Translate this page into:
Measuring preparedness of hospitals to manage traumatic brain injuries: Criterion development and assessment in an Indian district
-
Received: ,
Accepted: ,
How to cite this article: Adusumilli A, Sukumar GM, Pandey G, Shukla D. Measuring preparedness of hospitals to manage traumatic brain injuries: Criterion development and assessment in an Indian district. J Neurosci Rural Pract. doi: 10.25259/JNRP_461_2023
Abstract
Objectives:
The objectives of the study are to develop a criterion to objectively assess the preparedness of hospitals to manage traumatic brain injuries (TBIs) and to assess and classify the preparedness of secondary and tertiary care hospitals to manage TBIs in an Indian district.
Materials and Methods:
This ethically approved hospital-based cross-sectional study was conducted between June 2022 and February 2023 in all eligible secondary and tertiary hospitals in Kolar, Karnataka, India. A study instrument (Form 1, 2, and 3) and the criterion (level-numeric scoring system) to objectively measure the preparedness of hospitals to manage TBIs were developed based on the Neurotrauma Society of India guidelines. This was used to collect data on facilities, manpower, intensive care unit care, drugs, and equipment available for managing TBI in hospitals, by a combination of observation, interview, and verification of records. Based on the assessment, the preparedness of each hospital was categorized into different levels and scores.
Results:
We assessed all 11 eligible hospitals in the district of which 81% are categorized as having Level 4 preparedness to manage TBIs (corresponds to the management of mild head injury cases). One hospital each had Level 2 and Level 3 preparedness to manage TBIs (moderate and severe). There was no Level 1 preparedness in hospital in the district.
Conclusion:
Most hospitals were identified to have Level 4 preparedness, indicating a need for comprehensive strengthening of secondary and tertiary hospitals to manage TBI cases in the district.
Keywords
Traumatic brain injury
Preparedness assessment
Healthcare facilities
Hospitals
Scoring system
India
INTRODUCTION
Traumatic brain injury (TBI) is an injury to the brain caused by an external force that affects the functioning and structure of the brain.[1] The reported prevalence of TBI cases is 920/100,000 population[2] and TBIs account for nearly 1.6 million hospital admissions every year in India.[3] The crude DALY rate due to TBI increased by 55% in India, between 1990 and 2019.[4]
Road traffic injuries account for nearly 60% of TBIs[5,6] and this is expected to increase due to a rise in vulnerable road users, road infrastructure growth, and low helmet use rates necessitating improved hospital trauma care systems prepared to manage TBIs.
Adequate preparedness and effective management of TBI patients at the site of trauma, in transit, and in definitive hospitals are vital to reduce fatal outcomes of TBIs. Efficient management of TBIs could reduce 25–30% of TBI deaths in the hospital, indicating a need for well-prepared and efficient hospital systems to provide quality TBI care. Understanding the preparedness of these hospitals to manage TBI is important to strengthen TBI care in India.
An estimated 69000 public and private hospitals were recorded across India in the year 2019, of which nearly 63% are in the private sector.[7] Critically ill patients frequently overburden the health-care industry in India because there are fewer than 200 operational trauma centers for more than 120 crore people.[8] Although TBIs are reported by urban and rural populations, TBI care in India is private-sector dominant, urban-oriented, and extremely variable across hospitals due to a lack of uniform guidelines, diagnostic facilities, specialist human resources, drugs, and equipment. Thus, there is a need for systems development in all hospitals (urban and rural, public and private).
The Neurotrauma Society of India (NTSI) is a professional body of neurosurgeons which recently developed and released guidelines for TBI management called “National Guidelines for the Management of Traumatic Brain Injury” for the Indian context. The purpose of these guidelines is to standardize and improve TBI care starting from pre-hospital care, in-hospital care, and rehabilitation care.[9]
In line with NTSI guidelines, the authors developed a criterion to objectively measure hospital-level preparedness to manage TBI, for the Indian context. The present study was conducted to measure hospital-level preparedness to manage TBI cases in secondary and tertiary-level hospitals in Kolar, Karnataka, India. The results of this study would help to refine the methods and tools for replicating assessments across the states and countries.
MATERIALS AND METHODS
This cross-sectional study was conducted in the Kolar district situated 65 km from the Karnataka state capital, Bengaluru. The district has a population of 1.5 million people spread across six taluks (sub-districts).[10] Kolar is designated as the public health observatory of the Department of Epidemiology, National Institute of Mental Health and Neuro Sciences (NIMHANS). District health statistics indicate that there are 20 public hospitals and 41 private hospitals in Kolar.
All registered and consenting secondary and tertiary care hospitals in public and private located in rural and urban parts of the Kolar district were studied. These included hospitals having functional emergency room (ER)/casualty, intensive care unit (ICU), and operation theater (OT). In addition, all diagnostic and imaging centers in the district with computed tomography (CT) and magnetic resonance imaging scan facilities were also studied. Eligible hospitals refusing to provide information despite multiple efforts to collect data were excluded from the study.
An inception meeting was held with the District Health Officer (DHO) and a list of all secondary and tertiary hospitals in the public sector was obtained. A list of all private hospitals registered under the Karnataka Private Medical Establishments Act[11] and having ICU, OT, and ER was obtained from the DHO. This list of public and private hospitals was reviewed with DHO and finalized for complete enumeration as shown in Figure 1.
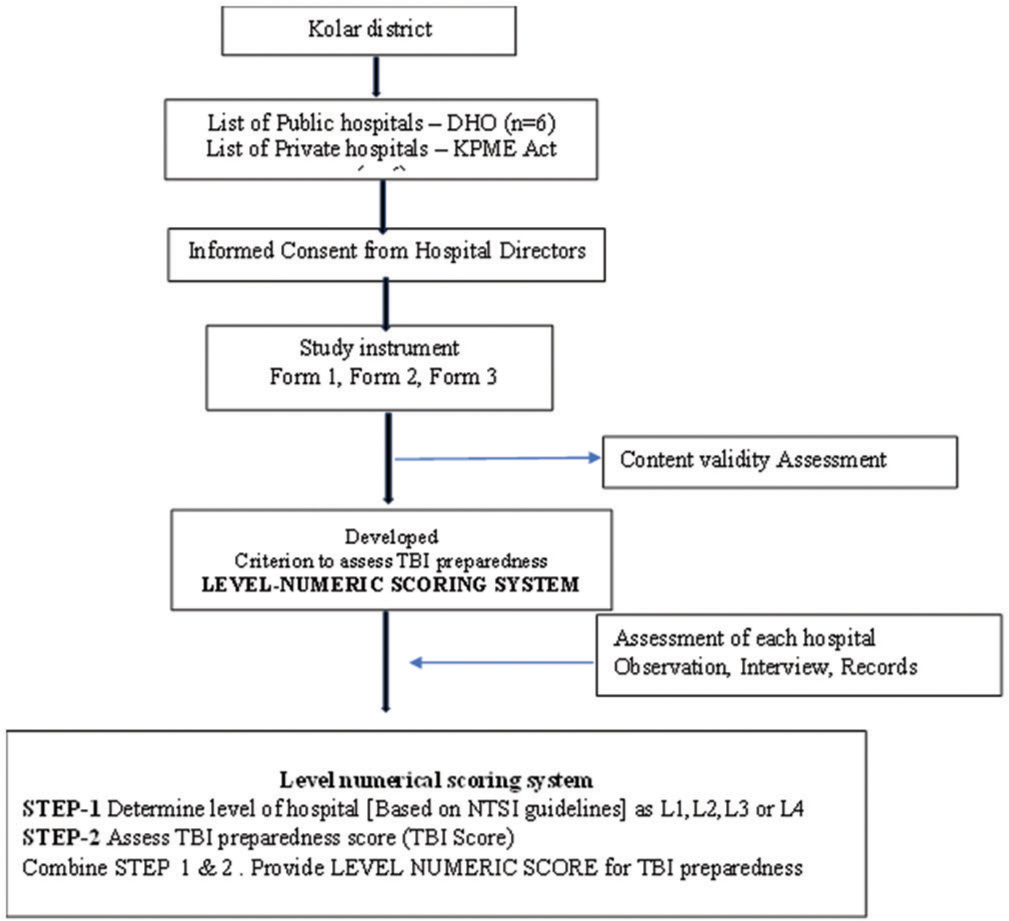
- Assessing preparedness of hospital for traumatic brain injury management – A flow chart.
Trained investigators visited each hospital in person, obtained informed consent from the director/or person in charge, and collected data on preparedness to manage TBI, using a specifically developed study instrument and criterion.
Study instrument
The study instrument and criterion for measuring preparedness were developed based on the review of the World Health Organization trauma care guidelines,[12] Neurocritical Care Society,[13] and NTSI guidelines.[9]
The study instrument consisted of three forms (Forms 1, 2, and 3). Details of assessment variables and mode of data collection for each form are presented in Table 1. E-review was done following which assessment variables were shortlisted, discussed with experts, and a draft instrument was prepared. Five subject experts rated the content validity of each item in the instrument on a four-point response scale (0 = not relevant, must be removed; 1 = not relevant, may be retained or removed; 2 = relevant and to be retained; 3 = very relevant and must be retained) based.
| S. No. | Forms | Variables | Domain of assessment | Method of data collection |
|---|---|---|---|---|
| 1. | Form 1 | Hospital general information. Beds in ER, ICU, and Tables in OT. Admissions – Trauma and TBI. Deaths – All causes, trauma, and TBI. Length of stay of TBI cases in ER and ICU. Age, gender, severity, and cause of TBI. |
Assess case load of TBI in the hospital Cause of TBI Duration of hospitalization |
Interview, review of medical records. |
| 2. | Form 2 | Macro areas Human resources and infrastructure. Drugs and consumables. Equipment availability across ER, ICU, and OT |
Facilities, human resources, and drugs available for TBI care | Interview, review of medical records, Observation. |
| 3. | Form 3 | Facilities available – CT/MRI. Manpower availability. CT and MRI scans for head injuries |
Case-load for imaging TBI proportion among total CT/MRI |
Interview, review of medical records. |
TBI: Traumatic brain injury, ER: Emergency room, ICU: Intensive care unit, OT: Operation theatre, CT: Computed tomography, MRI: Magnetic resonance imaging
Assessing and quantifying hospital-level preparedness for managing TBI
An objective criterion for assessing and quantifying hospital-level preparedness for TBI management based on NTSI criteria[9] called the level-numerical scoring system for TBI preparedness assessment was developed. This assessment process involves three steps.
Step 1: Determine the preparedness level of the hospital to manage TBI as per NTSI criteria
Based on available facilities and human resources for the management of neurotrauma [Table 2], hospitals were categorized into four levels (levels 1, 2, 3, and 4) by NTSI. Data were collected using forms 1 and 2 and the level of each hospital was determined as either L1, L2, L3, or L4 depicted in Table 2.
| Levels of hospitals | Criterion based on NTSI guidelines |
|---|---|
| Level 1 (All criteria to be satisfied) |
• 24/7 CT scan facilities • Neurosurgical and neurocritical care available full-time • Ability to handle head injury of any severity and major trauma of other systems. • Full-fledged ICU facility |
| Level 2 | • 24/7 CT scan facilities • Neuro surgeon is available on a call basis • Limited ICU and neurocritical facilities • Ability to handle moderate and minor head injuries which require surgeries |
| Level 3 | • 24/7 CT scan facilities • Trauma care services are available • Remote neurosurgical consultation (no onsite neurosurgeon) • Ability to handle moderate and minor head injuries – which do not require surgery (conservative management) • Referral to higher centers within 2 h if CT is abnormal |
| Level 4 | • No CT scan facilities • Have facilities to stabilize ABC • Conservative management of mild head injuries – not needing a CT scan |
TBI: Traumatic brain injury, NTSI: Neurotrauma Society of India, ICU: Intensive care unit, CT: Computed tomography, ABC: Airway, breathing, and circulation
Step 2: Calculate the TBI preparedness score for each hospital
After categorizing the hospitals’ level, a preparedness score for each hospital to manage TBI was determined, based on hospital facilities, human resources, and ICU facilities [Table 3]. This was deemed essential as hospitals with the same levels may have different ICU capabilities. This scoring criterion is designed to be simple to enable assessment by trained paramedical professionals and allow for objective assessment and monitor change in ICU facilities within and between different levels of hospitals. The criterion (variables and scoring) is presented in Table 3.
| S. No. | 24 h services | Level 1 | Score | Level 2 | Score | Level 3 | Score | Level 4 | Score |
|---|---|---|---|---|---|---|---|---|---|
| Facilities | |||||||||
| 1. | Mobile CT scan | Available | 5 | Available | 5 | NA | 0 | NA | 0 |
| 2. | CT scan (24 h) | Available | 5 | Available | 5 | Available | 5 | NA | 0 |
| 3. | Laboratory (24 h) | Available | 5 | Available | 5 | Available | 5 | Available | 5 |
| 4. | ECG facility | Available | 1 | Available | 1 | Available | 1 | Available | 1 |
| 5. | Mobile chest X-ray | Available | 1 | Available | 1 | Available | 1 | NA | 0 |
| 6. | Physiotherapy services in ICU* | Available | 1 | Available | 1 | Available | 1 | NA | 0 |
| Human resources | |||||||||
| 7. | Neurosurgeon | Available 24 h | 3 | On Call within 1 h | 2 | Remote NS consultation | 1 | NA | 0 |
| 8. | Pulmonologist | Available | 1 | Available | 1 | NA | 0 | NA | 0 |
| 9. | Cardiologists | Available | 1 | Available | 1 | NA | 0 | NA | 0 |
| 10. | Nephrologists | Available | 1 | Available | 1 | NA | 0 | NA | 0 |
| 11. | Endocrinologists | Available | 1 | Available | 1 | NA | 0 | NA | 0 |
| 12. | Anesthetist/intensivist | Available | 1 | Available | 1 | Available | 1 | NA | 0 |
| 13. | Neurocritical care specialist | Available | 2 | NA | 0 | NA | 0 | NA | 0 |
| 14. | Orthopedics | Available | 1 | Available | 1 | Available | 1 | NA | 0 |
| 15. | Other surgical specialists | Available | 1 | Available | 1 | Available | 1 | NA | 0 |
| 16. | TBI cases managed | Any severity | 3 | Moderate requiring surgery | 3 | Moderate and mild –conservative treatment | 2 | Mild cases do not require a CT scan | 1 |
| Total | 33 | 30 | 19 | 7 | |||||
| ICU score | |||||||||
| 17. | 24/7 Doctor | Intensivist | 2 | MBBS | 1 | MBBS | 1 | Others | 0 |
| 18. | Nurses prescribed | 1 Nurse/1 bed | 3 | 1 Nurse/2 bed | 2 | 1 Nurse/3–5 beds | 1 | 1 Nurse/5 beds | 1 |
| 19. | Monitors prescribed | For every bed | 2 | For every bed | 2 | For every bed | 2 | For every alternate bed | 1 |
| 20. | Mechanical ventilators | Available | 1 | Available | 1 | NA | 0 | NA | 0 |
| 21. | ABG analysis | Available | 2 | Available | 2 | Outsourced | 1 | NA | 0 |
| 22. | Defibrillator | Available | 1 | Available | 1 | Available | 1 | Available | 1 |
| 23. | Emergency drugs | Available | 1 | Available | 1 | Available | 1 | Available | 1 |
| 24. | Intracranial pressure monitoring | Available | 1 | NA | 0 | NA | 0 | NA | 0 |
| 25. | Step down ICU beds | Available | 1 | Available | 1 | Available | 1 | NA | 0 |
| 26. | Central line monitoring | Available | 1 | Available | 1 | Available | 1 | NA | 0 |
| 27. | Centralized oxygen supply piped |
Available | 1 | Available | 1 | NA | 0 | NA | 0 |
| 28. | Centralized suction supply piped |
Available | 1 | Available | 1 | NA | 0 | NA | 0 |
| 29. | Resuscitation equipment | Available | 1 | Available | 1 | Available | 1 | Available | 1 |
| 30. | Resuscitation equipment pediatric size |
Available | 1 | NA | 0 | NA | 0 | NA | 0 |
| 31. | A/C | Available | 1 | Available | 1 | Available | 1 | Available | 1 |
| Total | 20 | 16 | 11 | 6 | |||||
| Maximum possible score | 53 | 46 | 25 | 13 | |||||
Physiotherapy services in ICU can be delivered through trained nursing staff. TBI: Traumatic brain injury, ICU: Intensive care unit, ECG: Electrocardiogram, CT: Computed tomography, NA: Not available, *= Availability of trained nurse to perform chest physiotherapy and postural drainage (can also be scored) if physiotherapist is not available round the clock.
Step 3: Combine both to provide a level-numeric score of TBI preparedness
The level of each hospital and the TBI preparedness score of the hospital were clubbed to provide a level-numeric score of TBI preparedness for each hospital. Two hospitals of the same level may have different scores if ICU facilities differ.
Using the level-numeric scoring system, average preparedness scores can be summarized at the district level quantitatively, thereby providing scope to monitor changes in scores post-interventions to improve TBI care. It is simple to evaluate by nurses or allied health staff or health managers with minimal training, thereby improving acceptance and coverage.
Statistics
Data were entered in Microsoft Excel 2019 MSO and analyzed using SPSS version 23. Lawshe’s content validity ratio (CVR) method was used to calculate the CVR for each item in the study instrument using the formula
Ne is the number of experts indicating “very relevant” and “relevant,” and N is the total number of experts.
Data regarding the number of hospitals, number of beds, macro areas, demographic details of patients, number of trauma, and TBI cases in the public and private sector, and cause and severity of TBI are expressed as frequency and percentages. The median preparedness score of hospitals is presented and the proportion of hospitals in each level is presented.
RESULTS
Content validity
Out of the 58 items in Form 1, 56 items had good CVR (>0.5) and two items scored less CVR of 0.2. Of the 346 items in Form 2, 342 items scored a good CVR (>0.5) and four items had less CVR values of 0.2. Overall, good quality content was demonstrated.
TBI preparedness in the Kolar district
Level-numerical scoring of all studied hospitals is presented in Table 4. Of the 11 assessed hospitals, one hospital in the private sector was categorized as Level 2 and one hospital in the public sector as Level 3. The remaining nine hospitals are categorized as Level 4 as they did not have CT scan facilities or neurosurgeons and were managing mild head injuries. Of the nine Level 4 hospitals, five (55%) were in the public sector.
| S. No. | Hospital id | Preparedness level | Preparedness score | Level- numeric score |
|---|---|---|---|---|
| 1. | H-1 | L4 | 12 | L4-12 |
| 2. | H-2 | L4 | 09 | L4-09 |
| 3. | H-3 | L4 | 11 | L4-11 |
| 4. | H-4 | L4 | 8 | L4-08 |
| 5. | H-5 | L4 | 8 | L4-08 |
| 6. | H-6 | L3 | 23 | L3-23 |
| 7. | H-7 | L4 | 11 | L4-11 |
| 8. | H-8 | L4 | 12 | L4-12 |
| 9. | H-9 | L4 | 05 | L4-05 |
| 10. | H-10 | L2 | 35 | L2-35 |
| 11. | H-11 | L4 | 13 | L4-13 |
TBI: Traumatic brain injury
The numeric score varied between 05 and 35 in the assessed hospitals. The numerical scores in Level 4 hospitals ranged between 05 and 13 with an average score of 11. Numerical scores of preparedness differed within the same level of hospital indicating differences in ICU functioning and facilities. 9% of hospitals were classified as Level 2 with a score of 16, 9% as Level 3 with a score of 11, and 81% as Level 4 with a score of 6.
DISCUSSION
The study is a unique attempt to objectively assess and quantify hospital-level preparedness to manage TBIs as per NTSI guidelines (2022), covering both private and public hospitals in an Indian district. The study provides a tool and criterion for objective quantification of hospital-level preparedness to manage TBIs, hence having widespread applications in surveillance, monitoring, resource allocation, and assessment of the effectiveness of health system development interventions. Though tools to assess trauma care systems are available,[14] a specific tool for objectively assessing systems for TBI management is not available and our study fills this gap.
Data extraction from records was one of the modes of data collection in this assessment. It was observed that medical records pertaining to TBIs were not uniform across the hospitals, indicating a need for a standard case format for TBIs identification and management. This would help to establish a uniform hospital-based TBI surveillance system.
Our assessment revealed that there was not even a single hospital corresponding to Level 1 preparedness to manage TBI and there was one hospital with Level 2 preparedness, indicating that existing hospitals in the Kolar are prepared to manage only mild and moderate TBI cases. To manage severe cases, a Level 1 hospital is required. Our assessment indicated a huge disparity between the need for TBI care versus the availability and preparedness of systems and services to manage TBI. The highest score observed was L2–40.
Even though functional ICUs are present in many hospitals, the lack of neurosurgeons to perform surgeries categorizes hospitals as Level 3 instead of Level 2. Irrespective of the numerical score, the hospital level can shift upward only if it fulfills the criteria of full-time CT scan, availability of neurosurgeon (full-time, on-call, and remote neurosurgical consultation), and full-fledged ICU. Thus, moving up in levels needs significant resources.
The availability of neurosurgeons is critical in upgrading Level 3 hospitals to Level 2 or Level 1. Most of the assessed hospitals (82%) were functioning at Level 4 preparedness, that is, the preparedness corresponds to the management of mild TBI cases. Hence, trained manpower is a critical factor to upgrade levels of hospitals. A relook of the current medical education system for neurosurgery is required to understand methods to increase the availability of neurosurgeons in India. At present, there is one neurosurgeon per 10 lakh people in India.[15] Replication of assessments in other districts will help to quantify state- and national-level TBI management preparedness. As the assessment is objective and uniform, this level-numeric scoring system would enable comparison and progress monitoring.
Our assessment indicates that TBI management is highly dependent on special human resources such as neurosurgeons, facilities in OT, and ICU care. These are very important variables for preparedness to manage TBI. Apart from these, many other variables such as algorithms, capacity building of paramedic personnel, referral, and monitoring mechanisms are required to manage TBI in the Kolar district.
In summary, the preparedness of hospitals to manage TBI is limited to Levels 3 and 4, that is, the management of moderate and mild cases. The lack of neurosurgeons in Kolar could be attributed to the proximity of Kolar to Bengaluru city, which has many Level 4 hospitals, resulting in less demand for TBI care in the Kolar district.
Strengths
This study is a unique first attempt to objectively assess hospitals’ preparedness for TBI management. Our study developed a tool and methodology and tested its feasibility to objectively quantify hospital-level preparedness to manage TBI as well as to monitor the preparedness levels over time. This study was a combined effort of public health and neurosurgeons, which is required for strengthening public health approaches in neurotrauma care in India, especially in rural areas. One of the key strengths is testing the feasibility across entire districts covering all secondary/tertiary/public and private hospitals at district and taluka levels.
Limitations
One medical college did not provide consent for the study, hereby underestimating overall preparedness levels in the Kolar district.
Future recommendations
As our observations indicate that it is feasible to assess and quantify the preparedness of hospitals to manage TBIs using our tool, we recommend the following
To undertake validity and reliability testing of the level-numerical scoring system across hospitals in different districts and develop an online portal for hospitals to use this scoring system. Neurotrauma Society of India to facilitate this process across the country
To facilitate district health authorities to use this tool as an assessment evaluation parameter to improve scoring for TBI preparedness in the district. Based on the assessment of preparedness levels, establish a prompt referral network and good networking of health-care facilities of all levels within 50–100 km
To train and capacity-build generalist physicians, surgeons, and nurses to improve ICU and ER care for neurotrauma, as a short-term measure. District health authorities to develop mechanisms to appoint full-time/ part-time neurosurgeons in district hospitals
To develop and disseminate algorithms for TBI case management in ER and ICU for each level of the hospital, based on their preparedness levels to manage TBI cases
Develop a uniform digital HMIS system for surveillance and monitoring of TBIs and trauma cases across all levels of hospitals in the Kolar district.
CONCLUSION
The study has measured hospital-level preparedness to manage TBI cases in secondary and tertiary-level hospitals in Kolar district. Preparedness was limited to Level 4 in the Kolar district, which implies hospitals are prepared to manage mild and moderate cases of TBIs that require conservative care. The study throws light on the need for comprehensive strengthening of secondary and tertiary hospitals to manage TBI cases in the Kolar district.
Acknowledgment
The completion of this undertaking could not have been possible without the participation and assistance of so many people whose names may not all be enumerated. Their contribution is sincerely appreciated and gratefully acknowledged.
We extend our heartfelt appreciation to the private hospitals, DHOs, Hospital directors, and Kolar district officers who provided invaluable guidance, feedback, and expertise throughout the research process. Their constructive criticism and thoughtful suggestions greatly enriched the quality of this work.
The collaborative efforts of all these individuals have made this manuscript possible, and we offer our heartfelt appreciation for their contributions.
Ethical approval
Ethics approval for the study was obtained from the Institutional Ethics Committee, NIMHANS [NO. NIMH/ DO/IEC (BS&NS DIV)/2022], dated 8th June 2022 and informed consent was obtained from the hospital directors or equivalents.
Declaration of patient consent
Patient’s consent is not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Get the Facts about TBI. 2023. Available from: https://www.cdc.gov/traumaticbraininjury/get_the_facts.html [Last accessed on 2023 Oct 12]
- [Google Scholar]
- GBD India Compare. Available from: https://vizhub.healthdata.org/gbdcompare/india [Last accessed on 2023 Oct 12]
- [Google Scholar]
- A key traumatic brain injury initiative in India. Lancet Neurol. 2016;15:1011-2.
- [CrossRef] [PubMed] [Google Scholar]
- The burden of neurological disorders across the states of India: The Global Burden of Disease study 1990-2019. Lancet Glob Health. 1990;9:e1129-44.
- [Google Scholar]
- Epidemiology of traumatic brain injuries: Indian scenario. Neurol Res. 2002;24:24-8.
- [CrossRef] [PubMed] [Google Scholar]
- Safety on road safety. A case study. Available from: https://nimhans.ac.in/wp-content/uploads/2019/02/gururaj_highway-safety-report_-final_-22-june-2015.pdf [Last accessed on 2023 Oct 12]
- [Google Scholar]
- India: Estimated number of public and private hospitals. Available from: https://www.statista.com/statistics/1128425/india-number-of-public-and-private-hospitals-estimated [Last accessed on 2023 Oct 12]
- [Google Scholar]
- The Sunday guardian live. More trauma care hubs will bring down highway fatality rates. 2022. Experts. Available from: https://sundayguardianlive.com/news/trauma-care-hubs-will-bring-highway-fatality-rates-experts [Last accessed on 2023 Oct 12]
- [Google Scholar]
- Available from: https://neurosocietyindia.com/wp-content/uploads/2022/03/ntbi_merged_seventh-proof.pdf [Last accessed on 2023 Oct 12]
- Karnataka at glance. Available from: https://kgis.ksrsac.in/kag [Last accessed on 2023 Oct 12]
- [Google Scholar]
- Home. Available from: https://kpme.karnataka.gov.in/allapplicationlist.aspx [Last accessed on 2023 Oct 12]
- [Google Scholar]
- Available from: https://iris.who.int/bitstream/handle/10665/42565/9241546409_eng.pdf [Last accessed on 2023 Oct 12]
- Correction to: Standards for neurologic critical care units: A statement for healthcare professionals from the neurocritical care society. Neurocrit Care. 2019;31:229.
- [CrossRef] [PubMed] [Google Scholar]
- Trauma care systems in healthcare facilities of an Indian District: Assessment and future directions. J Family Med Prim Care. 2023;12:567-75.
- [CrossRef] [PubMed] [Google Scholar]
- Shortage of neurosurgeons in India major issue, notes AIIMS doctor. The New Indian Express. Available from: https://www.newindianexpress.com/cities/delhi/2022/mar/22/shortage-of-neurosurgeons-in-indiamajor-issue-notes-aiims-doctor-2432824.html [Last accessed on 2023 Aug 24]
- [Google Scholar]







