Translate this page into:
Unveiling the mystery: Infective endocarditis as an etiological cause of recurrent intracranial hemorrhage
-
Received: ,
Accepted: ,
How to cite this article: Thuppanattumadam Ananthasubramanian S, Nashi S, Taallapalli A, Krishna Reddy H, Arshad F, Srijithesh PR, et al. Unveiling the mystery: Infective endocarditis as an etiological cause of recurrent intracranial hemorrhage. J Neurosci Rural Pract. doi: 10.25259/JNRP_35_2024
Abstract
Intracerebral hemorrhage (ICH) in the context of infective endocarditis (IE) is an uncommon and complex phenomenon involving diverse underlying mechanisms. We present a compelling case of a 48-year-old patient with recurrent ICH, ultimately leading to the diagnosis of IE with vegetation on the anterior leaflet of the mitral valve. The patient underwent a successful mitral valve replacement followed by a gradual improvement in neurological symptoms. This case report delves into the intricate diagnostic journey, highlighting the significance of suspecting IE in patients presenting with ICH. A multidisciplinary and comprehensive management approach played a pivotal role in achieving positive outcomes.
Keywords
Intracerebral hemorrhage
Infective endocarditis
Mitral valve
Vegetations
Recurrent IC bleed
INTRODUCTION
Intracerebral hemorrhage (ICH) is a critical neurological event often stemming from a multitude of underlying factors, ranging from hypertension, coagulopathy, and vascular anomalies to systemic disorders.[1] Among the diverse etiologies, infective endocarditis (IE) emerges as a rare and compelling cause, intricately linking cardiac pathology to cerebral vascular complications.[2-5] While ICH evokes immediate concern, its recurrence raises a heightened urgency for precise diagnosis and targeted intervention. In this case report, we illuminate the distinctive narrative of a 48-year-old patient, who experienced recurrent ICH, a phenomenon that ultimately unveiled a diagnosis of IE. This unique intersection of neurological and cardiovascular domains underscores the need for heightened clinical suspicion, meticulous diagnostic exploration, and comprehensive management strategies. The case not only accentuates the complexity of recurrent ICH but also underscores the significance of recognizing IE as an unexpected yet crucial contributor to such presentations.
CASE REPORT
A 48-year-old man visited our center with a history of sudden onset of altered sensorium, irrelevant speech, and an inability to recognize family members, which occurred three months before presentation. Imaging studies done at another center revealed a right parietal bleed, prompting immediate management with anti-seizure medications and anti-edema measures, following which he gradually improved. In the following three months, he developed recurrent fevers, which occurred every —two to three days, accompanied by an evening temperature rise without chills and rigors. Extensive evaluation at another medical center led to the discovery of a splenic infarct on a positron emission tomography–computed tomography (CT) whole-body scan. He was initiated on empirical anti-tubercular therapy for pyrexia of unknown origin. However, despite treatment, the patient developed altered sensorium, irritability, and right-sided weakness five days before presenting at our center. He was not a known case of hypertension or diabetes and had no history of substance abuse. Vitals showed a pulse rate of 120 beats/min with blood pressure of 130/80 mmHg. Mild pallor was noted on general physical examination. Cardiac auscultation revealed soft S1 with a pansystolic murmur noted in the mitral area. The patient was conscious, but agitated and disoriented. However, he was able to follow simple commands. He had no neck stiffness. On cranial nerve examination, there was no abnormality noted. Motor examination uncovered right hemiparesis and dragging of the right leg during ambulation (accurate power assessment was not possible in view of mixed aphasia). He also has decreased arm swing on the right side while walking. Routine investigations revealed anemia (hemoglobin: 11.1 g/dL) with neutrophilic leukocytosis (25,900 cells/μL) and normal platelet count. Liver and kidney function tests were within normal limits. Imaging studies showed a left temporoparietal bleed alongside a resolving hematoma in the right parietal region, with no evidence of cerebral venous thrombosis. Imaging studies showed a left temporoparietal bleed alongside a resolving hematoma in the right parietal region, with no evidence of cerebral venous thrombosis [Figure 1]. A CT thorax revealed no significant abnormalities. Recurrent cerebral parenchymal bleeding can result due to hypertension, coagulopathy, arteriovenous malformations, cerebral aneurysms, moyamoya disease, amyloid angiopathy, and cerebral venous thrombosis.[1] In view of recurrent parenchymal bleeding, a possibility of IE, although rare, was considered, as the patient had a history of pyrexia of unknown origin.
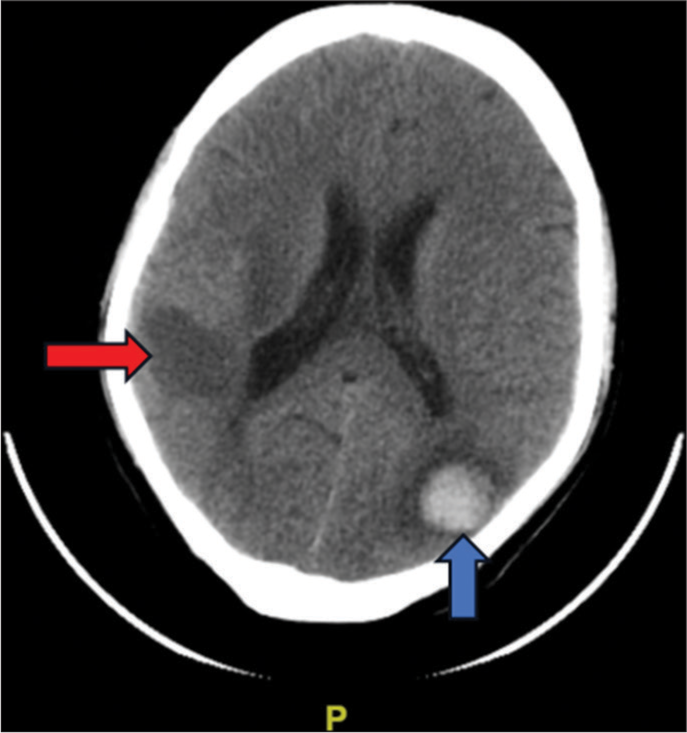
- Non-contrast Computed Tomography (CT) scan of the brain showing left parietal lobe hemorrhage (blue arrow) and hypodensity over the right parietal region (red arrow), suggestive of resolving hematoma.
A 2D echocardiography confirmed the diagnosis of IE, revealing vegetation on the anterior leaflet of the mitral valve. A 2D echocardiography confirmed the diagnosis of infective endocarditis, revealing a vegetation on the anterior leaflet of the mitral valve [Figure 2].
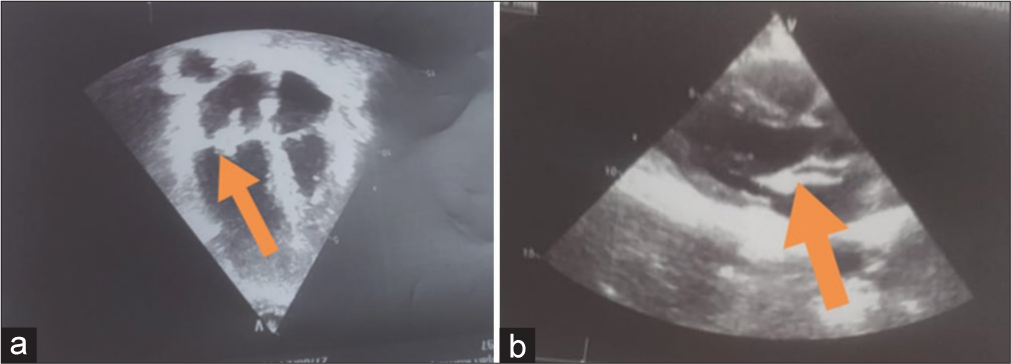
- 2D Echocardiography of the heart reveals a mobile vegetation on the anterior leaflet of mitral valve in (a) Apical four chamber view (Orange arrow) and (b) Parasternal long axis view (Orange arrow).
MANAGEMENT AND FOLLOW-UP
Given the severity of the presentation and the strong suspicion of IE, the patient was referred to a cardiology center where the patient underwent successful mitral valve replacement with an SJM 25 mm mechanical valve. Subsequent tissue culture revealed colonies of Gram-positive cocci, supporting the diagnosis of definite IE by 2023 Duke-ISCVID criteria.[6]
The patient received comprehensive management, including anti-edema measures, anti-epileptics, broad-spectrum antibiotics, and appropriate antiplatelets. Angiotensin-converting-enzyme inhibitors and beta-blockers were prescribed to optimize cardiovascular function. Gradually, the patient’s condition improved, with residual difficulties noted in wayfinding, calculation, and naming at two-year follow-up.
DISCUSSION
Intracranial hemorrhage in IE can arise from three different mechanisms – ruptured mycotic aneurysm, hemorrhage following an acute ischemic stroke, and ICH of undetermined etiology. In the previous studies, the prevalence of these mechanisms was found to vary, with undetermined etiology accounting for 28% of cases, ruptured mycotic aneurysm for 32%, and hemorrhage after ischemic stroke for 40%.[2,7]
To predict ICH risk in IE, five variables have been identified as associated factors, including platelet count <150 × 10^9/L, severe regurgitation, cerebral ischemic embolism, other symptomatic systemic embolisms, and the presence of mycotic aneurysm.[2]
The mechanism of ischemic stroke involves the migration of a “macro” fragment or the entire vegetation into cerebral arteries.[5,8] In contrast, mycotic aneurysms arise from “microemboli” to the vasa vasorum and can also be secondary to bacterial escape from a septic “macroemboli” that occludes a vessel.[3,5] As for ICH of undetermined etiology, it may result from septic arteritis, with an erosion of the vessel wall caused by “microemboli,” but without a well-delineated aneurysm.[3]
This diagnostic odyssey sheds light on the intricate and rare association between recurrent intracranial hemorrhage and IE in a patient with pyrexia of unknown origin. The diverse mechanisms underlying ICH in IE warrant close attention, guiding clinicians to consider this unique etiology in patients with unexplained intracranial bleeding. A multidisciplinary approach and comprehensive management played a pivotal role in optimizing outcomes in this challenging case.
CONCLUSION
This case report underscores the significance of recognizing IE as an underlying cause of recurrent intracranial hemorrhage. The diagnostic journey and successful management highlight the importance of thorough evaluation and tailored treatment strategies. Vigilant follow-up and rehabilitation efforts contribute to enhancing patient recovery and quality of life. This rare case serves as a compelling reminder for clinicians to remain vigilant for IE in patients presenting with recurrent intracranial hemorrhage.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Recurrent intracerebral hemorrhage: Associations with comorbidities and medicine with antithrombotic effects. PLoS One. 2016;11:e0166223.
- [CrossRef] [PubMed] [Google Scholar]
- Intracranial haemorrhage in infective endocarditis. Arch Cardiovasc Dis. 2018;111:712-21.
- [CrossRef] [PubMed] [Google Scholar]
- Mechanisms of intracranial hemorrhage in infective endocarditis. Stroke. 1987;18:1048-56.
- [CrossRef] [PubMed] [Google Scholar]
- Neurologic manifestations of infective endocarditis a 17-year experience in a teaching hospital in Finland. Arch Intern Med. 2000;160:2781-7.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of stroke on therapeutic decision making in infective endocarditis. J Neurol. 2010;257:315-21.
- [CrossRef] [PubMed] [Google Scholar]
- The 2023 Duke-International Society for cardiovascular infectious diseases criteria for infective endocarditis: Updating the modified duke criteria. Clin Infect Dis. 2023;77:518-26.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical utility of cerebral angiography in the preoperative assessment of endocarditis. Vasc Med. 2014;19:500-6.
- [CrossRef] [PubMed] [Google Scholar]
- Grand round case presentation a dangerous dilemma: Management of infectious intracranial aneurysms complicating endocarditis. Lancet Infect Dis. 2006;6:742-8.
- [CrossRef] [PubMed] [Google Scholar]






