Translate this page into:
Venous Sinus Stenting using Transcranial Access for the Treatment of Idiopathic Intracranial Hypertension in a Pediatric Patient
Address for correspondence: Dr. Thomas J. Buell, Department of Neurological Surgery, University of Virginia, Charlottesville, Virginia 22908, USA. E-mail: tjb4p@virginia.edu
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
A 4-year-old male with headaches, papilledema, intracranial hypertension, and bilateral transverse sinus (TS) stenosis underwent attempted percutaneous placement of a right TS stent. Stent deployment was not technically feasible due to the stiffness of the stent and tortuosity of the patient's jugular bulb. Therefore, the patient underwent hybrid endovascular stenting of the right TS using neuronavigation and direct access of the TS following a single burr hole craniectomy. Two Express 8 mm × 17 mm balloon-mounted stents were deployed into the right TS, which resulted in obliteration of the preexisting trans-stenosis pressure gradient and decreased intracranial parenchymal pressure as monitored through an intracranial pressure bolt. The patient's headaches and papilledema resolved, and follow-up imaging demonstrated no in-stent or stent-adjacent stenosis. This case demonstrates the feasibility of combining minimally invasive open surgical access to allow direct cannulation for venous sinus stenting.
Keywords
Endovascular
idiopathic intracranial hypertension
stent
outcomes
pressure gradient
pseudotumor cerebri
venous stenosis
INTRODUCTION
Idiopathic intracranial hypertension (IIH) is infrequently diagnosed in prepubertal children.[1] Venous sinus outflow obstruction, typically from stenotic or occluded transverse sinuses (TS), is evident in many IIH patients.[23] Cerebrospinal fluid (CSF) diversion has traditionally been the main surgical treatment for IIH patients who are refractory to medical therapy. However, ventriculoperitoneal and lumboperitoneal shunt placement can be challenging due to the slit-like ventricles and large body habitus which are often associated with IIH. Furthermore, these shunts can become occluded, resulting in repeat surgery for shunt revisions in some patients. Due to the limitations of CSF diversion, endovascular treatment of IIH with venous sinus stenting (VSS) has recently emerged as a promising alternative therapy for patients with evidence of TS stenosis associated with a significant trans-stenosis pressure gradient.[45] Due to the rarity of IIH in the pediatric population, the outcomes of VSS in this subgroup of patients are poorly understood. We present a case of a very young pediatric IIH patient who underwent VSS using transcranial access after failed endovascular treatment from a transfemoral route.
CASE REPORT
A 4-year-old male with no medical history presented with 2 weeks of retro-orbital headaches, emesis, visual complaints, and hypersomnolence. There was a family history significant for IIH in the mother and maternal grandmother. Ophthalmologic evaluation demonstrated anomalous appearing optic discs and significant thickening of the nerve fiber layer bilaterally, consistent with papilledema. Brain magnetic resonance imaging (MRI) showed findings consistent with intracranial hypertension including a Chiari I malformation with 8 mm of herniation of the cerebellar tonsils below the foramen magnum, dilation of the optic nerve sheaths, and a partially empty sella [Figure 1a and b]. Brain MR venography (MRV) showed severe focal stenosis of the distal right TS and arachnoid granulations in the left distal TS partially filling the lumen [Figure 1c and d]. MRI of the cervical and thoracic spine was unremarkable and without evidence of a syrinx. An intraparenchymal intracranial pressure (ICP) monitor was placed, and mean ICPs were 30–40 mmHg, with a range of 20–60 mmHg. The parents were presented with the various treatment options including acetazolamide therapy, shunt placement, and VSS. After a lengthy conversation with the parents, they elected to proceed with VSS. The patient started daily aspirin 121.5 mg and clopidogrel 18.75 mg. Aspirin and P2Y assays were 539 (therapeutic level <551) and 170 (therapeutic level <208), respectively, after initiation of dual antiplatelet medication. Six-vessel cerebral angiography revealed no evidence of aneurysm, fistula, or arteriovenous shunting. Venography showed severe bilateral distal TS stenosis caused by arachnoid granulations, with resultant elevated mean venous pressures (MVP) in the torcula and proximal and middle right TS. MVP in the torcula was 34 mmHg and decreased to 11 mmHg in the sigmoid sinus, which indicates that the trans-stenosis pressure gradient across the TS was 23 mmHg. Stent deployment into the right TS was attempted multiple times from a transfemoral route but was unsuccessful due to stiffness of the stent and tortuosity of the jugular bulb.

- Brain magnetic resonance imaging showed findings consistent with intracranial hypertension including a Chiari I malformation with 8 mm of herniation of the cerebellar tonsils below the foramen magnum, dilation of the optic nerve sheaths, and a partially empty sella (a and b). Brain magnetic resonance venography showed severe focal stenosis of the distal right transverse sinus and arachnoid granulations in the left distal transverse sinus partially filling the lumen (c and d)
To bypass the tortuous jugular bulb, we decided to perform the VSS procedure with direct transcranial access of the right TS. The patient was positioned supine in a hybrid operating room with the head turned laterally (right side facing up). We used the StealthStation (Medtronic, Minneapolis, MN, USA) frameless stereotactic navigation system to localize the right TS. A single burr hole was placed over the right TS [Figure 2a]. A 19G single wall puncture needle was then used to cannulate the sinus, and a 7F 4 cm sheath was introduced over a 0.035 guidewire. Contrast was injected through the sheath under fluoroscopy to confirm the correct position within the right TS. Microcatheter MVP measurements were then performed and confirmed an elevated trans-stenosis gradient measuring 18 mmHg under general anesthesia.[6] A 0.035 guidewire was then placed across the stenosis into the right internal jugular vein, over which an 8 mm × 17 mm Express balloon-mounted stent was deployed (Boston Scientific, Washington DC, USA). Poststent angiography showed incomplete resolution of the stenosis, so a second 8 mm × 17 mm Express stent was placed, which resolved the stenosis [Figure 2b]. Balloon mounted stents were chosen over self-expanding stents to take into account future growth of the intracranial vault and to allow for future intervention to increase stent diameter should it become necessary. Venous manometry showed obliteration of the previous trans-stenosis gradient and the ICPs started to decrease from 37 to 15 mmHg immediately. The right internal carotid artery was then catheterized with a 4F diagnostic catheter from a transfemoral route, and arteriography showed patency of the stent and right TS. The 7F short sheath was then removed from the right TS, and hemostasis was obtained with Gelfoam and manual pressure.
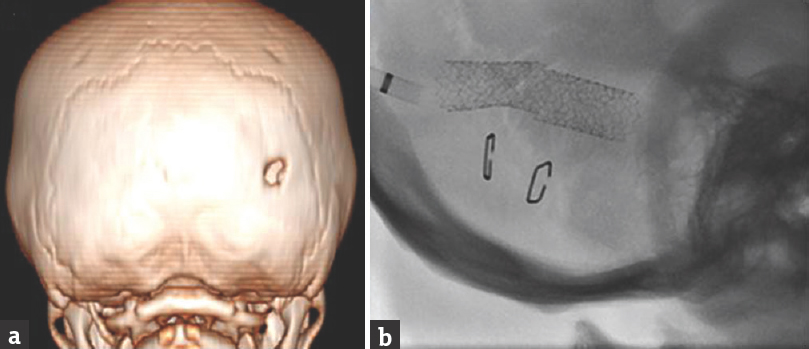
- Three-dimensional reconstruction of head computed tomography showing a single burr hole placed over the right transverse sinus (a). This is a fluoroscopic image showing two 8 mm × 17 mm Express balloon-mounted stents within the right transverse sinus (Boston Scientific, Washington DC, USA) (b)
Postoperative brain computed tomography showed no complications. The mean post-VSS ICPs were <20 mmHg, with a range of 10–30 mmHg. The patient's headaches improved, and he was discharged on daily dual antiplatelet therapy. Brain MRI/MRV 2 weeks after VSS demonstrated partial resolution of the Chiari I malformation, partially reduced empty sella and patency of the TS stents. Three-month follow-up angiography showed patency of the stents and a maximum venous pressure gradient of 4 mmHg [Figure 3a and b]. Four-month follow-up ophthalmologic examination revealed resolved bilateral optic disc edema and normal retinal optical coherence tomography (OCT). Brain MRI/MRV 6 months after VSS continued to demonstrate less evidence of intracranial hypertension, and patency of the transverse sinus stents [Figure 3c and d]. Twenty-month follow-up ophthalmological examination and retinal OCT remained stable, and the parents and patient continued to report resolution of preoperative symptoms.
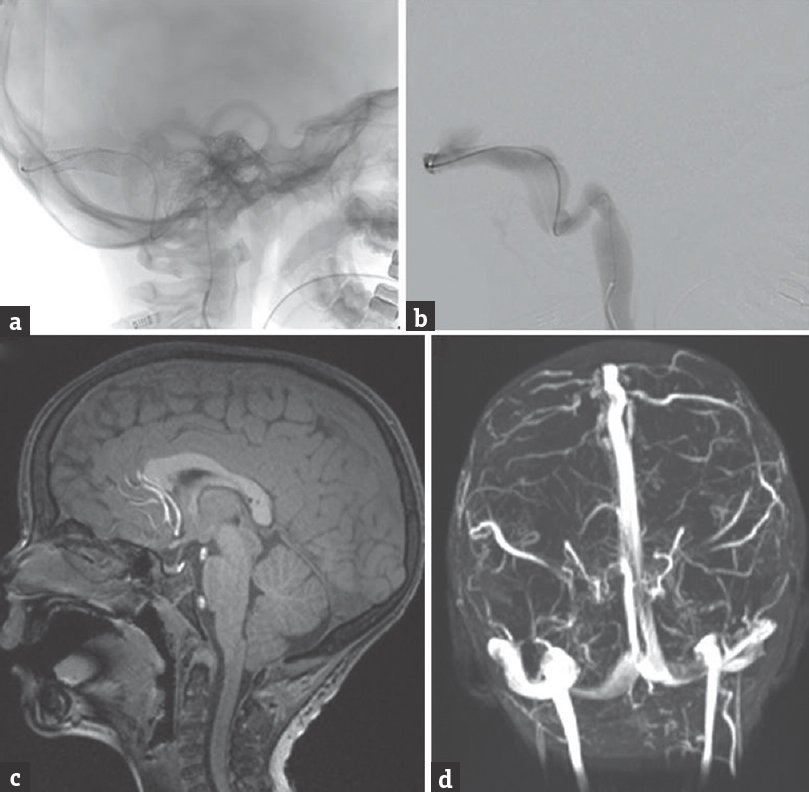
- Three-month follow-up angiography showed patency of the stents (a and b). Brain magnetic resonance imaging and venography demonstrated partial resolution of the Chiari I malformation, partially reduced empty sella, and patency of the transverse sinus stents (c and d)
DISCUSSION
IIH is uncommon in young children and, like in adults, preferentially affects females. As such, IIH in a prepubertal male is particularly rare, with an estimated incidence of 0.4 in 100,000.[1] IIH has been found to be associated with veno-occlusive disease, and affected patients are frequently found to have stenosis of one or both TS.[234] The first-line treatment for IIH is medical therapy with acetazolamide.[7] When medical therapy fails, CSF diversion has typically been the first-line surgical treatment for IIH. There is mounting evidence that, in patients with venous sinus stenosis and a significant trans-stenosis pressure gradient, VSS can improve or reverse the neurological, ophthalmologic, and radiologic signs of IIH.[234]
We present a case of the youngest IIH patient to undergo successful treatment with VSS. Furthermore, this is the first reported case of VSS performed through direct transcranial access of the TS. Direct transcranial access for neurointerventional treatment of other intracranial lesions has been successful.[89] This case demonstrates the feasibility of combining open surgical access to allow direct cannulation for VSS to treat pediatric IIH. A transcranial approach may be considered when conventional percutaneous methods are not feasible. In our patient, the stiffness of the stent combined with the tortuosity of the jugular bulb prevented stent deployment from a transfemoral route. In adults, larger support catheters may allow for transvenous navigation, but these catheters are often not options in very young pediatric patients, whose smaller venous structures are unable to accommodate these relatively large-bore catheters. We used stereotactic neuronavigation to precisely localize the TS to minimize the size of the burr hole and dural exposure.[101112131415] Furthermore, since ICP monitoring was performed concurrently with VSS, we provide evidence for a direct relationship between venous sinus stenosis and intracranial hypertension.[16]
The limitations of our combined technique for IIH treatment should be noted. First and foremost, the relationship between TS stenosis and the pathophysiology of IIH remains poorly defined. Specifically, it is unknown if venous sinus stenosis is the underlying etiology of IIH, or if it instead is an epiphenomenon which represents a neuroimaging manifestation of increased ICP. Prior reports have shown resolution of venous sinus stenosis after CSF diversion.[17] Additionally, the relative long-term efficacy of VSS compared to CSF diversion for IIH has not been determined, which is a topic of particular importance in the pediatric population. A randomized trial comparing VSS to CSF diversion for medically refractory IIH is necessary to address this issue. Another unresolved topic is the minimum trans-stenosis pressure gradient which is necessary to realize a benefit from VSS. This cutoff value varies widely across institutions and confounds comparisons of VSS outcomes among different series.[5] Some neurointerventionalists have used 8 mmHg as a minimum trans-stenosis gradient before VSS;[1819] however, some patients may still benefit from endovascular treatment of lower gradients.[20]
A disadvantage of VSS in our case is the necessity for temporary antiplatelet therapy in a young child, which limits his ability to participate in contact sports and predisposes him to a greater hemorrhage risk from trauma. In addition, direct puncture of the TS may have resulted in sinus thrombosis and occlusion, which would have further exacerbated the patient's symptoms. Due to the risks and incompletely understood long-term outcomes of transcranial VSS, this technique should be reserved for only the most carefully selected cases of IIH.
CONCLUSIONS
VSS may be an effective interventional alternative to CSF diversion for the treatment of IIH in pediatric patients. In IIH patients with venous sinus stenosis and a significant trans-stenosis pressure gradient, VSS reduces neurological, ophthalmologic, and radiologic signs of intracranial hypertension. Due to the rigidity of venous stents and unique anatomic constraints of the venous system in young children, stent deployment from a transfemoral approach may not be feasible. In carefully selected patients, a transcranial approach can safely provide direct access to the affected TS for VSS.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Pediatric pseudotumor cerebri: Descriptive epidemiology. Can J Neurol Sci. 1997;24:219-21.
- [Google Scholar]
- Elevated intracranial venous pressure as a universal mechanism in pseudotumor cerebri of varying etiologies. Neurology. 1996;46:198-202.
- [Google Scholar]
- Cerebral venography and manometry in idiopathic intracranial hypertension. Neurology. 1995;45:2224-8.
- [Google Scholar]
- Venous sinus stenting for refractory benign intracranial hypertension. Lancet. 2002;359:228-30.
- [Google Scholar]
- Endovascular treatment of venous sinus stenosis in idiopathic intracranial hypertension: Complications, neurological outcomes, and radiographic results. ScientificWorldJournal 2015 2015:140408.
- [Google Scholar]
- Intracranial venous pressures under conscious sedation and general anesthesia. J Neurointerv Surg 2017 pii: neurintsurg-2017-012984
- [Google Scholar]
- Effect of acetazolamide on visual function in patients with idiopathic intracranial hypertension and mild visual loss: The idiopathic intracranial hypertension treatment trial. JAMA. 2014;311:1641-51.
- [Google Scholar]
- Onyx embolization of an intracranial hemangiopericytoma by direct transcranial puncture. Interv Neuroradiol. 2013;19:466-70.
- [Google Scholar]
- Direct transcranial puncture for Onyx embolization of a cerebellar hemangioblastoma. J Clin Neurosci. 2014;21:1040-3.
- [Google Scholar]
- Selective image-guided venous sinus exposure for direct embolization of dural arteriovenous fistula: Technical case report. Surg Neurol. 2008;69:192-6.
- [Google Scholar]
- A single burr hole approach for direct transverse sinus cannulation for the treatment of a dural arteriovenous fistula. J Neurointerv Surg. 2015;7:e5.
- [Google Scholar]
- Direct packing of the isolated sinus in patients with dural arteriovenous fistulas of the transverse-sigmoid sinus. J Neurosurg. 1998;88:449-56.
- [Google Scholar]
- Transcranial approach for venous embolization of dural arteriovenous fistulas. J Neurosurg. 2002;97:280-6.
- [Google Scholar]
- Single stage transcranial exposure of large dural venous sinuses for surgically-assisted direct transvenous embolization of high-grade dural arteriovenous fistulas: Technical note. Acta Neurochir (Wien). 2012;154:1855-9.
- [Google Scholar]
- Combined surgical and endovascular management of a complex posttraumatic dural arteriovenous fistula of the tentorium and straight sinus. J Neuroimaging. 2004;14:273-6.
- [Google Scholar]
- Venous sinus stenting for reduction of intracranial pressure in IIH: A prospective pilot study? J Neurosurg 2016:1-8. DOI:10.3171/2016.8.JNS16879
- [Google Scholar]
- Reversibility of venous sinus obstruction in idiopathic intracranial hypertension. AJNR Am J Neuroradiol. 2007;28:656-9.
- [Google Scholar]
- Resolution of pulsatile tinnitus after venous sinus stenting in patients with idiopathic intracranial hypertension. PLoS One. 2016;11:e0164466.
- [Google Scholar]
- Venous Sinus Stenting in Idiopathic Intracranial Hypertension: Results of a Prospective Trial. J Neuroophthalmol. 2017;37:113-121.
- [Google Scholar]
- A pilot study and novel angiographic classification for superior sagittal sinus stenting in patients with non-thrombotic intracranial venous occlusive disease. J Neurointerv Surg 2017 pii: Neurintsurg-2016-012906
- [Google Scholar]






