Translate this page into:
Cytotoxic lesion of corpus callosum secondary to phenytoin toxicity
*Corresponding author: Amrita Gotur, Department of Neurology, Shanti Mukund Hospital, Delhi, India. amrita.gotur@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sahib A, Gotur A. Cytotoxic lesion of corpus callosum secondary to phenytoin toxicity. J Neurosci Rural Pract. 2024;15:148-9. doi: 10.25259/JNRP_468_2023
Dear Editor,
A 27-year-old male presented with tremulousness of both upper limbs and imbalance while walking for 10 days. He had a history of left temporal arteriovenous malformation for which he underwent gamma knife surgery 18 years back and was on antiseizure medications (ASMs). One year back, his ASM was changed to phenytoin at a dose of 350 mg. Neurological examination revealed bilateral upper limb intentional tremors, bilateral horizontal gaze-evoked nystagmus, incoordination on finger nose test, impaired heel shin test, and perioral dyskinetic movements along with gait ataxia. Magnetic resonance imaging (MRI) brain with contrast revealed a small round lesion in the splenium of the corpus callosum which was hyperintense on T2 and fluid-attenuated inversion recovery sequences with diffusion restriction and no post-contrast enhancement [Figure 1]. The electroencephalogram was normal while Vitamin B12, B1, and B6 levels were in the normal range. Serum phenytoin levels were 43 mcg/mL (range 10–20 mcg/mL). He was diagnosed as a case of cytotoxic lesion of the corpus callosum secondary to phenytoin toxicity. He was managed with intravenous fluids, thiamine, and changing phenytoin to levetiracetam. There was significant improvement in his symptoms and a repeat MRI brain after 1 month showed resolution of the splenial lesion [Figure 2].

- Magnetic resonance imaging (MRI) brain at presentation: An oval T2 and fluid-attenuated inversion recovery (a and b) hyperintense lesion is noted in the center of the corpus callosum which shows diffusion restriction (c) which is dark on apparent diffusion coefficient (not shown) and no contrast enhancement (d) in axial MRI brain.
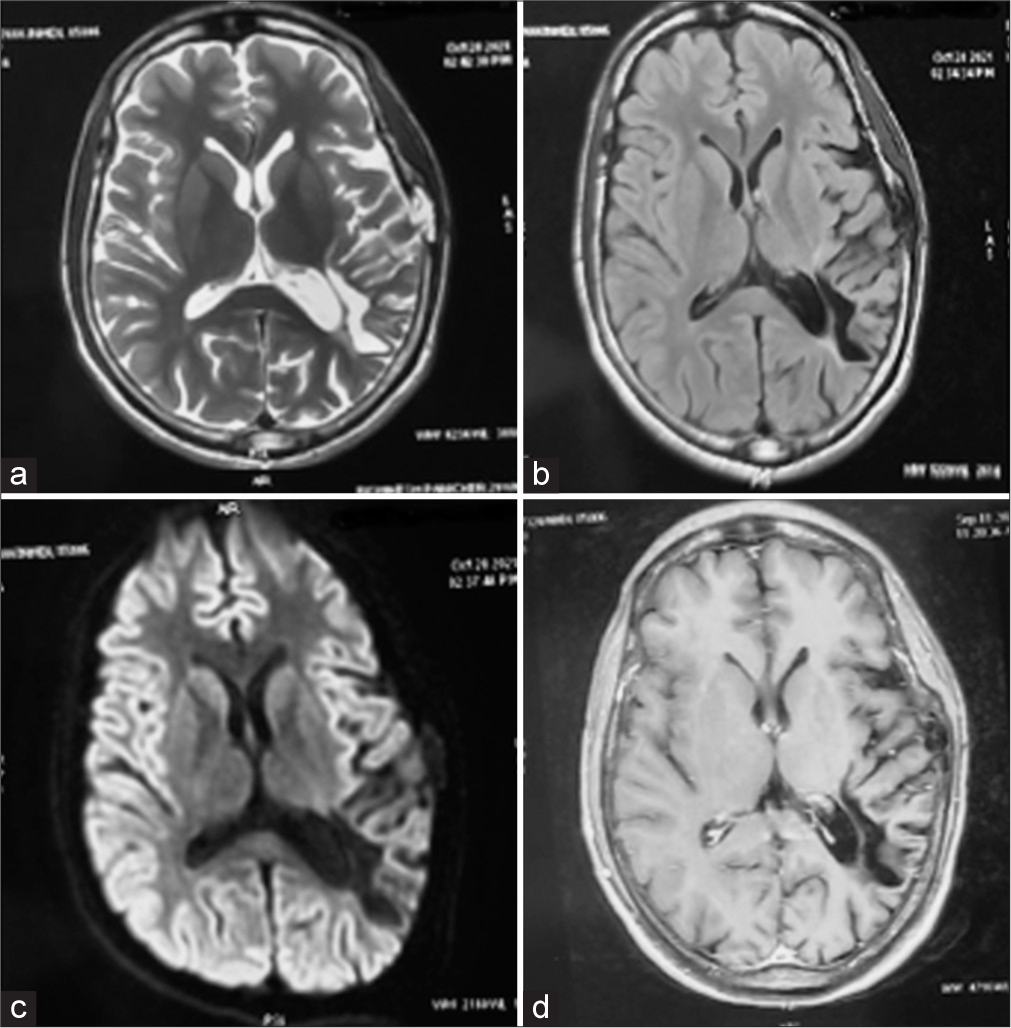
- Follow-up magnetic resonance imaging (a-d) done 1 month later shows disappearance of the lesion.
A localized discrete lesion within the center of the splenium of the corpus callosum without associated lesions is rarely encountered in a clinical setting. Various causes associated with such lesion include drugs such as metronidazole, infections (influenza-associated encephalitis, Escherichia coli-associated hemolytic uremic syndrome, and rotavirus encephalopathy), metabolic disorders (Marchiafava– Bignami disease, Wernickes encephalopathy, osmotic demyelination syndrome, and Wilsons disease), tumor (central nervous system malignancy or history of chemotherapy), and rarely can be subarachnoid hemorrhage associated.[1] In addition to the above causes, cytotoxic lesions in the splenium of the corpus callosum can occur very rarely due to seizures, ASM toxicity, or its withdrawal.[2] Duberkar and Jawale reported a similar finding in a patient with abrupt phenytoin withdrawal.[3] There was no history of seizure either clinically or electrographically in our patient; serum phenytoin level was elevated in our patient and the lesion disappeared after withdrawal of phenytoin. These facts suggest that the lesion was possibly caused by the administration of phenytoin either in response to higher doses or drug sensitivity.
The exact mechanism involved is not yet completely understood. Kim et al.[4] hypothesized that ASM toxicity can cause transient demyelination of the splenium of corpus callosum whereas Polster et al. postulated that rapid changes in ASM levels might disturb the arginine-vasopressin physiology leading to dysfunction in fluid balance resulting in an abnormally high water content in the focal area.[5] To conclude, a focal lesion in the splenium of the corpus callosum may be seen on MRI images of patients with epilepsy. This lesion might be due to epileptic activity or ASM toxicity leading to focal demyelination or vasogenic edema in the splenium of the corpus callosum. This condition must be promptly recognized to avoid misdiagnosis and unnecessary procedures.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Cytotoxic lesions of the corpus callosum that show restricted diffusion: mechanisms, causes, and manifestations. Radiographics. 2017;37:562-76.
- [CrossRef] [PubMed] [Google Scholar]
- Focal transient lesion in the splenium of the corpus callosum in three non-epileptic patients. Neuroradiology. 2006;48:731-5.
- [CrossRef] [PubMed] [Google Scholar]
- Transient lesion in the splenium of corpus callosum due to abrupt phenytoin withdrawal. Neurol India. 2017;65:S104.
- [Google Scholar]
- Focal lesion in the splenium of the corpus callosum in epileptic patients: Antiepileptic drug toxicity? Am J Neuroradiol. 1999;20:125-9.
- [Google Scholar]
- Transient lesion in the splenium of the corpus callosum: Three further cases in epileptic patients and a pathophysiological hypothesis. J Neurol Neurosurg Psychiatry. 2001;70:459-63.
- [CrossRef] [PubMed] [Google Scholar]






