Translate this page into:
Tuberculosis: A Common Infection with Rare Presentation, Isolated Sellar Tuberculoma with Panhypopituitarism
Address for correspondence: Dr. Vivek Mahesh Agrawal, Department of Neurosurgery, Superspeciality Hospital and Government Medical College, Nagpur, Maharashtra, India. E-mail: vivekmaheshagrawal21@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Isolated sellar tuberculoma is a very rare condition and usually presents with headache and decreased vision. It can present with panhypopituitarism with 3rd nerve palsy. Tuberculoma mimics pituitary adenoma clinically as well as radiologically and requires endoscopic transsphenoidal surgery and histopathological examination for the final diagnosis. We present a rare case of a 40-year-old female presented with headache, decreased vision, and unilateral 3rd nerve palsy with panhypopituitarism.
Keywords
Endoscopic transsphenoidal surgery
histopathology
panhypopituitarism
sellar tuberculoma
INTRODUCTION
Tuberculosis (TB) is a very common infection that involves all age groups and all organs. TB of the central nervous system can occur at any site. In developing countries like India, tuberculoma constituted up to 30% of space-occupying intracranial lesions until recently. Now, intracranial tuberculoma accounts for 0.15%–4% of intracranial space-occupying lesions after the development of antituberculosis drugs.[1] Isolated sellar tuberculoma is very rare, with seventy cases reported all over the world.[23]
CASE REPORT
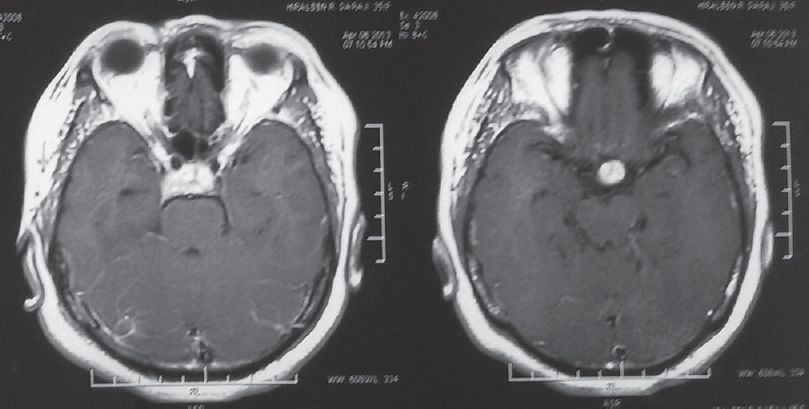
A 40-year-old female patient presented with chief complaint of headache for the last 3 months. She had also complaints of gradual decreased in vision in the right eye for 2 months. On examination, the patient was conscious, oriented, vitally stable with right temporal hemianopia with visual acuity 6/24 in the right eye and 6/6 in the left eye. The patient had developed right eye ptosis after admission. Other cranial nerves were normal, and there was no other neurological deficit. Hormone profile was as follows: prolactin - 3.97, cortisol - 0.42, growth hormone - 0.309, follicle-stimulating hormone - 2.59, luteinizing hormone - 0.26, thyroid-stimulating hormone - 0.4, free triiodothyronine - 1.92 (FT), and free thyroxine - 0.75. On magnetic resonance imaging (MRI) scan, there was intense homogeneously enhancing lesion on T1-weighted (W) contrast study of size 13 mm × 20 mm, 20 mm × 12 mm, 17 mm × 19 mm in the sellar region. The lesion was isointense on T1W and heterogeneous hyperintense on T2W extending into supra-sellar cistern with mild superior displacement of optic chiasma. Pituitary stalk was thickened. The lesion causes lateral displacement of the intracavernous segment of the right internal carotid artery [Figures 1-6]. Preoperative treatment was started with dexamethasone and thyroxin. The lesion was partially excised through endoscopic endonasal transsphenoidal approach under glucocorticoid coverage with reconstruction of sella with fat, fascia lata, and fibrin glue as the tumor had firm consistency and was adherent to the surrounding structure. The postoperative period was uneventful except for diabetes insipidus for few days, which was managed conservatively. Postoperatively, headache disappeared and vision improved in the right eye. Histopathology revealed caseating granuloma, most likely tuberculoma [Figures 7 and 8]. Ziehl–Neelsen staining of the excised tissue was negative. The patient has been put on and discharged with antituberculous therapy with maintenance dose of dexamethasone and thyroxin. Steroid has been tapered and discontinued in the follow-up. 3rd nerve palsy improved in the follow-up, and the patient is doing well and has been on antituberculous therapy and thyroxin since the last 12 months.
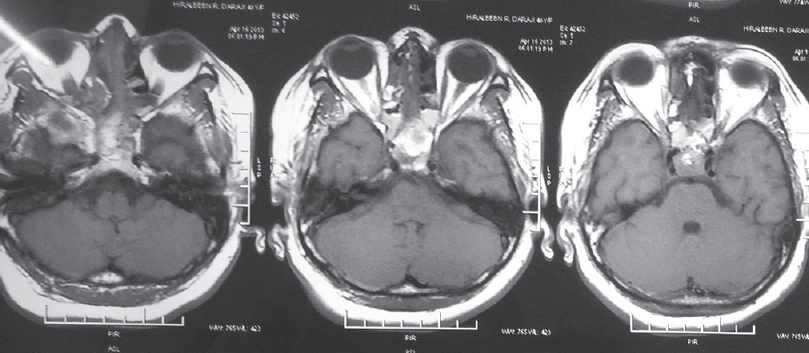
- T1 postoperative images

- Sagittal image of TI-weighted magnetic resonance imaging
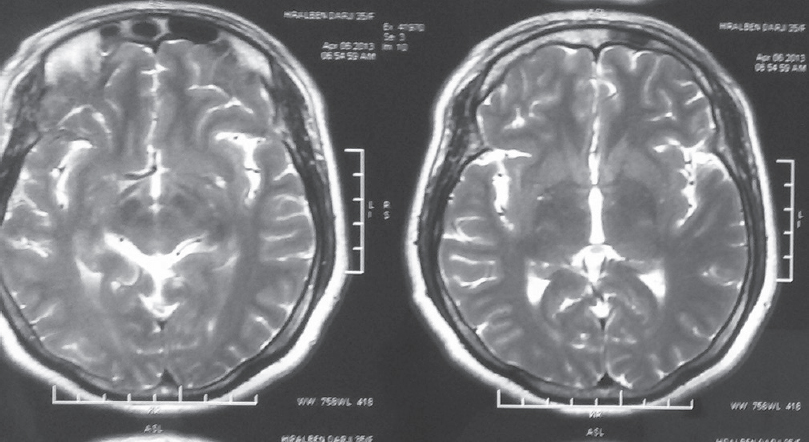
- T2 image
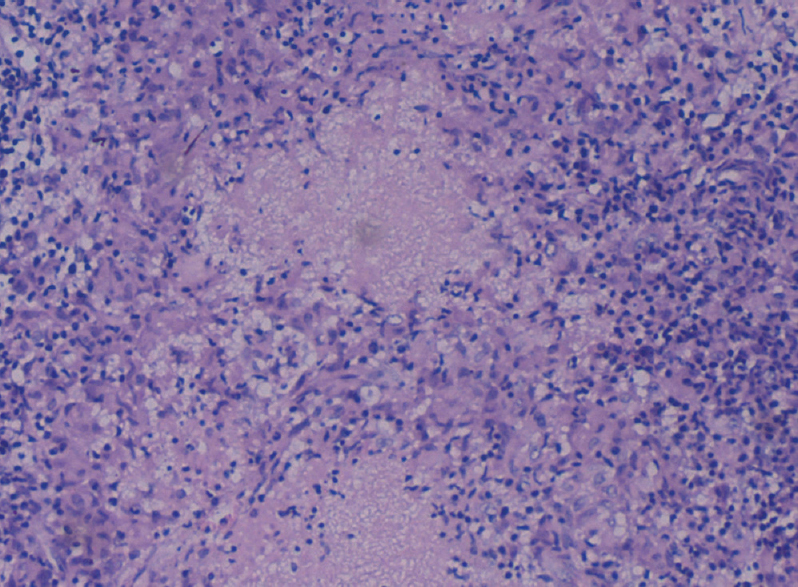
- Histopathology image with granuloma
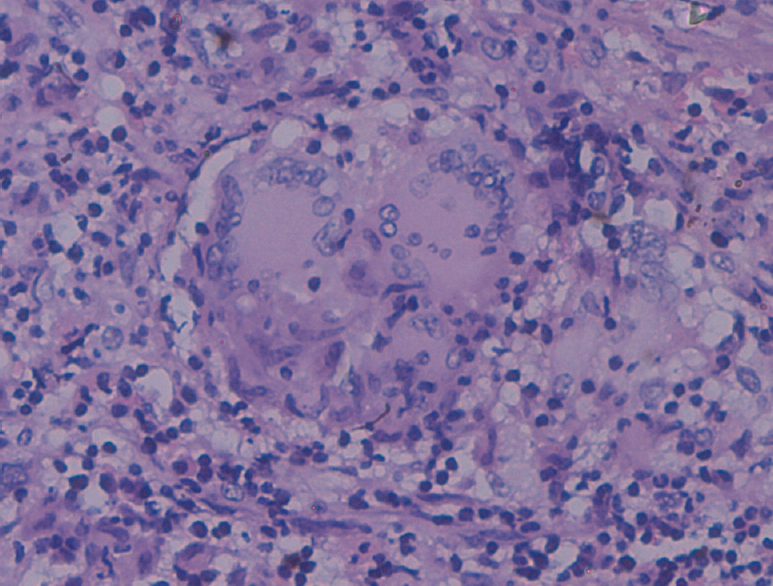
- Enlarge histopathology image
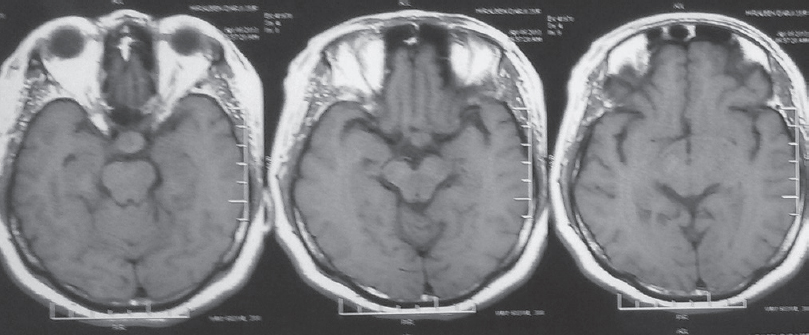
- T1-weighted image
- T1 contrast image
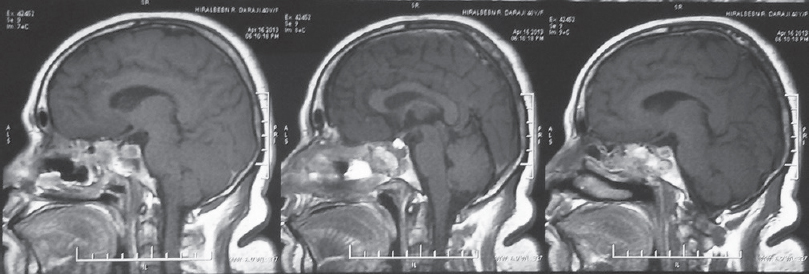
- Postoperative sagittal images
DISCUSSION
Pituitary adenomas are the most common lesion of the sellar region, but nonadenohypophyseal lesions such as TB should be considered in the differential diagnosis of the sellar masses, especially in Asian countries, particularly in India. Hypothalamic-pituitary axis tuberculomas are a very rare pathology.[4] Only few cases have been reported in the literature.[23] With the review of previous reported cases, we found headache as the most common complaint, followed by decreased or loss of vision. There is female preponderance with age ranging from 8 to 43 years (average 23.6). Endocrinological evaluation varies from hypopituitarism to hyperprolactinemia.[3] Radiologically, pituitary tuberculoma resembles adenoma, and it is very difficult to put a direct diagnosis of tuberculoma, especially if no previous history of pulmonary TB is present. Usually, tuberculoma appears isointense on T1W and has homogeneous contrast enhancement on postcontrast MRI. On T2W sequence, tuberculoma can have heterogeneous hyperintense appearance. Thickening of the stalk is seen characteristically in pituitary tuberculoma; however, it is a nonspecific finding and can also occur in other conditions such as inflammatory diseases such as sarcoidosis, syphilis, granulomatous hypophysitis, and eosinophilic granuloma.[156] Intrasellar tuberculoma can also present as apoplexy, subarachnoid hemorrhage as well as sellar floor erosion. Other MRI findings in pituitary tuberculoma include adjacent dural enhancement, peripheral ring enhancement, and sellar/suprasellar calcification.[5]
Since the diagnosis of pituitary TB cannot be established with certainty based on clinical and radiological features alone, surgery is required to get tissue diagnosis as well as to decompress the optic chiasma and surrounding structure.[7] Since transsphenoidal route avoids cerebrospinal fluid contamination and tuberculous meningitis, the procedure of choice for pituitary tuberculoma is endoscopic endonasal transsphenoidal excision of the lesion.[4] Other option is subfrontal approach after craniotomy. Intraoperatively, tuberculoma is usually found to be adherent to the surrounding structure and is nonsuckable, making it difficult to excise completely.
Histopathological examination is required to make the final diagnosis. Caseating granuloma differentiates TB from other causes of granulomatous inflammation of the pituitary such as sarcoidosis, Langerhans histiocytosis as well as lymphocytic hypophysitis. Acid-fast bacilli may not be seen on Ziehl–Neelsen staining. Polymerase chain reaction technique can be used in cerebrospinal fluid and specimen for the diagnosis.
All patients with pituitary TB require anti-tuberculosis drug treatment for 18-month duration although there is no general agreement on the duration of treatment as the site is very rare. Our patient has been put on four antituberculosis drugs (isoniazid, rifampicin, ethambutol, and pyrazinamide) for the first 2 months, and then, two drugs (isoniazid and rifampicin) for the remaining 16 months. The response to medication is excellent as in our case.[78] The effect of antituberculosis drugs on hormone profile is not known as previous reports have not given enough information regarding the same; however, one case report has mentioned the normalization of prolactin and improvement of diabetes insipidus on antituberculous treatment without any specific hormone replacement.[7] Our patient is still taking thyroxin for hypothyroidism.
CONCLUSION
Isolated sellar tuberculoma is a very rare pathology and difficult to diagnose on clinical and radiological ground as it mimics pituitary adenoma. Transsphenoidal surgery is required for tissue diagnosis as well as for decompression of vital neural structure. Tuberculoma as a differential diagnosis should be kept in mind when surgeon comes across a firm, adherent, nonsuckable, and relatively avascular tumor. Histopathological examination is required for the final diagnosis. Antituberculosis treatment has good response after surgery. Periodic follow-up is required for the assessment of hormone profile of the patient and may require lifelong replacement.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Thickening of the pituitary stalk: A finding suggestive of intrasellar tuberculoma? Case report. Neurosurgery. 1995;36:1013-5.
- [Google Scholar]
- Intrasellar tuberculoma – An enigmatic pituitary infection: A series of 18 cases. Clin Neurol Neurosurg. 2000;102:72-7.
- [Google Scholar]
- Pituitary granuloma and chronic inflammation of hypophysis: Clinical and immunohistochemical studies. Acta Neurochir (Wien). 1993;121:152-8.
- [Google Scholar]
- Tuberculomas of the hypophysis cerebri: Report of five cases. J Clin Neurosci. 2003;10:562-6.
- [Google Scholar]
- Suprasellar tubercular abscess presenting as panhypopituitarism: A common lesion in an uncommon site with a brief review of literature. Pituitary. 2006;9:73-7.
- [Google Scholar]






