the ophthalmic segment of the internal carotid artery after anterior clinoidectomy: Morphometric analysis. Acta Neurochir (Wien). 2006;148:971-5.
- [Google Scholar]
- The “no-drill” technique of anterior clinoidectomy: A cranial base approach to the paraclinoid and parasellar region. Neurosurgery. 2009;64(3 Suppl):ons96-105.
- [Google Scholar]
- Intradural en-bloc removal of the anterior clinoid process. Acta Neurochir (Wien). 2004;146:505-9.
- [Google Scholar]
- Significance of anatomic variants of bony surroundings of the internal carotid artery and their significance for lateral surgical approaches to the cavernous sinus. Ann Acad Med Stetin. 2003;49:205-29.
- [Google Scholar]
- Anatomical variations and morphometric study of the optic strut and the anterior clinoid process. Bosn J Basic Med Sci. 2012;12:88-93.
- [Google Scholar]
- Optic strut and para-clinoid region-Assessment by multi-detector computed tomography with multiplanar and 3 dimensional reconstructions. J Clin Diagn Res. 2015;9:TC06-9.
- [Google Scholar]






