Translate this page into:
Non-typhoid Salmonella spondylodiscitis – An unusual organism in the back
*Corresponding author: Vaishak Balekkala Bhat, Department of Orthopedics, Kasturba Medical College Mangalore, Manipal Academy of Higher Education, Manipal, Karnataka, India. vaishak.bhat@manipal.edu
-
Received: ,
Accepted: ,
How to cite this article: Bhat VB, Bhat A, Kaur H, Thota S, Vashemane KV. Non-typhoid Salmonella spondylodiscitis – an unusual organism in the back. J Neurosci Rural Pract. doi: 10.25259/JNRP_59_2025
Abstract
Non-typhoidal Salmonella (NTS), a Gram-negative bacillus, is a common etiological of gastroenteritis but is not associated with spondylodiscitis. This is a case report depicting an uncommon presentation of spondylodiscitis in an elderly patient, a fish consumer with no preceding gastrointestinal (GI) symptoms or fever contributing new insights into spinal infections and microbiology. A 62-year-old female patient who was recently diagnosed with type 2 diabetes mellitus presented with progressive mid-back pain for two months. She had no history of fever, recent trauma, or any GI symptoms. The patient is a regular consumer of fish, a potential source of NTS infection. Physical examination revealed tenderness over the T0-T10 region with restricted spinal movements, and inflammatory markers were elevated. Magnetic resonance imaging revealed T0-T10 vertebral collapse with end plate destruction with fluid collections leading us to a diagnosis of spondylodiscitis. A percutaneous biopsy and laboratory analysis confirmed the presence of Salmonella enterica serovar Typhimurium. The patient was treated with intravenous ceftriaxone followed by ciprofloxacin. The case highlights the importance of considering NTS as a potential pathogen in cases of spondylodiscitis, even without preceding GI symptoms, especially when the patient is a regular consumer of fish. It also emphasizes the need for early laboratory workup, antibiotic therapy, and comprehensive imaging.
Keywords
Biopsy
Medical management
Non-typhoidal Salmonella ser. Typhimurium
Spondylodiscitis
INTRODUCTION
Salmonella spp. are Gram-negative bacilli belonging to the Enterobacteriaceae family. The most common route of infection is through ingestion of contaminated food and water. Salmonella Typhi causes a systemic illness, but non-Salmonella Typhi primarily causes gastroenteritis.[1] The infection could disseminate to other sites by hematogenous spread to the genitourinary tract, skin, and respiratory tract. Dissemination to the spine is mostly due to arterial supply to vertebral bodies and even the venous circulation through retrograde flow from the pelvic venous plexus to the paravertebral plexus.[2,3]
The most common history of presenting illness is that of gastroenteritis such as diarrhea, abdominal pain, and fever.[4] However, our patient did not have any history pertaining to that of gastroenteritis and had come with the chief complaint of back pain.
CASE REPORT
Patient information
The patient, a 62-year-old female, presented with chief complaints of mid-back pain for two months. The pain was progressive and insidious in onset. The patient was a known asthmatic but was not on medication. There was no history of recent trauma, fever, contact with a tuberculosis patient, weight loss, or radiculopathy. The patient was then recently diagnosed with type 2 diabetes mellitus (DM) and was on treatment. She had a mixed diet and regularly consumed fish. She was a non-smoker, with no history of consumption of alcohol or drugs. There was no significant family history.
Clinical findings
A general physical examination revealed a dull shriveled look, with poor nourishment. Spine examination of the dorsal spine showed senile kyphosis with tenderness at the T9-T10 level. The range of motions was painfully restricted. Neurological examinations, bowel and bladder were normal.
Diagnostic assessment
Inflammatory markers in the blood showed elevated C-reactive protein (CRP) 128 mg/L and erythrocyte sedimentation rate (ESR) 80 mm/h, total counts of 10, 080. An X-ray revealed D9-D10 collapse with end-plate irregularity and destruction.
Magnetic resonance imaging (MRI) of the dorsal region with whole spine screening showed hyperintense signal intensities in T2-weighted imaging, short tau inversion recovery, and isointense in T1-weighted imaging. These abnormal signal intensities were seen in the T9 and T10 vertebrae and the disc, extending into the T9 pedicle. There were fluid collections around the spinal canal. The MRI was suggestive of collection pointing out to be infective spondylodiscitis (SD) suggestive of tuberculosis [Figure 1]. MRI of the brain was done to rule out skip lesions. Blood tests revealed that the patient’s hemoglobin A1C level was 12.5 with random blood glucose of 300 mg/dL She underwent percutaneous biopsy using a Jamshidi needle under local and monitored anesthesia care. Materials were sent for gram staining, culture, sensitivity, cartridge based nucleic acid amplification test (CB-NAAT), and histopathology (HPE).
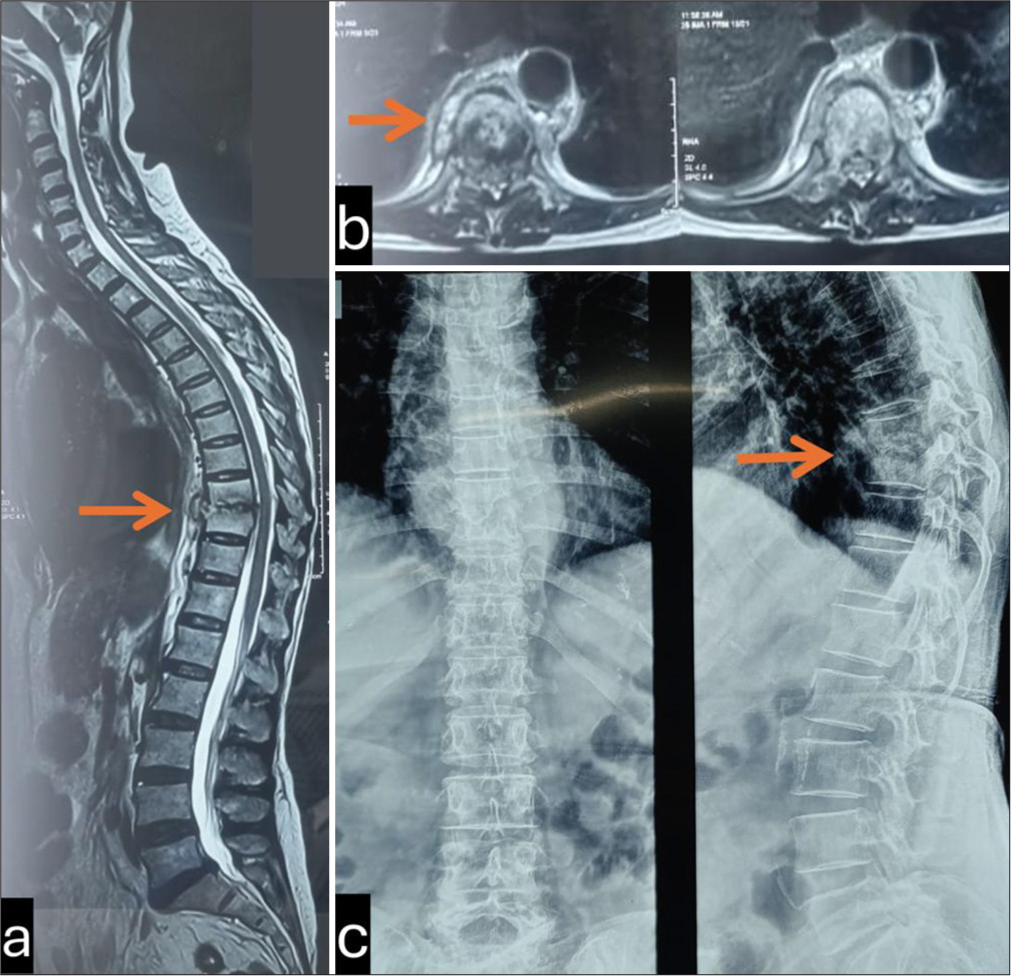
- Initial radiological investigations, (a) Showing T2Wi Sagittal MR1 image with hyperintensity in D9-D10 (arrow) disc space s/o spondylodiscitis, (b) Axial MRI of D9-D10 (arrow) T2Wi showing the collection in the disc space. (c) Plain X-ray Ap/Lat of Dorsal spine showing D9-D10 (arrow) collapse with end plate degeneration with vertebral collapse.
Upon a histopathological examination, bone tissue section study showed fragments of degenerated disc tissue with abundant fibrin-hemorrhagic material, with aggregates of chronic inflammatory infiltrate staining and CB-NAAT was negative. Gram staining showed the presence of polymorphonuclear cells. The culture was positive for non-Salmonella Ser. Typhimurium. The bacteria showed susceptibility to trimetho- prim, ciprofloxacin, ampicillin, cefotaxime, ceftriaxone, azithromycin, and chloramphenicol.
Therapeutic intervention
An infection disease specialist was consulted after which she received two weeks of intravenous (IV) ceftriaxone 1 gm twice a day followed by IV ciprofloxacin for four weeks. After six weeks, the patient had clinical improvement and reduction of pain, ESR was 28, and CRP was unelevated. The patient was switched to oral antibiotics. The patient received ciprofloxacin 750 mg twice a day and azithromycin 500 mg once daily for two months.
Follow-up and outcomes
During the treatment course, the patient had deglycation and Achilles tendinitis after which ciprofloxacin was discontinued. After eight months of therapy, the patient exhibited radiological resolution [Figure 2]. The patient was counseled about safe food and water practices. She was also advised osteoporotic treatment with an injection of teriparatide 20 mcg subcutaneously once daily for six months.
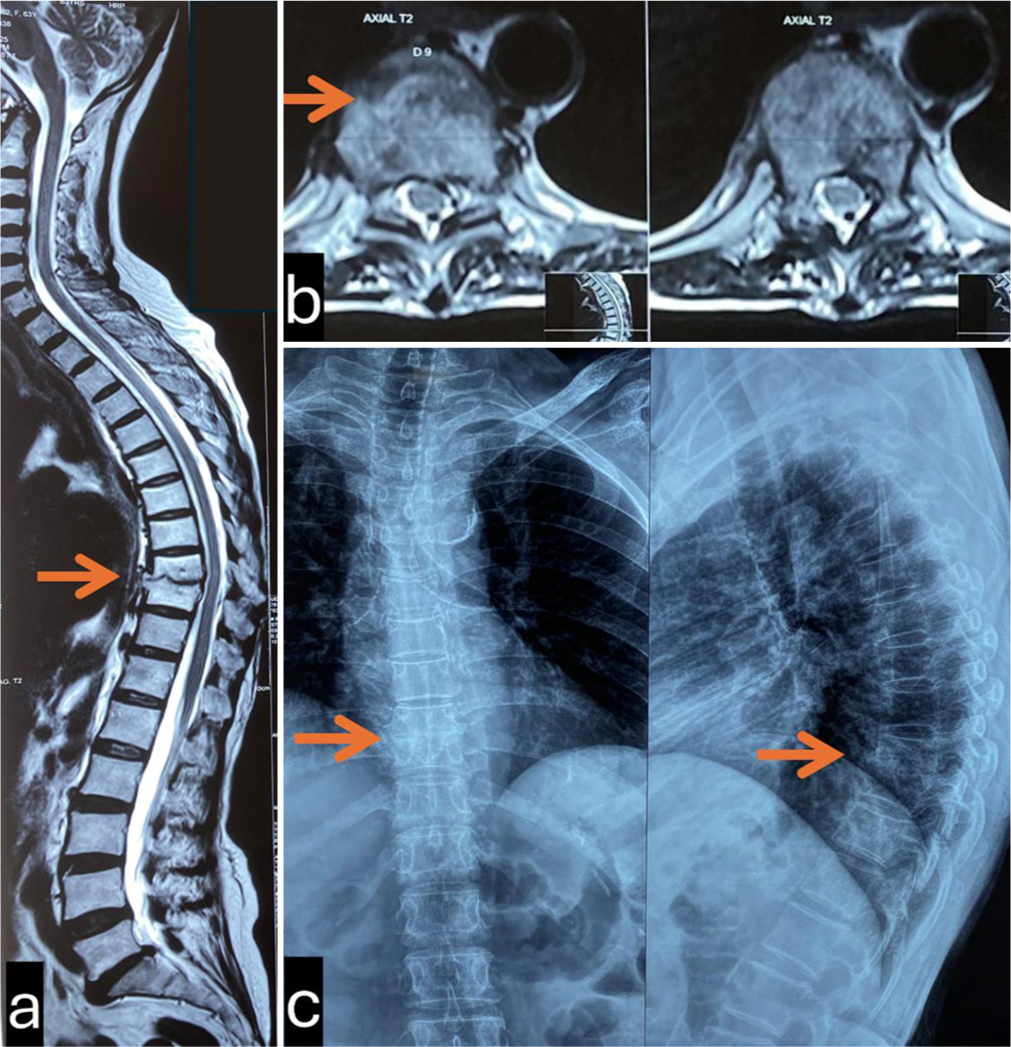
- Post-treatment radiological investigations, (a and b) MRI showing resolution of disease with healing at D9-D10 disc space, (c) X-ray showing vertebral body integrity being maintained.
DISCUSSION
Spondylodiscitis is a term describing three manifestations: Vertebral osteomyelitis, spondylitis, and discitis: All due to the same pathology. Salmonella infection is uncommon and is seen in patients with sickle cell disease or aortic mycotic aneurysms.[3] Salmonella spp. causing enteric diseases can manifest to become a multisystem disease but non-typhoidal Salmonella is mostly limited to gastrointestinal (GI) manifestations.[4-6] In this case, our patient had no history of any GI symptoms probably because of the self-containing nature, back pain was the only presenting symptom which was not associated with fever.
In the vertebral column, the discs are avascular and the anastomoses within the bone shrink, leading to end arteries, and no collateral circulation. This may result in osseous infarcts due to a septic embolus as there is not enough blood to contain the infection.[3] In immunocompromised states such as DM, there could be increased compromise to the vascularity which could have been so in this case.
Clinically, SD is very non-specific, which could be due to several etiologies due to which diagnosis could be delayed as seen in this patient.[4] Cases are treated with empirical antibiotics and antimycobacterial drugs.[5,7,8] Antimicrobial resistance is a hurdle. A study revealed that non-Salmonella typhi species have high resistance to ceftriaxone.[9] Confirmatory diagnosis can only be made through microbiological workup.
It is interesting to note that since she was a regular consumer of fish. Studies have shown that Salmonella grows extensively on seafood and depending on temperature, expresses certain risk factors.[10]
CONCLUSION
We must consider infectious etiology for spondylodiscitis in elderly patients with back pain that is not due to a mechanical reason. It is also important to correlate radio-imaging with hematological picture. Any spondylodiscitis needs a whole spine screening and brain screening. Spondylodiscitis requires surgical intervention if there is structural instability or neurological involvement. Opinion of an Infectious Disease specialist may be sought as well.
Ethical approval:
The research/study was approved by the Institutional Review Board at Kasturba Medical College, Mangalore, Manipal Academy of Higher Education, Manipal, Karnataka, India, number IEC KMC MLR 09-2024-566, dated September 18, 2024.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Salmonellosis nontyphoidal. 2024. CDC Yellow book. Available from: https://wwwnc.cdc.gov/travel/yellowbook/2024/infections-diseases/salmonellosis-nontyphoidal#:~:text=epidemiology [Last accessed on 2025 Feb 18]
- [Google Scholar]
- Spondylodiscitis: Update on diagnosis and management. J Antimicrob Chemother. 2010;65:iii11-24.
- [CrossRef] [PubMed] [Google Scholar]
- An atypical case of spondylitis due to nontyphoidal Salmonella in an adult patient: A case report and review of the literature. Cureus. 2024;16:e55034.
- [CrossRef] [Google Scholar]
- Case report of infective spondylodiscitis due to nalidixic acid-resistant Salmonella paratyphi A. J Family Med Prim Care. 2021;10:554-7.
- [CrossRef] [PubMed] [Google Scholar]
- Disseminated non typhoidal Salmonella infection with Salmonella pneumonia and vertebral osteomyelitis in sickle cell disease: A case report. IDCases. 2022;27:e01390.
- [CrossRef] [PubMed] [Google Scholar]
- Spondylodiscitis due to Salmonella Typhi: A series of four cases. Oxf Med Case Reports. 2021;2021:omab128.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical-microbiological study of nontyphoidal Salmonella infections from Karnataka, India. Scientifica (Cairo). 2024;2024:6620871.
- [CrossRef] [PubMed] [Google Scholar]
- Salmonella grows vigorously on seafood and expresses its virulence and stress genes at different temperature exposure. BMC Microbiol. 2015;15:254.
- [CrossRef] [PubMed] [Google Scholar]







