Translate this page into:
Twin Middle Cerebral Artery with Aneurysm: A Variant of Early Bifurcation or a Discrete Entity
Address for correspondence: Dr. Sushant Sahoo, Department of Neurosurgery, KGMU, Lucknow, Uttar Pradesh, India. E-mail: drsushantsahoo@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The middle cerebral artery (MCA) usually bifurcates into a superior or frontal and inferior or temporal branch. However, it may have various branching pattern, and there may be additional arteries from the anterior circulation supplying its territory. The majority of them remain asymptomatic. Some cases may have aneurismal dilatation due to turbulent blood flow or the weak arterial wall. The surgical approach in these cases may be challenging due to complex anatomical pattern of MCA. In this report, we have described a distinct pattern of left MCA with an aneurysm which was not clear in computed tomography angiogram and further confirmed on digital subtraction angiography. The different anatomical patterns of MCA and their surgical implications have also been discussed.
Keywords
Aneurysm
computed tomography angiography
middle cerebral artery
subarachnoid hemorrhage
INTRODUCTION
Various branching patterns of middle cerebral artery (MCA) have been described in literature. Early bifurcation, duplicated MCA, accessory MCA, trifurcation, and quadrifurcation are commonly discussed.[1] Although most of them remain clinically silent, these anomalous subdivisions of MCA have additional risk of aneurysm formation.[2] The anomalous arterial geometry poses great difficulty in surgical exposure and also there is a potential risk of injuring additional cortical branches. We describe here a case of ruptured MCA aneurysm in a young male with a unique cortical branching pattern highlighting the operative nuances.
CASE REPORT
A 30-year-old male patient admitted to our emergency department with complaints of sudden onset severe headache and altered sensorium. At presentation, he was conscious but disoriented. After initial resuscitations, computed tomography (CT) scan was done which showed left perisylvian hematoma with diffuse subarachnoid hemorrhage [Figure 1a]. Then, a CT angiography (CTA) was obtained which demonstrated the early bifurcation of the MCA with each branch further divided into frontal and temporal branches. There was a fusiform dilation at the origin of the dominant frontal branch [Figure 1b]. Digital subtraction angiography (DSA) was done that clarified the secular nature of the aneurysm [Figure 1c]. The patient was operated by left pterional craniotomy. The MCA had early bifurcation with a dominant branch which was traced further distally. Only after the second branching point, aneurysm was reached and there was fusiform dilation of the artery proximal to the aneurysm. Aneurysm was clipped without any intraoperative rupture, and muscle wrapping over the dilated proximal segment was done [Figure 1d and e]. There was no perioperative complication and postoperative CT showed no infarction in the territory of MCA [Figure 1f]. The patient improved completely without any added deficit.
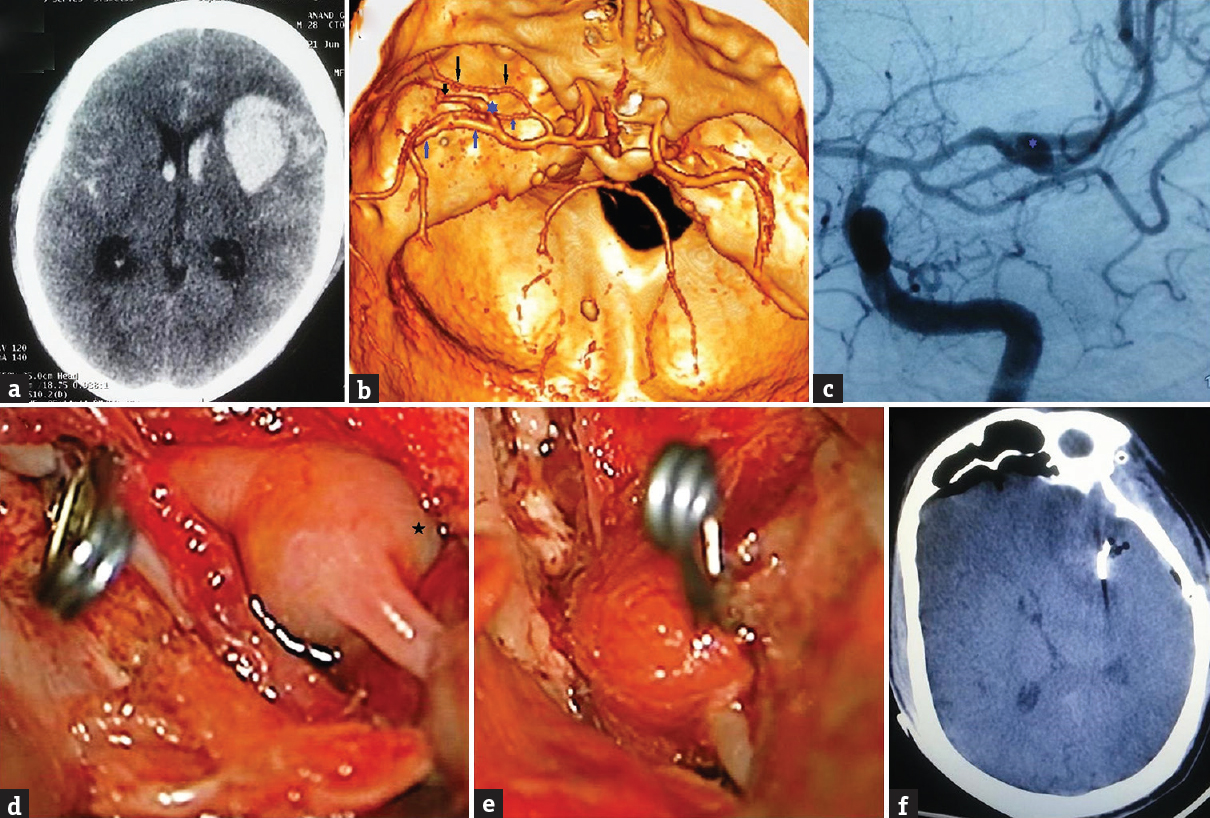
- (a) Computed tomography scan showing left sylvian hematoma with diffuse subarachnoid hemorrhage. (b) Computed tomography angiography showing the early division of middle cerebral artery. Each artery divided into frontal (black arrows) and temporal (blue arrows) branches. Note the fusiform dilation (blue star) at the origin of the dominant frontal branch. (c) Digital subtraction angiography showing the secular nature of the aneurysm (blue star). (d) Intraoperative image showing the temporary clip just proximal to the aneurysm and the aneurysm sac (black star). (e) intraoperative image showing the clipped aneurysm with muscle wrapping. (f) Postoperative computed tomography scan showing the clip with no hematoma or infarct in territory of middle cerebral artery
DISCUSSION
The MCA along with its frontal and temporal branch usually course along the sylvian fissure. Sometimes, supplementary branches may follow the course of MCA in the sylvian fissure. Arteries arising independently from the internal carotid artery (ICA) and coursing along the MCA are termed as duplicated MCA and their incidence is <2% in DSA. Accessory MCA arises from the ACA and course along the sylvian fissure to supply the MCA territory. The prevalence of accessory MCA is <0.5% in DSA.[3] If the bifurcation of MCA occurs within 5 mm from the origin, it is called as early bifurcation.[4] Association of aneurysm with duplicated MCA, accessory MCA, and early bifurcation, especially with the early frontal branch, has been reported. The etiological factors described for the association of aneurysm with these anomalous arteries are remnant of embryonic artery, defect in the medial membrane, degeneration of arterial wall, and hemodynamic stress.[4]
Because the MCA in our case bifurcate into two divisions at 0.5 cm from its origin, it can be termed as early bifurcation as per the conventional classification. However, the two divisions of MCA further divided into another two branches, one going toward the frontal region and other toward the temporal region. Although one was dominant, both had similar pattern of branching and course parallel to each other along the left sylvian fissure. Therefore, we considered it different from the category of early bifurcation and other anomalous MCA described previously [Figure 2]. Hence, we termed this as twin MCA.
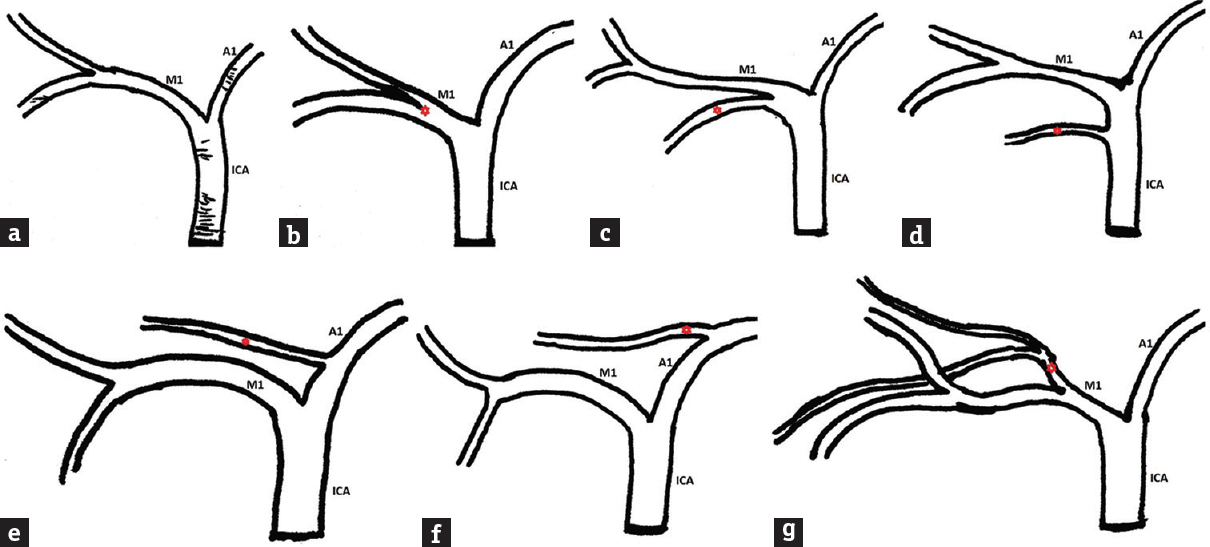
- (a) Sketch showing the normal bifurcation of middle cerebral artery. (b) Early bifurcation of middle cerebral artery. (c) Type 1 duplication of middle cerebral artery. (d) Type 2 duplication of middle cerebral artery. (e) Accessory middle cerebral artery arising from early part of A1. (f) Accessory middle cerebral artery arising from the late part of A1. (g) The present anomalous twin middle cerebral artery (note the anomalous arteries are marked as red stars, ICA: Internal carotid artery, A1: precommunicating segment anterior cerebral artery, M1: prebifurcation middle cerebral artery)
Embryologically, the MCA develops from the primitive ICA as small buds arranged in plexiform manner at the 11–12 mm embryological stage. Later on, at the 16–18 mm stage of embryo, the plexi fuses into a single MCA.[3] Possibly, the persistence of some of the fetal branches resulted in this type of anomalous MCA. The inherent weakness of the anomalous arterial wall predisposes them to the risk of aneurysmal dilatation. The aneurysm in this case also morphologically different as it had a definite sac with fusiform dilatation of the proximal arterial segment. Hence, it was difficult to analyze the nature of the aneurysm on CTA though it clearly depicted the anomalous arterial architecture. Furthermore, on DSA, the sac of the aneurysm was identified and surgical clipping of aneurysm was planned. Sylvian fissure dissection in these cases is technically demanding as injury to any individual cortical branch may produce additional deficit. Intraoperative identification of the branch having aneurysm when it is present more distally like in our case is of paramount importance. Usually, the lenticulostriate branches arise from the proximal portion of the MCA or early branches. Hence, the distal location of aneurysms here favors the application of temporary clip without compromising the lenticulostriate branches.
Preoperative assessment of individual arterial architecture is therefore highly essential in planning the surgery, especially while dealing cases of ruptured aneurysm with anomalous MCA. Judicious application of temporary clip and sharp sylvian fissure dissection will prevent injury to the lenticulostriate arteries or other major cortical branches.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Middle cerebral artery duplication: Classification and clinical implications. J Korean Neurosurg Soc. 2011;49:102-6.
- [Google Scholar]
- Management of aneurysms at the origin of duplicated middle cerebral artery: Series of four patients with review of the literature. World Neurosurg. 2013;80:e313-8.
- [Google Scholar]
- A functional perspective on the embryology and anatomy of the cerebral blood supply. J Stroke. 2015;17:144-58.
- [Google Scholar]
- Accessory middle cerebral artery and duplication of middle cerebral artery – Terminology, incidence, vascular etiology, and developmental significance. Neurol Med Chir (Tokyo). 1992;32:262-7.
- [Google Scholar]






