Translate this page into:
A cadaveric observation of infraorbital and accessory infraorbital foramen in the Indian population
*Corresponding author: J. P. Femina Sam, Department of Anatomy, Christian Medical College, Vellore, Tamil Nadu, India. feminanegine@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Rout S, Femina Sam JP, Prasad M. A cadaveric observation of infraorbital and accessory infraorbital foramen in the Indian population. J Neurosci Rural Pract. doi: 10.25259/JNRP_316_2023
Abstract
Objectives:
The knowledge of the location of the infraorbital foramen (IOF) is crucial in the management of maxillofacial surgeries. The morphology of this foramen is variable in different populations. The purpose of this study is to locate the IOF and to determine the frequency and location of accessory IOF (AIOF) in the Indian population.
Materials and Methods:
The study was conducted after getting ethical approval from the institutional review board. It was done on the 60 hemi faces of formalin embalmed heads of 30 cadavers. A modified Weber–Fergusson’s incision was made to expose the anterior surface of the maxilla and the distance of IOF from the root of PM2 teeth and the infraorbital rim (IOR) was measured. The occurrence of AIOF was noted and the neurovascular structures passing through were traced. The distance of the AIOF from the IOF was measured and the statistical analysis was done.
Results:
The mean distance of the IOF to the IOR on the right side was 6.96 ± 1.79 mm and on the left side was 7.24 ± 1.84 mm. The mean distance of the IOF from the upper PM2 on the right side was 27.11 ± 5.16 mm and on the left side was 26.71 ± 5 mm. The AIOF was present in 10 % of the cadavers dissected and supero-medial in position. It may be single or double, transmitting blood vessels and nerves. The mean distance between the IOF to the AIOF was 9.92 mm on the right and 5.87 mm on the left.
Conclusion:
Until now, no studies have been conducted on human cadavers to determine if any neurovascular structures pass through AIOF in Indian populations. This human cadaveric study will give additional information to the clinicians that a considerable number of patients may have AIOF and they may transmit neurovascular structures, the knowledge of this is needed to avoid unexpected complications during surgical procedures and nerve block.
Keywords
Accessory infraorbital nerves
Accessory infraorbital arteries
Facial
Maxillofacial
Maxilla
INTRODUCTION
Recognition of the infraorbital foramen (IOF) is central in the treatment of injuries related to the maxillofacial region as well as in facial plastic surgery, and providing anesthesia in the orofacial region, or any repair during Le Fort’s osteotomies. The location of the IOF, as per the description of the traditional textbooks, is on the anterior surface of the maxilla, and it constantly transmits the infraorbital vessels and nerves. The ION continues downward and emerges on the facial region and it supplies the skin of the region surrounding it, that is, lower eyelid, conjunctiva, lateral surface of nose, and upper lip.[1] The morphology and the morphometry of the infraorbital foramen has been extensively studied by a lot of authors in different ethnic races in human skeletons using different bony (predominantly) as well as soft tissue landmarks.[2-9] This nerve is commonly blocked at the foramen to induce local anesthesia. The infraorbital vessels and nerve undergo division anywhere from the level of the inferior orbital fissure to the area of emergence from the IOF.[10] The morphometry of the IOF and the occurrence of accessory IOF (AIOF) has been reported in the literature using human skeletons.[2,9-12] Hu et al., in 2016, described the branching pattern of infraorbital nerves in relation to the infraorbital artery in human cadavers in the Korean population.[11] There are no previous reports on the details of the neurovascular structure traversing the foramen in the Indian population. Thus, essential topographical knowledge of IOF and the structures passing through is needed to avoid injuries to the neurovascular bundle and reduce postoperative complications. Hence, this cadaveric study aimed to find the location of IOF and to verify the frequency and location of AIOF and the structures passing through it in the South Indian population.
MATERIALS AND METHODS
The authors embarked on this research project with the approval of the institutional review board (IRB Min. No. 12085 dated 26-06-2019) and the study was conducted over 2 years. The specimens needed for this study were obtained from human cadavers who were donated to the department through the institution’s body donation program after fulfilling the requisite ethical guidelines. These cadavers were obtained after getting informed consent from the relatives while donating, to be used for the purpose of teaching and research.
Before starting the main study, a pilot study was done in twenty hemifaces to determine the frequency of the location of the IOF with respect to the premolar tooth. This was done to determine which premolar tooth is related to the IOF, as studies have mentioned different reference points. Once the reference point was obtained from the pilot study, the main study was started on the 60 hemifaces of formalin embalmed heads of 30 cadavers with no visible external abnormalities such as edentulous teeth or any fractures of the facial skeleton. The age of the cadavers was between 25 and 95 years.
Bilateral Weber–Fergusson’s incision (Dieffenbach’s modification) was made on each side of the face to expose the anterior surface of the maxilla from the inferior orbital rim to the alveolar ridge and then to the zygoma [Figure 1a].[13,14] The skin and the superficial fascia were reflected in the area between the orbital rim and the labiogingival sulcus vertically and the ala of the nose to the zygomatic arch horizontally. The orbital fibers of the orbicularis oculi superiorly, nasalis medially, and the zygomaticus minor infero-laterally form the triangular space where the IOF is found [Figure 1b]. The muscles near the IOF were reflected and the IOF was seen below the infraorbital rim (IOR) by reflecting the levator labii superioris muscle originating from the IOR. The periosteum of the IOR was lifted and resected. The IOF was seen, and the contents were dissected. The infraorbital nerves and vessels passing out through the foramen were carefully traced. The presence of AIOF and the presence of any structures in the AIOF were noted.
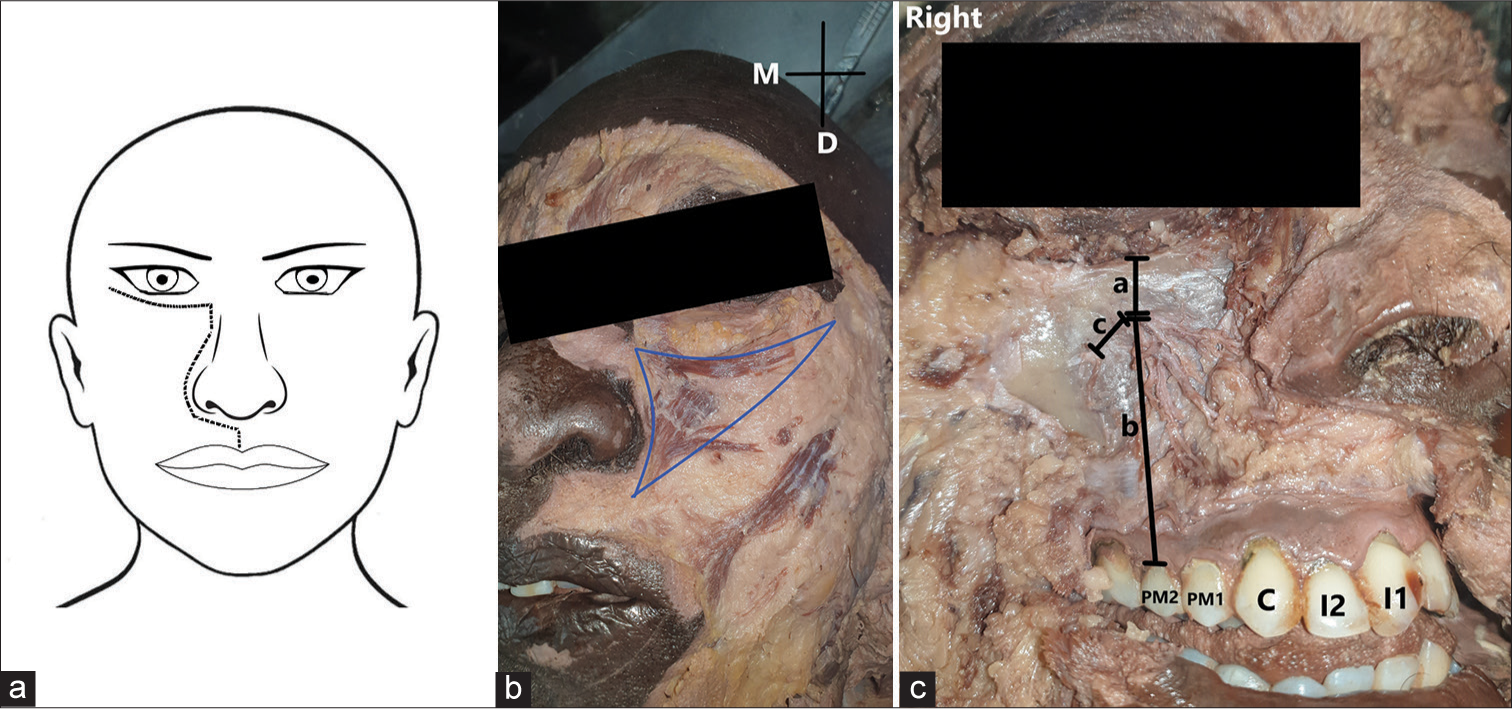
- (a) The Dieffenbach’s modification of Weber–Fergusson’s incision made on the side of the face from the inferior orbital rim to the alveolar ridge and then to the zygoma to expose the anterior surface of maxilla. (b) The triangular space bounded by the orbital fibers of the orbicularis oculi superiorly, nasalis medially and the zygomaticus minor infero-laterally where the infraorbital foramen is located. (c) The right hemiface of a cadaver shows the morphometric measurements. a-distance of the infraorbital foramen from the infraorbital rim, b-distance between the infraorbital foramen and the second premolar tooth, and c-distance between the infraorbital foramen and the accessory infraorbital foramen. (I1: Incisor 1, I2: Incisior 2, C: Canine, PM1: Premolar tooth 1, PM2: Premolar tooth 2).
As the IOF is commonly found in a vertical line from the second premolar teeth (right – 85% and left – 90%), the root of the second premolar teeth was marked after reflecting a few fibers of orbicularis oris. This finding was on par with the findings by Aggarwal et al., wherein more than half of the specimens, the IOF was laid aligned with the upper second maxillary premolar tooth.[15] Hence, we sought to measure the distance of IOF from the root of the second premolar teeth using an Vernier caliper with an accuracy of 0.001 mm. The distance of the infraorbital margin to the IOF was also measured. The distance of AIOF from the IOF was measured if it was present and the structures passing through it, was also noted [Figure 1c].
All the measurements were made to the nearest millimeter, and tabulated, and the quantitative data were analyzed using SPSS software. The comparison of distances related to IOF and AIOF between the right and left sides was done using a paired t-test. The mean, standard deviation, and the P-value of each were calculated.
RESULTS
In the current study, the main trunk of the infraorbital vessels and nerves was not seen emerging from the foramen, as it would have divided before reaching the IOF, and the divisions of those were found to emerge from the foramen. A few of the branches were found emerging through the AIOF. In contrast to our prior knowledge and the traditional description of the branching pattern given in textbooks, the branches of the ION were intertwined with the branches of infraorbital vessels [Figure 2] and the branching system could not be made out.
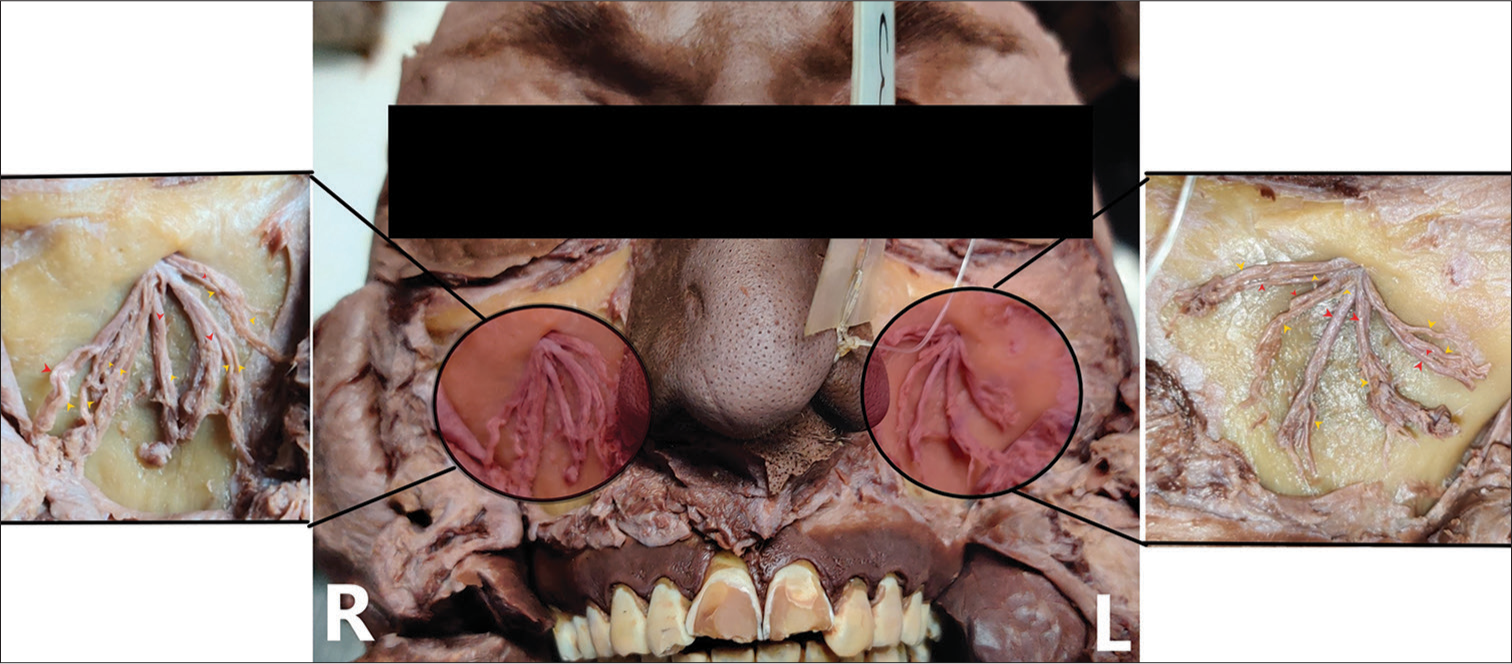
- Dissected face of a cadaver showing the branches of the infraorbital nerves jumbled with the branches of infraorbital vessels emerging out from the infraorbital foramen. (Inset showing the larger version of the structures emerging out from each infraorbital foramen, red arrowheads denote the branches of the infraorbital vessels, and the yellow arrowheads denote the branches of infraorbital nerves).
Morphometric measurements of the IOF from the IOR and the second premolar tooth were taken. The mean distance of the IOF to the IOR on the right side was 6.96 ± 1.79 mm (Range: 3.73 mm–9.66 mm). Similarly, on the left side, it was 7.24 ± 1.84 mm (Range: 4.03 mm–10.71 mm). The mean distance of the IOF from the upper second premolar tooth on the right side was 27.11 ± 5.16 mm and it ranged from 16.70 mm to 36.19 mm. Similarly, on the left side, it was 26.71 ± 5 mm and it ranged from 16.83 mm to 34.34 mm. There was no statistical difference between the right and left sides [Table 1a].
| Distances (mm) | Right (n=30) | Left (n=30) | P value | ||
|---|---|---|---|---|---|
| Mean+SD (in mm) | Range (in mm) | Mean+SD (in mm) | Range (in mm) | ||
| IOF to PM2 | 27.11±5.16 | 36.19-16.7 | 26.71+5 | 16.83-34.34 | 0.23 |
| IOF to IOR | 6.96±1.79 | 3.73-9.66 | 7.24+1.84 | 4.03-10.71 | 0.14 |
In a total of the 30 cadavers (60 hemifaces) studied, AIOF was observed in 10% (6/60), of which there was no significant difference between the sides. They were positioned infero-lateral in 3.3% (2/60) [Figure 3a] and supero-medial in 5.5% (4/60) with respect to the IOF [Figure 3b]. The average distance from the IOF to the AIOF was 9.92 mm on the right and 5.87 mm on the left [Table 1b]. The number of AIOF varied from single to double. In the present study, a single AIOF was reported in 5.5% (4/60) [Figure 4a], while double AIOF were seen in 3.3% (2/60) [Figure 4b]. The AIOF foramina are occasionally transmitted to nerves, arteries, or veins. In one of the cadavers with double AIOF, one of the AIOF transmitted a vein, and the other transmitted a nerve [Figure 4b]. In another hemiface, two accessory infraorbital arteries and two accessory infraorbital nerves were appearing from the AIOF [Figure 4c].
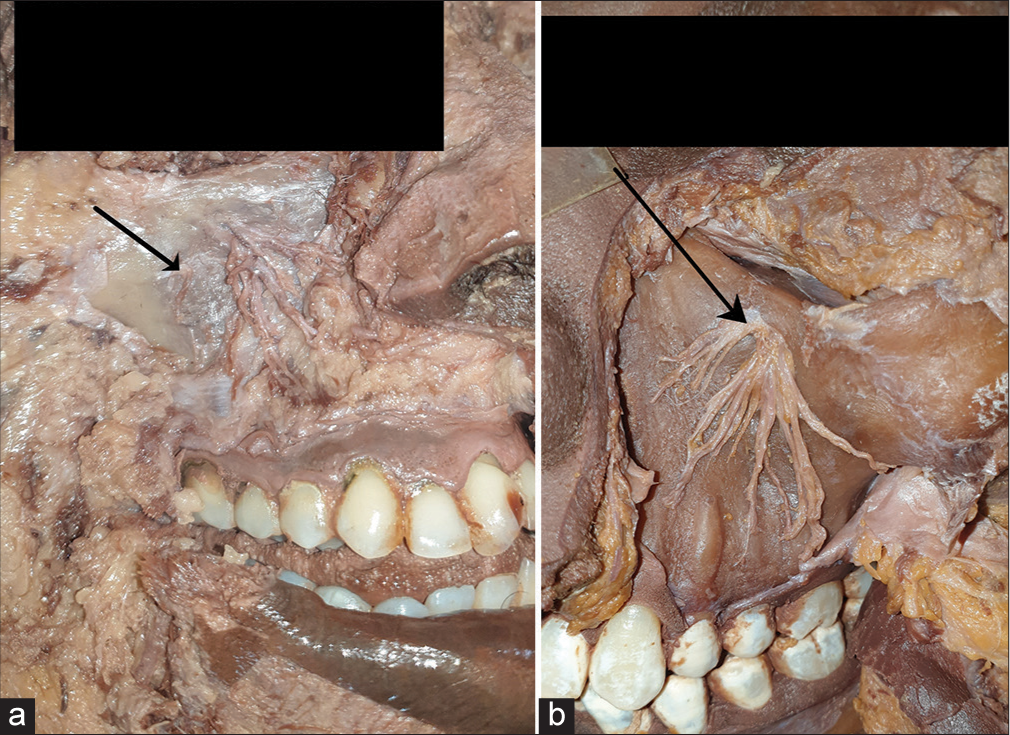
- (a) The right hemiface of a cadaver showing the accessory infraorbital foramen positioned inferolateral (depicted in a black arrow) with respect to the infraorbital foramen. (b) The left hemiface of a cadaver showing the accessory infraorbital foramen positioned superomedial (depicted in a black arrow) with respect to the infraorbital foramen.
| Variable | Number of skulls with AIOF (6) | Position of the AIOF in relation to IOF | Distance between the IOF and AIOF (mean in mm) | |
|---|---|---|---|---|
| Supero- medial | Infero- lateral | |||
| Right | 10 (%) | 7.5% | 2.5% | 9.92 |
| Left | 10 (%) | 7.5% | 2.5% | 5.87 |
AIOF: Accessory infraorbital foramen, IOF: Infraorbital foramen. All measurements are in millimeters.

- (a) The right hemiface of a cadaver shows the presence of a single accessory infraorbital foramen (depicted in a black arrow). (b) The right hemiface of a cadaver shows the presence of double accessory infraorbital foramen, one of which transmits a vein (represented by a blue arrowhead) and the other transmits a nerve (represented by a yellow arrowhead). (c) The left hemiface of a cadaver shows the presence of accessory infraorbital foramen (represented by a black arrow), one of which transmits two accessory infraorbital arteries (outlined in red color) and two accessory infraorbital nerves (outlined in yellow color).
DISCUSSION
The IOF present inferior to the infraorbital margin in the maxilla shows a lot of variability between different ethnicities. These differences may be due to racial changes.[10] The infraorbital nerve and vessels transmitting through this foramen, after externalizing out, the infraorbital nerve terminates in 5–11 terminal branches[16] and provides sensory innervation to a part of the facial region close to it.[17]
IOF is an essential marker to enable anesthetic and surgical interventions of the midface region.[18] An infraorbital nerve block is needed for techniques involving the region between the lower eyelid and upper lip and for dental procedures. It is carried out by injecting an anesthetic medicine around the IOF. This can be done either by an extraoral or an intraoral approach. The intraoral approach is done by injecting an anesthetic medium into the buccal mucosa opposite the upper second premolar tooth, approximately 0.5 cm from the buccal surface.[12] The extraoral approach involves injecting the drug into the tissues surrounding the IOF.[19] For both approaches, the surgeon must know the exact location of IOF in relation to IOR and the upper second premolar tooth. Hence, in this study, measurements of the IOF were taken from the IOR and the second premolar tooth, as both intraoral and extraoral approaches need these skeletal landmarks.
The comparison of the morphometric measurements of IOF between various ethnic groups was tabulated [Table 2a]. This study showed the vertical distance between the IOF and the PM2 as 27.11 mm and 26.71 mm on the right and left sides, respectively. The bony tooth landmarks differ in different ethnic races, that is, in the majority of the American population, the IOF lies in line with PM1, and in the Asian population, it lies commonly opposite to PM2. The Indian researchers have just reported how many percentages of cadavers with the IOF lying in line with the PM2, but not measured the distance of IOF from the second premolar.[20,21] As, in most of the Indian population, the IOF is in line with the PM2,[20,21] we sought to measure the distance of IOF to the PM2. There are no Indian studies to compare the distance of IOF to the PM2 described in the present study, except an American study by Masabni and Ahmad,[22] which has shown similarity to the present study as they have measured the distance of the IOF from the second premolar tooth. The study done by Masabni and Ahmad described the mean distance between IOF to the PM2 as 29.07 mm and 29.39 mm on the right and left sides, respectively.[22]
| Population | Author | IOF to the PM2(mm) | IOF to the IOR (mm) | ||
|---|---|---|---|---|---|
| Right | Left | Right | Left | ||
| Current study | 27.11 (36.19-16.7) | 26.71 (16.83-34.34) | 6.96 (3.73-9.66) | 7.24 (4.03-10.71) | |
| Indian | Aggarwal et al., 2015[15] | 6.37 (3.14-12.93) | 6.28 (3.14-12.93) | ||
| American | Masabni and Ahmad, 2017[22] | 29.07 (20.5-36.5) | 29.39 (21-36) | 6.46 (4-11) | 6.74 (3-12) |
| American | Aziz et al., 2000[18] | 8.3 (2.5-15) | 8.1 (2.5-15) | ||
| American | Raschke et al., 2013[29] | 41.81 in males and 37.33 in females | 8.61 in males and 8.25 in females | ||
| Turkey | Canon et al., 1999[30] | 7.0-9.7 | 6.8-9.8 | ||
| Poland | Przygocka et al., 2012[3] | 2.47±1.56 (males) | |||
| 1.76±1.48 (females) | |||||
| Indian | Potu et al., 2019[21) | 5.49 (3.29-7.59) | 5.85 (4.51-8.56) | ||
| Lebanese | Sokhn et al., 2019[10] | 7.94 (3.40-10.80) | 8.03 (4.50-11.20) | ||
AIOF: Accessory infraorbital foramen, IOF: Infraorbital foramen. All measurements are in millimeters.
Furthermore, the present study showed the distance between the IOF and the IOR as 6.96 mm, and 7.24 mm on the right and left sides, respectively. An Indian study done on skulls by Tewari et al. described the mean distance of IOF to the IOR to be 7.09 mm and 6.95 mm on the right and left sides, respectively.[20] and this distance is comparable to different population such as Americans, Indians, Poland, Turkey, and Lebanese, as cited in [Table 2a]. The mean distance of IOF to IOR is 6.37 mm and 6.28 mm on the right and left sides, respectively, in the Indian population,[15] 6.46 mm and 6.74 mm on the right and left sides, respectively, in the American population,[22] and 7.94 mm and 8.03 mm on the right and left sides, respectively, in the Lebanese population.[10] This measurement, that is, IOF to the IOR seems to be a reliable measurement to find the IOF. The distance of IOF from the upper second premolar tooth as well as the IOR between the right and left sides were not statistically significant in the present study.
A large deviation in the presence of AIOF among different populations has been reported.[3,9,23-26] A single IOF is exceptional to humans, and animals such as gorilla, pan, and pongo generally have 2–3 infraorbital foramina.[24] As reported by Leo et al., the earliest account of the presence of multiple AIOF was quoted by Gruber in 1875.[3] It was present frequently superomedial to the main IOF.[3,9] The knowledge about the accessory infraorbital foramen is essential as there is a constant rise in the popularity in the field of esthetic medicine especially, midface augmentation surgeries as well as the routine surgeries involving the external access of the maxillary air sinus in Caldwell Luc surgeries.[27-29] Canan et al. performed research on dry skulls and noted the presence of AIOF in 23.1%, Rai et al. recorded the presence of AIOF in 27.3% of dry skulls and Ali et al. reported the AIOF in 29% by cone-beam computed tomography (CT) scans.[11,12,30] The frequency of AIOF varied according to different demographic areas and found significant differences.[12] In this study, single or two AIOF were noted in 20% of hemifaces dissected, and they were predominantly supero-medial to the IOF. The mean distance between the IOF and the AIOF is 9.92 mm and 5.87 mm on the right and left side, respectively, with a range of 2.67–15.57 mm, which is comparable with the other Indian study by Ali et al., who had reported the distance to be 9.60 mm and 9.98 mm on the right and left sides, respectively,[12] and Rai et al., who reported this distance in 65 skulls as 9.6 mm and 10 mm on right and left, respectively.[11] Nevertheless, it varied with different ethnic groups. Bressan et al., in the Italian population, reported the distance of IOF to AIOF to be in a vast range of 2–15 mm.[31] Canon et al. described the distance of IOF and the AIOF to be in a range of 1–12 mm with a mean of 7 mm.[30] The comparison of the mean distance between the AIOF and the IOF with the other population was tabulated [Table 2b].
| Population | Author | Number of skulls | AIOF-IOF (mm) | |
|---|---|---|---|---|
| Right | Left | |||
| Current study | 30 | 9.92 (3.52-10.96) | 5.87 (2.67-15.57) | |
| Indian | Ali et al., 2017[12] | 200 | 9.60 (1.16-13.73) | 9.98 (6.19-12.06) |
| Turkey | Canon et al., 1999[30] | 348 | 7 (1-12) | |
| Italy | Bressan et al., 2004[31] | 1068 | 2-15 | |
| Indian | Rai et al., 2013[11] | 65 | 9.6 (1.2-13.7) | 10 (6.2-12.1) |
| Switzerland | Polo et al., 2019[9] | 30 | 11.47 (2.69-19.59) | 12.06 (3.76-18.69) |
AIOF: Accessory infraorbital foramen, IOF: Infraorbital foramen. All measurements are in millimeters.
The occurrence of AIOF and the presence of neural contents have clinical consequences like difficult or failed regional anesthesia and the risk of nerve damage during any interventions in the maxillary region.[9] Most of the studies have mentioned the presence of accessory infraorbital nerves or bifid ION through the AIOF.[23,24,26] In this study, a vein and an artery were seen passing through an accessory foramen. The arteries in the AIOF can be one of the branches of infraorbital arteries. The vascular injury following unintentional intra-arterial injection may induce adverse events from a range of erythema to skin necrosis. There are a few case reports of visual impairment and cerebral infarction during infraorbital enhancement injections.[27]
No other research work has been conducted in human cadavers to notify the structures passing through the AIOF in the South Indian population. This knowledge is of high priority for the surgeon doing procedures in the facial region to evade injury to the duplicated infraorbital nerve or a blood vessel and also to gain adequate local anesthesia.[23] The IOF is a constant reference point in orbital surgeries as well as to locate and gain entry to the maxillary sinus.[28] Moreover, an understanding of the anatomical location of the IOF and AIOF is important as there is a constant rise of endoscopic procedures, and the bony landmarks used in this study are applicable to the CT images.
A few numbers of patients may feel sensation even after giving an ION block, this may be associated with the presence of AIOF which may be transmitting a branch of the infraorbital nerve, and the surgeon should consider an added injection into AIOF to achieve a proper anesthetic effect.
There are a few limitations in this study. As the availability of the cadavers was constrained, this study was done on a small sample size of 30 cadavers. The authors could not trace the entire course of the nerves and the vessels passing through the foramen, as the cadavers were embalmed and preserved in a conventional formalin-based solution. This issue could be rectified hopefully by using fresh frozen cadavers and by making hemi-sections of the heads. The gender details of the cadavers were not available; hence, the impact of sex on the measurements related to the IOF could not be assessed.
CONCLUSION
Though several osteology studies on the prevalence of accessory infraorbital foramen are there, corroborating the same with structures passing through will give additional information to the clinicians during surgical procedures and nerve block. This is the first study to notify the structures emerging out of the AIOF, the knowledge of which is certainly used to evade complications during the surgery.
Acknowledgments
The authors would like to acknowledge the IRB for having approved and funded the study; the human cadaveric donors and their families for donating the human bodies toward research and academic purposes; the non-teaching faculty of the department of anatomy who have helped with the maintenance of the cadavers.
Ethical approval
The author(s) declare that they have taken the ethical approval from IRB.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Fluid research fund of the institution.
References
- Anthropometric analysis of the infraorbital foramen in a South Indian population. Singapore Med J. 2010;51:730-5.
- [Google Scholar]
- Anatomic study of accessory infraorbital nerves and foramina: Application for a better understanding of complications of Le Fort fractures and osteotomy. J Oral Maxillofac Surg. 2020;78:717-23.
- [CrossRef] [PubMed] [Google Scholar]
- Variation in human infraorbital nerve, canal and foramen. Ann Anat. 1995;177:93-5.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomy of infraorbital foramen: Influence of sex, side, and cranium size. J Craniofac Surg. 2019;30:1284-8.
- [CrossRef] [PubMed] [Google Scholar]
- Anthropometric analysis of infraorbital foramen in adult Indian dry skull. J Health Allied Sci NU. 2016;6:27-30.
- [CrossRef] [Google Scholar]
- Infraorbital foramen: Horizontal location in relation to ala nasi. Ophthalmic Plast Reconstr Surg. 2011;27:295-7.
- [CrossRef] [PubMed] [Google Scholar]
- Location of the infraorbital foramen with reference to soft tissue landmarks. Surg Radiol Anat. 2017;39:11-5.
- [CrossRef] [PubMed] [Google Scholar]
- The location of the infraorbital foramen in human skulls, to be used as new anthropometric landmarks as a useful method for maxillofacial surgery. Folia Morphol (Warsz). 2012;71:198-204.
- [Google Scholar]
- The morphology of the infraorbital nerve and foramen in the presence of an accessory infraorbital foramen. J Craniofac Surg. 2019;30:244-53.
- [CrossRef] [PubMed] [Google Scholar]
- The infraorbital foramen in a sample of the Lebanese population: A radiographic study. Cureus. 2019;11:e6381.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomical and morphometric analysis of accessory infraorbital foramen. J Craniofac Surg. 2013;24:2124-6.
- [CrossRef] [PubMed] [Google Scholar]
- Cone beam computed tomography assessment of accessory infraorbital foramen and determination of infraorbital foramen position. J Craniofac Surg. 2018;29:e124-6.
- [CrossRef] [PubMed] [Google Scholar]
- Versatility of Dieffenbach's modification of Weber Fergusson's approach for treatment of maxillary pathologies. J Maxillofac Oral Surg. 2012;11:416-9.
- [CrossRef] [PubMed] [Google Scholar]
- Recurrent unicystic maxillary ameloblastoma presenting as unilateral proptosis. Saudi J Ophthalmol. 2018;33:94-8.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomical study of the infraorbital foramen: A basis for successful infraorbital nerve block. Clin Anat. 2015;28:753-60.
- [CrossRef] [PubMed] [Google Scholar]
- Infraorbital nerve: A surgically relevant landmark for the pterygopalatine fossa, cavernous sinus, and anterolateral skull base in endoscopic transmaxillary approaches. J Neurosurg. 2016;125:1460-8.
- [CrossRef] [PubMed] [Google Scholar]
- Branching patterns of the infraorbital nerve and topography within the infraorbital space. J Craniofac Surg. 2006;17:1111-5.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomic characteristics of the infraorbital foramen: A Cadaver study. J Oral Maxillofac Surg. 2000;58:992-6.
- [CrossRef] [PubMed] [Google Scholar]
- Infraorbital nerve block In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499881 [Last accessed on 2023 Aug 08]
- [Google Scholar]
- Morphometric analysis of infraorbital foramen in South Indian dry skulls. Bangladesh J Med Sci. 2018;17:562.
- [CrossRef] [Google Scholar]
- Morphometric evaluation of the infraorbital foramen in human dry skulls of South Indian population. Ital J Anat Embryol. 2019;124:382-91.
- [Google Scholar]
- Infraorbital foramen and pterygopalatine fossa location in dry skulls: Anatomical guidelines for local anesthesia. Anat Res Int. 2017;2017:1403120.
- [CrossRef] [PubMed] [Google Scholar]
- Morphometric analysis of the infraorbital foramen: The clinical relevance. Anat Res Int. 2016;2016:7917343.
- [CrossRef] [PubMed] [Google Scholar]
- A variation of the infraorbital nerve: its potential clinical consequence especially in the treatment of trigeminal neuralgia: Case report. Neurosurgery. 2010;67(3 Suppl):Operative:onsE315. discussion onsE315
- [CrossRef] [PubMed] [Google Scholar]
- Anatomy and clinical significance of the maxillary nerve: A literature review. Folia Morphol (Warsz). 2015;74:150-6.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomic study of accessory infraorbital nerves and foramina: Application for a better understanding of complications of le fort fractures and osteotomy. J Oral Maxillofac Surg. 2020;78:717-23.
- [CrossRef] [PubMed] [Google Scholar]
- The infraorbital artery: Clinical relevance in esthetic medicine and identification of danger zones of the midface. J Plast Reconstr Aesthet Surg. 2019;72:131-6.
- [CrossRef] [PubMed] [Google Scholar]
- The foramen and infraorbital nerve relating to the surgery for external access to the maxillary sinus (Caldwell-Luc) Int Arch Otorhinolarnygol. 2008;12:342-6.
- [Google Scholar]
- Identifying a safe zone for midface augmentation using anatomic landmarks for the infraorbital foramen. Aesthet Surg J. 2013;33:13-8.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomic variations of the infraorbital foramen. Ann Plast Surg. 1999;43:613-7.
- [CrossRef] [PubMed] [Google Scholar]
- Descriptive and topographic anatomy of the accessory infraorbital foramen. Clinical implications in maxillary surgery. Minerva Stomatol. 2004;53:495-505.
- [Google Scholar]







