Translate this page into:
Trend of Neuropsychiatric Morbidity in Sub-Himalayan Region: An Audit of Retrospective Data Mining
Address for correspondence: Dr. Mitasha Singh, Department of Community Medicine, ESIC Medical College and Hospital, Faridabad - 121 001, Haryana, India. E-mail: mitasha.17@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
There is a paradigm shift in health loss due to premature mortality and disability from neuropsychiatric disorders with major burden in low- and middle-income countries.
Objective:
To study the trend of admissions with neuropsychiatric and substance-use disorders in 3 years in psychiatry and medicine wards of tertiary care hospital in rural Himachal Pradesh.
Methodology:
A retrospective data mining was done from records of Inpatient wards of Dr. R. P. Government Medical College, Tanda, Himachal Pradesh, for the year 2013–2015. Demographic details and diagnosis of neuropsychiatric disorders, licit and illicit drug use, and their consequences in the form of hanging and poisoning were analyzed.
Results:
Majority of admissions were attributed to alcohol abuse which increased in 3 years significantly in the months of July–September (P = 0.02) and October–December (P = 0.00). Almost all cases of neuropsychiatric disorders and majority of poisoning (58.2%) were observed among females. The productive young and middle age group (21–40 years) was mostly affected by all cause neuropsychiatric disorders (80.9%) and presented with poisoning (66.2%). Illicit drug abuse was on increasing drift among females.
Conclusion:
Indoor admissions were attributed to alcohol use and poisoning while neuropsychiatric disorders and substance abuse were probably dealt with at outpatient level. Treatment pertaining to mental illnesses was sought in severe cases only. Data demonstrating population burden are needed urgently to address the barriers to treatment to reduce burden.
Keywords
Neuropsychiatric disorder
tertiary center
trend analysis
INTRODUCTION
The World Health Organization (WHO) defines mental health as not just the absence of illness, rather it is conceptualized as a state of well-being in which the individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her community.[1] Recent data from the global burden of diseases (GBD) demonstrate the magnitude of the burden of mental and behavioral disorders (2010) as 7.4% of DALYs worldwide that significantly increased from 1990 as 5.4%. In 2013, mental, neurological, and substance-use disorders accounted for 31 million DALYs in India (6% of all disease burden).[2] The magnitude and costs of mental health and disorders are relatively neglected,[3] in spite of growing health challenge. In the existing structures into which mental health services fit, there is continued dominance of large psychiatric hospitals in many countries including India. Decentralizing and deinstitutionalizing the mental health has been an agenda of the National Mental Health Programme and the District Mental Health Programme since their inception. Furthermore, it has discussed about the integration between the community and hospitals, and appropriate referral systems incorporating secondary and tertiary care.[45] However, due to shortage of workforce and inadequate infrastructure, the role of tertiary hospitals in provision of primary to tertiary care in form of specialized beds remains important.[6] Himachal Pradesh like any other states of the country focuses its workforce and infrastructure on combating communicable diseases with stress on maternal and child health programs. The neuropsychiatric disorders and substance abuse remains a neglected entity. In the above scenario, the present study aimed to conduct a retrospective data mining of neuropsychiatric disorders, licit and illicit substance use, and their consequences of suicidal or homicidal poisoning and hanging in consecutive 3 years (2013–2015) among inpatients in a tertiary care center in rural setting.
METHODOLOGY
A retrospective data mining of three consecutive years (2013 through 2015) was conducted at the inpatient wards of a tertiary care center of Dr. Rajendra Prasad Government Medical College, Kangra at Tanda, Himachal Pradesh. Records of adult patients admitted to the Inpatient Department of Medicine and Psychiatry and those referred from other specialties to the Department of Psychiatry for the management of deaddiction and evaluated by the consultant psychiatrist were retrieved. The recorded data included age, gender, residence, month of admission, and outcome of patient in terms of death during stay at hospital.
Inclusion criteria
Neuropsychiatric cases and substance-use disorders were diagnosed according to the 10th revision of International Classification of Diseases during inclusion in the data.[7] Further, homicidal or suicidal poisoning and hanging cases, admitted as a consequence of neuropsychiatric illnesses or as a result of substance use, were also included.
Exclusion criteria
Admissions due to mental retardation were excluded from the study.
Data collection procedure
Ethical approval and due permission were obtained from the institutional ethics committee. Prior formal administrative approval was sought from the concerned authorities and medical records department of the institute. Initial screening of records was done by a research fellow of the institute under supervision of the principal investigator with the help of personnel of medical records department. The final listing of cases was done by the residents of community medicine, also the coinvestigators.
Data analysis
Data were entered into Microsoft excel sheet (2003–2007), and trends of different illnesses were computed as proportion. The trend analysis was done with Chi-square test for trend at the alpha level of 5% statistical significance.
RESULTS
Gender distribution of the patients attending tertiary care center for neuropsychiatric illnesses and substance-abuse disorder showed that males predominated with variety of illnesses; with approximately 70% attendance throughout these 3 years under study. Majority of neuropsychiatric admissions were during summer (April–June); 33% in 2013, 28% in 2014 and 22% in 2015; majority were from district Kangra (more than one third every year) probably due to geographical location. Deaths among inpatients due to neuropsychiatric disorder or substance abuse was maximum in 2014 (7%) and minimum in 2015 (4.1%).
Neuropsychiatric disorder
Depression and conversion disorders were reported in highest numbers among 21–40 years’ age group, during monsoon and autumn seasons with an insignificant decreasing trend in these 3 years under study period. Females dominated the diagnosis with depression, anxiety, and conversion disorders all through these 3 years [Table 1].

Licit drug use
There was dominance of alcoholics (more than half in all 3 years) with an upward trend (54.8% to 56% from 2013 to 15); incidentally also high in 21–40 years of age group in these years with an upward trend (44.3% to 47%); yet majority of alcohol users belonged to 41–60 years’ age group with an increasing trend from 2013 to 15. Alcohol use as cause of admission was dominated by males though no significant trend was noted in 3 years. Summer season observed a significant decline in proportion of alcohol use, and autumn (October–November) season observed a significant rise in proportion (19%–46%) from 2013 to 2015. Alcohol use and poisoning in all the 3 years were reported in majority from Kangra with no significant trend in proportion. Cases were also reported from neighboring districts such as Chamba, Hamirpur, and Mandi. State of Punjab borders Himachal Pradesh and patients’ resident of Punjab reported with alcohol use, with an increasing trend. Among the alcoholics who reported at tertiary center and died, 32.5% died in 2013 which increased in 2014 and declined to 27.5% in 2015 [Table 2].
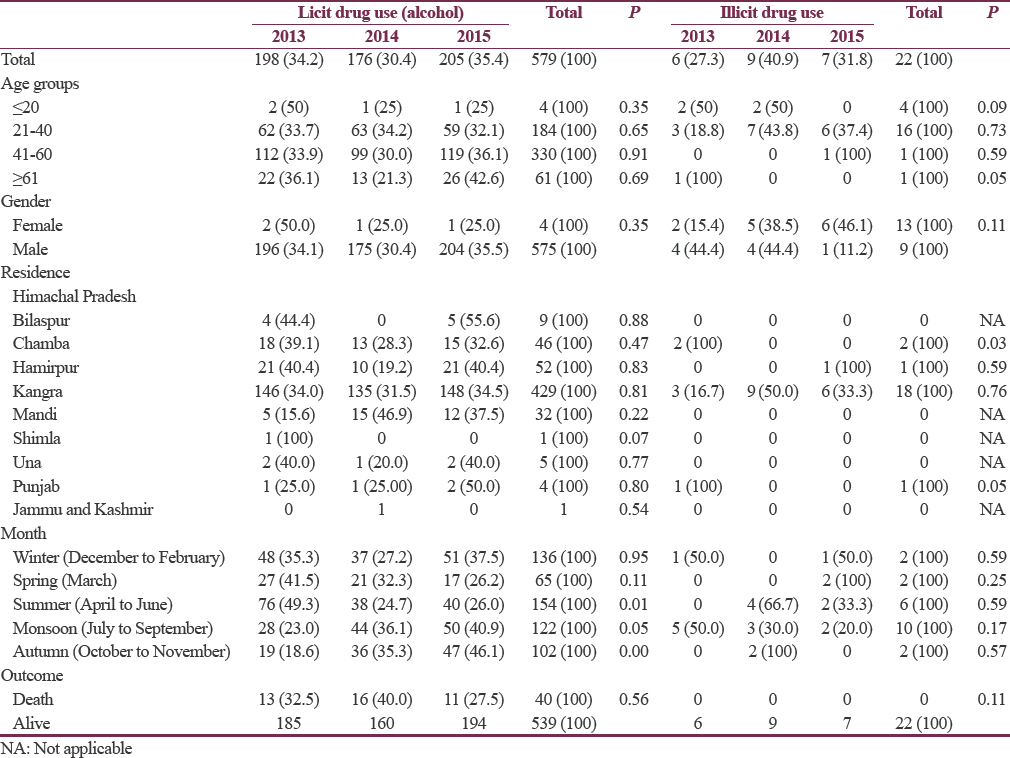
Illicit drug use
Illicit drug users were noted in majority from 21 to 40 years’ age group without any significant trend, noted higher in females with an increasing trend over the 3 years (30.7% increases). Majority of drug users were reported during summer and monsoon (July to September) though there was decreasing trends through 3 years (P = 0.59 and 0.17, respectively). There was a notably high influx of cases from neighboring state of Punjab which may be a reason [Table 2].
Hanging
Hanging cases were observed in majority among 21–40 years’ age group without any significant trend. Females dominated the history of hanging over these 3 years. Majority of cases of hanging were residents of district Kangra and the second highest proportion of cases reported from Hamirpur, the neighboring district and showing a declining trend in 3 years (28% decline, P = 0.06) [Table 3].
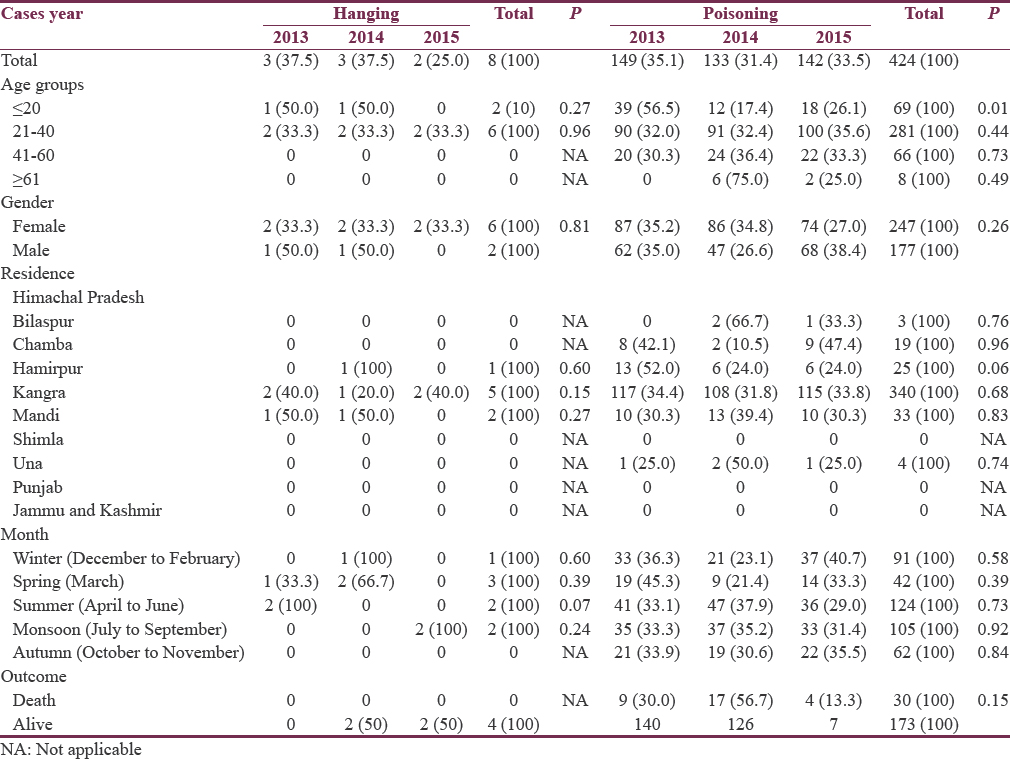
Poisoning
Homicidal/suicidal poisoning cases attributed to second highest number of cases being admitted with a decreasing trend in 3 years (41.3%–38.8%, P = 0.63); a higher proportion of poisoning also belonged to younger age group (21–40 years) in all the 3 years. A sharp decline (39.1%) was observed in the poisoning cases reported among ≤20 years’ age group from 2013 to 2014 which further increased by 8.7% in 2015, the trend being statistically significant (P = 0.01). Poisoning was diagnosed more among females with a decreasing trend of proportion in 3 years (P = 0.26). Poisoning cases were in majority reported during summer and spring (March) season with a declining trend in proportion of cases through the 3 years [Table 3].
DISCUSSION
India accounted for 15% of the global mental, neurological, and substance-use disorder burden.[8] A systematic review of epidemiological studies on psychiatric morbidity in India reported that the prevalence rates of psychiatric disorders vary across the populations and time.[9] This was evident in this trend analysis over 3 years in the same population of a Sub-Himalayan region. Also in India, the treatment-seeking behavior of a patient is sensitive to seasonal and environmental conditions, which varies with different regions.[10]
Neuropsychiatric disorders
In the current analysis, only 1% of all admissions were attributable to depressive disorders in 2013 which further decreased and anxiety disorders attributed even less. All of the depressive and anxiety disorders admissions were females involving 21–60 years’ age group. GBD study reports that depressive disorders and anxiety disorders accounted for more than half (52%) of DALYs in India in working-age adults (aged 20–69 years). It also supports our findings with proportion of depression and anxiety burden being consistently higher in women (63% in India) which consume most mental health resources.[11] A higher prevalence of 28.4% through screening was also reported among primary care attendees in South India and 21.7% among the Outpatient Department of Psychiatry of a tertiary care center of Delhi.[1213] Shahid et al. reported that 30% of all psychiatry cases who reported in emergency department were attributed to depressive disorders. However, many of these patients who were advised admission left against medical advice due to financial and stigma related issues.[10] Similarly, the outpatient attendance of these disorders may have been high in our institute also; however, since we focused on admissions due to morbidities or injuries related to these disorders, the proportion decreased in our analysis.
The peak incidence of patients with mood disorders in a study conducted at a tertiary center of Chandigarh in North India was observed from May to July (summer), attributed to high mean daily temperature and heat waves.[14] In an analysis from a mental hospital of Vietnam, a positive association between temperature and admissions for mental disorders and substance abuses in the month of June when the weather is at its hottest has been reported.[15] However, in our study, these cases were observed in majority during monsoon and autumn (July to November). Probably because in Himachal Pradesh during sowing and cutting of rabi and kharif crops, people are busy and the attendants of patients with neuropsychiatric disorders generally postpone their visit to health centers.
Licit drug use
Our study noted that more than half of inpatients were attributed to alcohol use with increasing trend. This was in contrast to disease burden study (GBD), 2013, which reported that alcohol abuse explained only 5% of all mental, neurological, and substance-use disorder burden in both China and India. However, India observed a 64% increase in DALYs attributed to alcohol-abuse disorders from 1990 to 2013.[11] One of the reasons could be that majority of the injuries and comorbidities which were diagnosed, admitted, and managed in a tertiary care center were attributed to alcohol abuse for obvious reasons. The fact is supported by Risal and Tharoor who in their comparative analysis of secondary and tertiary center of Karnataka reported that 81.6% of alcoholics present with different medical morbidities of which majority presented to tertiary center.[16] This may be due to the frequent use of radiological and other investigation facilities as well as the presence of a well-coordinated consultation services at tertiary centers. GBD study, in contrast, was conducted on regional prevalence data.[11] Majority of alcohol abuse was observed among middle age group (41–60 years). The age distribution was similar to a study conducted in a tertiary care center of North India with a significant increasing trend in 3 years (2008–2010).[17] Studies from the West also reported high likelihood of alcohol use among older adults.[18] With the increase in life expectancy, middle age is likely to constitute a larger fraction of treatment seekers in the coming years. In the current analysis, majority of patients with alcohol abuse and its complications were observed during summer months of North India. Similar observations have been made in western world which linked human behavior and their thermal environment,[192021] due to change in neurotransmitters and thermoregulation with change in ambient temperature.[22]
Illicit drug use
Illicit drug use was observed in our study to have an increasing trend among young and middle age females. GBD study reported higher number of DALYs of substance-abuse disorders from India among males in 2013 and had projected an almost equal percentage of increase in abuse among both genders over the next decade.[11] Substance use was reported among 3% of psychiatry cases reporting in emergency department of a tertiary center of Karachi, but admissions were reported to be higher among females.[10] Females tend to avoid treatment seeking and retaining early during initiation of substance abuse due to homemaking responsibilities, social stigma, a substance-abusing spouse, a male-oriented treatment system, and mental health diagnose, and hence, admitted late with complications.[2324] National data consistently documented a comparative lower prevalence of substance-use disorders among middle-aged individuals among general population in contrast to our findings. However, in the first National Survey in India, 30% of all current users of psychoactive substance were 40 years or more.[25] One of the probable reasons could be initiation of substance abuse in younger age group and presentation with adverse effects in middle age. Illicit substance-abuse disorders were observed during both summer and monsoon season. A study from a tribal district of Andhra Pradesh reported majority of patients with substance use from December to May, stating that during this period, the population here is free from sowing, reaping, and selling of crops.[26]
Poisoning and hanging
Poisoning cases attributed to second highest number of cases with majority in 21–40 years’ age group being admitted with a decreasing trend in our study period. Poisoning in many situations is outcome of some form of psychiatric morbidity with which a patient suffers. Hanging as a mode of suicide was observed in around 1% of cases with no change in trend. Maharani and Jailkhani et al. in their analysis of poisoning cases from a tertiary care center in Tamil Nadu and Maharashtra reported that associated comorbid conditions such as schizophrenia, depression, anxiety, adjustment disorder, and alcoholism were found in around 23 and 13% of cases, respectively.[2728] They also reported that poisoning was common among productive age group (20–30 years) that produces a huge socioeconomic burden on the society. Proportion of females with poisoning outnumbered males in our study, but an increasing trend was observed among males. Women outnumbered males in a study at tertiary center of Kerala also[29] in contrast to other Indian studies where proportion of males consuming poison was higher.[27283031] Factors such as dowry, cruelty by the in-laws, family quarrels, maladjustment in married life, and dependence of women on husband could be responsible for the higher incidence of poisoning among young middle age females in our study area which is a rural area.[27]
In India, overall population growth explains a greater proportion of the change in mental, neurological, and substance-use disorder burden from 1990 to 2013 (44%). Population growth and aging have pivotal roles in the dynamic changes of disease burden, exemplified by the major shifts from communicable to noncommunicable and acute to chronic diseases being noted worldwide. India has begun implementing several new approaches to address the treatment gap. These range from tackling the shortage of workforce through a task-sharing approach,[32] continuum of care approach in the community,[33] to technological innovations.[34] For a number of people with severe mental disorders, hospitalization is required at some point in their lives. District general hospitals and tertiary care centers provide an accessible and acceptable location for 24-h medical care and supervision of people with acute worsening of mental disorders, in the same way that these facilities manage acute exacerbations of physical health disorders.[35]
Strengths of the study
Early detection through active screening and monitoring of mental health is a far sighted approach to respond to the challenge of a rising mental, neurological, and substance-use disorder burden. We aimed to sensitize stakeholder of neuropsychiatric disorders, licit and illicit substance use, and their consequences of suicidal or homicidal poisoning and hanging.
Limitations of the study
To find the trend cohort study is needed over longer period that is lacking in this study.
Future directions of the study
Epidemiology of any disease or condition is the basis of formulation of its prevention strategies. The country still lacks an efficient system to report the exact prevalence of mental health disorder. The true burden of mental disorders still remains underestimated in India with no nationally representative epidemiological data available for which we need to strive.
CONCLUSIONS
To sum up, indoor admissions were attributed to alcohol use and poisoning while neuropsychiatric disorders and substance use were probably dealt at outpatient level to reduce inpatients’ burden. Community-based interventions will usher long-term solutions for prevention, early treatment, addressing barriers to treatment with data demonstrating population burden.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 2016. Mental Health: Strengthening our Response. Fact Sheet. Geneva: World Health Organization; Available from: http://www.who.int/mediacentre/factsheets/fs220/en/
- Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2197-223.
- [Google Scholar]
- Strengthening evidence for mental health promotion. Health Promot Int. 2011;26:140-6.
- [Google Scholar]
- Director General of Health Services (DGHS): National Mental Health Programme for India. New Delhi: Ministry of Health and Family Welfare; 1982.
- NIMHANS. District Mental Health Program. Available from: http://www.nimhans.kar.nic.in/%E2%80%A6/default.htm% 00%00
- Mental Health Policy and Service Guidance Package. Organization of Services for Mental Health. Geneva: WHO; 2003.
- World Health Organization. ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva: WHO; 1992.
- Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990-2013: Quantifying the epidemiological transition. Lancet. 2015;386:2145-91.
- [Google Scholar]
- Profile of psychiatric patients presenting to a tertiary care emergency department of Karachi. J Coll Physicians Surg Pak. 2015;25:386-8.
- [Google Scholar]
- The burden of mental, neurological, and substance use disorders in China and India: A systematic analysis of community representative epidemiological studies. Lancet. 2016;388:376-89.
- [Google Scholar]
- Common mental disorders among primary care attenders in Vellore, South India: Nature, prevalence and risk factors. Int J Soc Psychiatry. 2003;49:119-25.
- [Google Scholar]
- Current scenario of psychiatric diagnosis in a tertiary care teaching hospital. Delhi Psychiatry. 2012;15:107-10.
- [Google Scholar]
- Seasonal pattern of psychiatry service utilization in a tertiary care hospital. Indian J Psychiatry. 2007;49:91-5.
- [Google Scholar]
- Seasonality of hospital admissions for mental disorders in Hanoi, Vietnam. Glob Health Action. 2016;9:32116.
- [Google Scholar]
- A cross-sectional comparison of drinking patterns, alcohol use and related medical morbidities in a secondary versus tertiary setting. Kathmandu Univ Med J (KUMJ). 2013;11:152-7.
- [Google Scholar]
- A retrospective chart review of treatment seeking middle aged individuals at a tertiary care substance use disorder treatment centre in North part of India over five successive years: Findings from drug abuse monitoring system. ScientificWorldJournal 2013 2013:316372.
- [Google Scholar]
- Geriatric patients on a substance abuse consultation service. Am J Geriatr Psychiatry. 2002;10:337-42.
- [Google Scholar]
- The effect of heat waves on mental health in a temperate Australian city. Environ Health Perspect. 2008;116:1369-75.
- [Google Scholar]
- Psychological responses. Thermal Environments the Effect of Hot Moderate and Cold Environments on Human Health Comfort and Performance (2nd ed). London: The Taylor & Francis; 2003. p. :47-68.
- The relationship of environmental temperature to the incidence and outcome of schizophrenia. Br J Psychiatry. 1992;160:788-92.
- [Google Scholar]
- Central fatigue and neurotransmitters, can thermoregulation be manipulated? Scand J Med Sci Sports. 2010;20(Suppl 3):19-28.
- [Google Scholar]
- Gender differences in predictors of initiation, retention, and completion in an HMO-based substance abuse treatment program. J Subst Abuse Treat. 2002;23:285-95.
- [Google Scholar]
- Course, severity, and treatment of substance abuse among women versus men. Am J Drug Alcohol Abuse. 2000;26:523-35.
- [Google Scholar]
- The Extent, Pattern and Trends of Drug Abuse in India- National Survey, Ministry of Social Justice and Empowerment. Government of India and United Nations Office on Drugs and Crime 2004
- [Google Scholar]
- Profile of poisoning cases in a tertiary care hospital, Tamil Nadu, India. J Appl Pharm Sci. 2013;3:91-4.
- [Google Scholar]
- Retrospective analysis of poisoning cases admitted in a tertiary care hospital. Int J Recent Trends Sci Technol. 2014;10:365-8.
- [Google Scholar]
- One-year study on pattern of acute pharmaceutical and chemical poisoning cases admitted to a tertiary care hospital in Thrissur, India. Asia Pac J Med Toxicol. 2015;4:79-82.
- [Google Scholar]
- Epidemiology of insecticide poisoning at A.I.I.M.S Emergency service and role of its detection by gas liquid chromatography in diagnosis. Medicoleg Update. 2007;7:49.
- [Google Scholar]
- The epidemiology of poisoning: An Indian view point. J Forensic Med Toxicol. 2002;19:5-11.
- [Google Scholar]
- Effectiveness of an intervention led by lay health counsellors for depressive and anxiety disorders in primary care in Goa, India (MANAS): A cluster randomised controlled trial. Lancet. 2010;376:2086-95.
- [Google Scholar]
- Effectiveness of a community-based intervention for people with schizophrenia and their caregivers in India (COPSI): A randomised controlled trial. Lancet. 2014;383:1385-94.
- [Google Scholar]
- Telepsychiatry in Chennai, India: The SCARF experience. Behav Sci Law. 2008;26:315-22.
- [Google Scholar]
- World Health Organization. Improving Health Systems and Services for Mental Health. Geneva: WHO; 2009.






