Translate this page into:
Unilateral Vision Loss without Ophthalmoplegia as a Rare Complication of Spinal Surgery
Address for correspondence: Dr. Mehmet Sabri Gürbüz, Yıldıztepe Mah., Bağcılar Cad., No: 108 34203 Bağcılar, İstanbul, Turkey. E-mail: mehmetsabrigurbuz@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Postoperative visual loss is an extremely rare complication of nonocular surgery. The most common causes are ischemic optic neuropathy, central retinal artery occlusion, and cerebral ischemia. Acute visual loss after spinal surgery is even rarer. The most important risk factors are long-lasting operations, massive bleedings, fluid overload, hypotension, hypothermia, coagulation disorders, direct trauma, embolism, long-term external ocular pressure, and anemia. Here, we present a case of a 54-year-old male who developed acute visual loss in his left eye after a lumbar instrumentation surgery and was diagnosed with retinal artery occlusion.
Keywords
Lumbar instrumentation
nonocular surgery
postoperative visual loss
retinal artery embolism
retinal artery occlusion
INTRODUCTION
Visual loss seen after nonocular surgery is an uncommon but dramatic complication.[1] It has been reported in literature that it may be caused by longer anesthetic duration, massive bleeding, hypotension, hypothermia, coagulation disorders, direct trauma, embolism, long-term external ocular pressure, and anemia.[23] These risk factors are thought to lead to an increase in the venous pressure, resulting in optic nerve damage. Ischemic optic neuropathy, central retinal artery occlusion, and cerebral ischemia have been reported as the major underlying pathologies.[1345] Postoperative visual loss might also be caused by pituitary apoplexy and resultant optic nerve injury.[6]
The incidence of postoperative visual loss increases as the number of complicated and prolonged spinal surgeries increases.[7] On the other hand, isolated vision loss, which is the vision loss without ophthalmoplegia, is a rarer presentation.[5] We present a case of isolated unilateral vision loss seen after lumbar instrumentation surgery secondary to central retinal artery occlusion and discuss the possible causative factors under the light of the current literature.
CASE REPORT
A 54-year-old male presented to our outpatient clinic with a 3-week history of low back pain radiating down to his right leg. The patient's medical history was unremarkable except for an operation of cholecystectomy 5 years previously. The patient's physical examination was unremarkable. Neurogenic claudication and lumbar radiculopathy were detected in his neurological examination. Grade 1 spondylolisthesis, multiple discopathies, and lumbar spinal stenosis were detected on his lumbar magnetic resonance imaging (MRI) scan.
After completing the appropriate preoperative evaluation, the patient was taken to the operation theater and placed on the operating table in the prone position under general anesthesia. As routinely done, silicon pads and pillows were placed to pressure points to provide pressure relief. The patient underwent a 2-level lumbar micro-discectomy, 4-level decompression, and 4-level transpedicular screw fixation surgery. The total duration of the operation was 270 min. The patient's blood pressure remained within normal limits (110/70 mmHg) except for 30 min of 90/70 mmHg during the surgery. Total blood loss was 500 ml and urine output was 300 ml. The replacement was performed with 1000 ml of normal saline with no need for blood transfusion. The lowest hematocrit level detected during the surgery and in the early postoperative period was 42%.
Immediately after the surgery, the patient complained of having no vision in his left eye. In ophthalmologic examination, visual acuity was 20/20 in the right eye and he had no vision and no light perception in the left eye. There was relative afferent pupil defect in his left eye. In the fundoscopic examination, the right retina was normal and the left retina was completely pale [Figure 1a and b]. Upon consultation with the department of ophthalmology, the intraocular pressures of both eyes were measured and detected within normal limits (18 mmHg). In the biomicroscopic examination, the anterior segment structures of both eyes were normal. There was no problem in the functions of the extraocular muscles. Based on the suggestion of the department of ophthalmology, the patient was started on carbonic anhydrase inhibitor as the first-line treatment. The brain MRI and diffusion MRI of the patient were normal. In fundus fluorescein angiography (FFA), there was no filling defect in the retinal vascular structures in the left eye [Figure 2]. On computed tomography angiography, there was no filling defect in the vertebral artery, internal carotid artery, ophthalmic artery, and retinal arteries. Anterior chamber paracentesis was performed at the 20th h of the surgery. The patient was discharged with a loss of vision in the left eye on the 5th day of operation. The patient was followed up at regular intervals at outpatient clinic. However, the patient's vision and light reflex did not improve during the 1st month of operation.
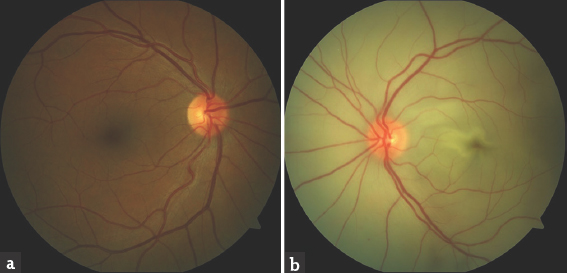
- Fundoscopic views of both eyes performed immediately after the detection of vision loss. Fundoscopic view of the right eye (a) reveals normal findings; however, fundoscopic view of the left eye (b) reveals total retinal paleness
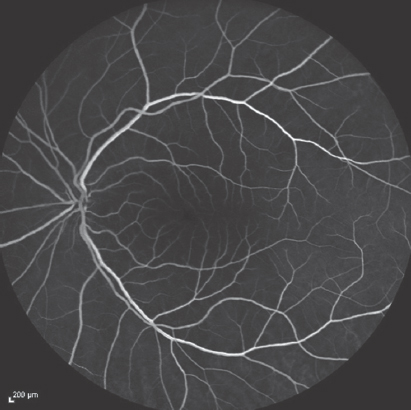
- Fundus fluorescein angiography of the left eye performed immediately after the detection of vision loss reveals that the filling of the left retinal artery and vein is normal (15th s)
During the examination of the patient at the 4th week, visual acuity was recorded as at the level of hand movements in the left eye. In fundoscopic examination, the left optic disc was pale, the vascular structures were highly thinned, and the left retina was atrophic [Figure 3]. In FFA performed on the same day, the vascular structures were thinned, there was a delay in their filling, and there were hypofluorescence areas secondary to retinal atrophy on the left optic disc [Figure 4]. No further improvement was achieved in the vision in the 3rd month, the 6th month, and 1 year of follow-up.
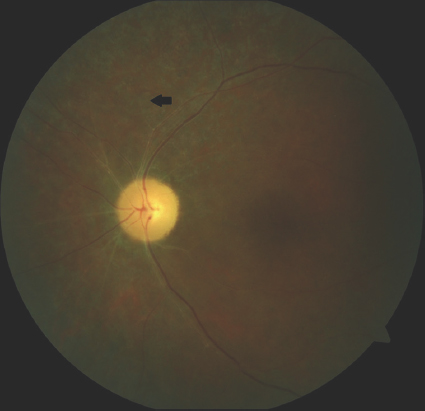
- Fundoscopic view of the left eye performed at the 4th week of the vision loss reveals vascular attenuation and left retinal atrophy indicated in black arrow

- Fundus fluorescein angiography of the left eye performed at the 4th week of vision loss reveals thinned vascular structures and their delayed filling. Black arrow indicates hypo-fluorescent area secondary to retinal atrophy on the left optic disc (14th s)
DISCUSSION
Although postoperative visual loss is a rare complication of nonocular surgery, it might be irreversible which would be a dramatic consequence.[34] Few cases of central retinal artery embolism occurring after nonocular surgery have been reported so far. The highest incidence was reported as 0.28% after scoliosis surgery[8] and 0.14% after posterior lumbar instrumentation.[7]
The underlying mechanism of postoperative visual loss has not yet been fully understood.[9] Its etiology could not be fully elucidated in most of the cases; however, most of them are considered to be multi-factorial.[10] Of the cases reported so far, 67% has been found associated with the spinal surgeries performed in the prone position.[9] Preoperative risk factors include male gender, hypertension, diabetes, hyperviscosity syndromes (sickle cell anemia, polycythemia vera), smoking, renal failure, narrow-angle glaucoma, atherosclerotic vascular disease, and collagen-vascular diseases.[4910] Perioperative risk factors possibly responsible for this complication include massive blood loss, fluid overload, hypotension, hypothermia, coagulation disorders, direct trauma, embolism, long-term external pressure on the eye, increased intraocular pressure due to prone position, and anemia.[23410]
Our case is unusual having no predisposing factors such as cardiovascular diseases, diabetes, hypertension, and smoking. However, prone position, a relatively long duration of surgery, and hypotension due to perioperative bleeding can be considered as the risk factors. Although the patient's blood pressure was 110/70 mmHg during the surgery, it remained 90/70 mmHg for 30 min. The lowest hemoglobin level was 42% during and shortly after the surgery which indicates an appropriate fluid balance during the surgery.
One of the causes of visual loss after spinal surgery is retinal ischemia due to increased external ocular pressure in the prone position.[35] Eye bumpers may disrupt the arterial and venous circulation of the eye and may lead to postoperative edema.[5] Edema, redness, and total ophthalmoplegia have been recorded in all cases reported so far. However, such findings, which might indicate perioperative external ocular compression, were not present in our case although retinal artery occlusion was detected on the ocular angiography.
An increase in intraocular pressure is another risk factor for postoperative visual loss which might be caused by central venous insufficiency.[9] An increase in the abdominal pressure and head being at a lower level are the causes of increased central venous pressure.[911] In our patient, the patient's head was placed on a silicon headrest in neutral position and there was no ocular compression. Moreover, by placing silicon pillows under the abdomen, a possible increase in the intra-abdominal pressure was prevented. Postoperative intraocular pressure was found normal in both eyes of our patient.
Central retinal artery occlusion causes a particular decrease in retinal blood supply. Hollenhorst et al.[12] described central retinal artery occlusion in eight patients after spinal surgery performed in prone position on horseshoe headrest. Roth reported a case of unilateral central retinal artery occlusion secondary to the compression of the protective eyeglasses in a patient operated in the prone position.[13] The treatment options for central retinal artery occlusion are carbogen inhalation, acetozalamide, intravenous glyceryltrinitrate, ocular massage, and paracentesis, although none of them has been proved to alter its natural history definitely. Retinal damage is considered to turn irreversible after 6 h although the exact time when it becomes irreversible is not known.[14] In our patient, fundoscopic examination and angiography were performed in a very short time after the surgery. However, anterior chamber paracentesis was performed at the 20th h of the surgery which is accepted late according to the current literature. Although it is not known whether paracentesis can change the natural history of the central retinal artery occlusion, it should be performed in the first 6 h of vision loss. If retinal artery occlusion is not diagnosed early and treated in time, irreversible vision loss will be an inevitable consequence.
Knowing that central retinal artery occlusion is almost always irreversible and there is no effective treatment, it is crucial to take necessary precautions to prevent its occurrence. Anesthesiologists and surgeons must be aware of the risk factors which might cause postoperative vision loss and they should take the necessary measures to avoid this rare but devastating complication.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Ischemic optic neuropathy following spine surgery. J Neurosurg Anesthesiol. 2005;17:38-44.
- [Google Scholar]
- Postoperative vision loss after spine surgery: A single-institution case-control comparison. Ochsner J. 2014;14:179-83.
- [Google Scholar]
- Acute visual loss with ophthalmoplegia after spinal surgery: Report of a case and review of the literature. Indian J Ophthalmol. 2014;62:963-5.
- [Google Scholar]
- Central retinal artery occlusion and ophthalmoplegia following spinal surgery in the prone position. Med J Malaysia. 2009;64:323-4.
- [Google Scholar]
- Perioperative visual loss in ocular and nonocular surgery. Clin Ophthalmol. 2010;4:531-46.
- [Google Scholar]
- Amaurosis after spine surgery: Survey of the literature and discussion of one case. Eur Spine J. 2011;20:171-6.
- [Google Scholar]
- Central retinal artery occlusion after scoliosis surgery with a horseshoe headrest. Case report and literature review. Spine (Phila Pa 1976). 1993;18:1226-8.
- [Google Scholar]
- Postoperative visual loss following prone spinal surgery. J Anaesth. 2005;95:257-60.
- [Google Scholar]
- Monocular blindness due to central retinal artery occlusion in bipolar hemireplacement arthroplasty of the hip. Singapore Med J. 2008;49:e96-7.
- [Google Scholar]
- Perioperative visual loss after nonocular surgeries. Am J Ophthalmol. 2008;145:604-10.
- [Google Scholar]
- Unilateral blindness occurring during anesthesia for neurosurgical operations. AMA Arch Ophthalmol. 1954;52:819-30.
- [Google Scholar]
- Perioperative visual loss: What do we know, what can we do? Br J Anaesth. 2009;103(Suppl 1):i31-40.
- [Google Scholar]
- Treatment options for central retinal artery occlusion. Curr Treat Options Neurol. 2013;15:63-77.
- [Google Scholar]






