Translate this page into:
Treatment Discontinuation in Schizophrenia: A Qualitative Exploration from a Rural South Indian Community
Address for correspondence: Dr. K. Shanivaram Reddy, Department of Psychiatric Social Work, National Institute of Mental Health and Neurosciences, Bengaluru, Karnataka, India. E-mail: shanivaramreddyk@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Medication discontinuation remains a big hurdle for retaining persons with schizophrenia under the treatment AMBIT. It is imperative to understand reasons for the same to effectively tackle it.
Methods:
The study was carried out in Turuvekere, a rural South Indian taluk (an administrative block). Qualitative interviews were conducted with consenting consecutive nineteen patients (along with their family members) who had discontinued medications. All interviews were transcribed. Enlisted reasons were then color coded to synthesize different factors. From the 16th patient onward, no new reason emerged. Three more interviews were done to ensure that there was no additional reason.
Results:
The following factors (average 4.26 factors per patient) led to medication discontinuation: (1) lack of support/supervision from family/well-wishers (n = 14/19 [73.68%]); (2) lack of insight and cooperation from the patient (n = 11; [57.89%]); (3) lack of awareness about the illness (8 [42.10%]); (4) adverse effects of medications (n = 8; [42.10%]); (5) financial factors (n = 8; [42.10%]); (6) distance/transport (n = 8; [42.10%]); (7) lack of knowledge about treatment process (n = 7; [36.84%]); (8) perceived lack of beneficial effects of treatment (n = 5; [26.32%]); (9) treatment center-related issues (n = 4; [21.05%]); and others.
Conclusions:
Medication discontinuation is driven by a diverse set of interrelated factors among community-living persons with schizophrenia. Professionals need to be aware of this complexity to effectively manage the problem.
Keywords
India
medication discontinuation
rural community
schizophrenia
INTRODUCTION
In India, the treatment gap remains alarmingly high in persons with psychiatric disorders, particularly in those who suffer from schizophrenia (Gopinath et al.; 1987).[1] Medication discontinuation, a commonly observed clinical phenomenon, could arguably be construed as one important factor behind this sorry state of affairs. That being the case, it remains essential to understand reasons/factors that drive a patient toward medication discontinuation. Only then, a comprehensive management strategy could be mounted against this public health malady. In this context, it may be noted that many researchers have pointed out the need for in-depth study of treatment adherence in community-dwelling patients (Parthasarathy et al.; 1981,[2] Kulhara et al.; 1987,[3] Sriram et al.; 1990).[4] An ideal way to asses 'medication discontinuation' is to use a scale/schedule that taps all dimensions of the problem.
There are very few studies.[5] All these were conducted in hospital settings with very small sample sizes where pre-prepared checklists were used for assessing barriers for continuing psychiatric care. In addition, these studies included “in-patients,” out-patients who attended walk-in-clinics and discharged patients, neglecting the community dwellers. A recent community-based study[6] also used a checklist for assessing reasons for remaining untreated.[7] Use of prepared checklists and interviewer directed questionnaires may fail to capture all patient/family-related factors.[8] Further, these checklists/interviews are not standardized.[9] In this context, comprehensive, qualitative studies could be ideally suited to understand these issues.
As part of developing a comprehensive tool to assess this problem in rural communities, we conducted qualitative interviews to explore factors that preclude patients and their families' from continuing the once already initiated psychiatric treatment (in all probability, only medications). This paper describes the results of this qualitative interview.
METHODS
Setting
The study was conducted in Turuvekere, a South Indian taluk (an administrative block). The taluk has a population of 1, 52,177 according to census 2011. Patients were part of a community intervention program titled “Treating Untreated Psychosis in Rural Community: Variation in the Experience of Care (TURUVECARE)” entailing identification, treatment, and follow-up of all schizophrenia patients in the taluk. The program has been running for the past 6 years.
Identification of patients
The screening was done by the health workers (n = 361) and Accredited Social Health Activist workers[10] (n = 167). They were trained by our team in administration of a simple tool called “Symptoms in others.”[11] This is a validated instrument of identifying psychiatric disorders in the community, which can be used by grass-root level health staff. These grass-root level health staff administered the tool to the households that come under their purview during their routine visits. Positive cases were referred to the study team. In addition to this, the research social workers (SKR, SKK) covered every village of the taluk with the purpose of case finding. They interviewed key informants such as school teachers, post men, cooperative society's secretaries, village accountants, owners of provision stores and tea stalls, pharmacists, kerosene merchants, and general practitioners. Once the patient was identified, enquiries were made about similar persons that they may have come across (snow-balling technique).
Diagnosis and assessments
Soon after the referral, evaluation was made by research psychiatrists using the mini-international neuropsychiatric interview.[12] Their psychopathology and disability were assessed using the positive and negative syndrome scale (PANSS);[13] and the Indian Disability Evaluation and Assessment Scale (IDEAS),[14] respectively. Consecutive patients with history of having discontinued psychiatric treatment were recruited till we achieved “saturation” of factors (see below; n = 19). We recruited one patient on any given day; if two patients were identified on the same day, then we assessed only the first patient, as interviewing two patients and their families posed practical challenges in terms of time. “Psychiatric treatment” was defined as evaluation and treatment by doctors trained in modern allopathic treatment.
After complete description of the study to the participants/family members, written informed consent was obtained. Assessments were conducted only after the consent. The study was approved by the Ethics Committee of the National Institute of Mental Health and Neurosciences.[15]
Methodology of the qualitative interviews
We were interviewed patients along with their family members. “Family members” were defined as caregivers above 18 years, living under the same roof as that of the patient at least during the past year, and being responsible for the patient's overall care. Interviews were conducted in the following four phases.
Phase I
In this phase, we asked patients/family members to come up with all possible reasons for discontinuing medications. They were also quizzed how they were managing patient's altered behavior; reactions from other family members, neighbors and their experience of having had alternative methods of treatment. This phase was conducted using open-ended questions. They were encouraged to provide as much details as possible using facilitating questions such as, “what else?,” “then what?,” and “is there anything else?”.
Phase II
In this phase, semi-directive questions were used to obtain further elaboration on each of the reasons listed by patients/family members. Examples and illustrations were provided. Discrepancies and contradictions were reflected back to obtain clarifications.
Phase III
In this phase, a more directive questioning was conducted using a list of reasons obtained from the existing literature [Box 1] focusing on such reasons for discontinuing medications. In addition, we used Phase II techniques were used to get elaboration and clarification.[INLINE:1]
Phase IV
In this phase, the patients/family members were asked to cite the most and the least important reason (from among the reasons they had already listed), which prevented them from continuing medications.
Data management and analysis
All interviews were transcribed. Color coding was done to synthesize factors. Representative quotes were selected for each of these factors. The quotes and the color codes were reviewed by authors independently to reduce biases.
Saturation of factors
Data collection and interpretation took place iteratively. Whenever a new reason emerged, it was added to the existing list (that was used in Phase III). From the 16th patient onward, no new reason emerged. Three more patients and families were interviewed to ensure that there was no additional reason. Thus, families and patients of 19 patients were interviewed.
RESULTS
Average age of the patients was 36.47 (standard deviation [SD] = 13.87; median = 32.00) years. Out of the 19 patients, 5 (26.3%) were males; 17 (89.5%) belonged to the Hindu religion; and 4 (21.1%) had high school education. Mean duration of illness was 91.89 (SD = 62.29; median = 60) months. Mean PANSS score was 88.78 (SD = 2.89), mean total IDEAS score was 11.42 (SD = 3.50), indicating moderately symptomatic and disability, respectively.
19 patients and families came up with 99 reasons (average = 4.69 reasons for one patient) that discontinued psychiatric treatment. After color coding and clarification, these reasons were synthesized into 16 factors. Table 1 shows the frequency distribution of these factors (percentage of patients/family members reporting on a particular factor.
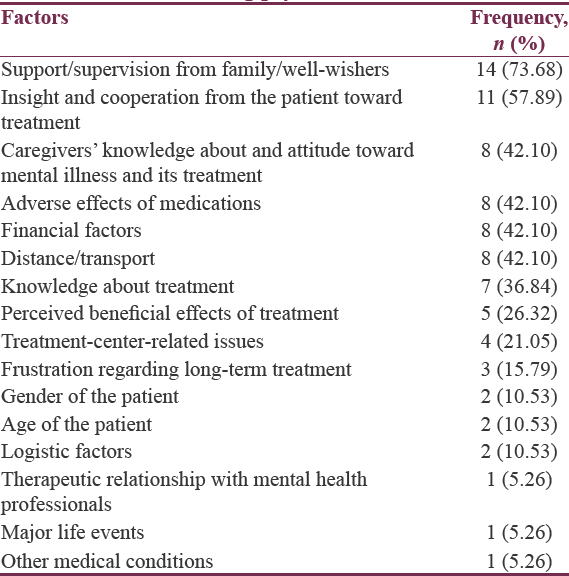
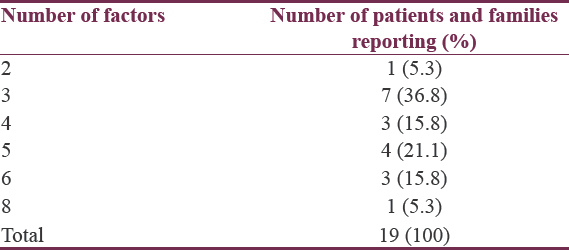
Table 2 shows the frequency distribution of the number of factors reported by patients/family members.
Following paragraph offers brief description about each factor illustrated by one or two quotes (actual quotes reported by patients/family members).
Perceived benefit of treatment-Perceived lack of effects of treatment
Perceived benefit or lack of it may influence continuity to treatment. The extent to which “perceived benefit” influenced medication-continuation in either of the directions has been subsumed here.
E.g.: Mr. P. says about his father that “After medication use, my father's improvement was unsatisfactory, his symptoms like talking to self, wandering behaviour did not improve.”
Adverse effects of medication
Experience of adverse effects of medications may have influenced the patients'/family members' decision to continue medications as prescribed or to change the dose or even to stop them.
E.g.: Mr. S. says about his wife that “Following medication, my wife was drowsy, dull, and sleeping most of the day; hence we discontinued medications.”
Frustration regarding long-term treatment
Patients and family members may have discontinued the treatment due to the sheer frustration of having to take medications continuously for days on end, which reminded them that they were “patients.” This may happen even in the context of patients experiencing substantial benefit out of treatment; however, it was more likely in those perceiving partial benefit.
E.g.: Mr. R. says about her husband that “After prolonged treatment, my family members lost hope of cure and neglected further pursuit.”
Caregivers' knowledge about and attitude toward mental illness and its treatment
Belief in alternative treatments such as Ayurveda, indigenous medicine/magico-religious treatment, may influence medication-discontinuation.
E.g.: Mr. S. says about his father “my other family members felt that the illness was due to magico-religious reasons and started to visit the faith healer.”
Knowledge about treatment-Information about mental health treatment
Patients may not continue treatment owing to poor knowledge about the dosage schedule and/or duration of treatment.
E.g.: Mrs. G. says about her husband that “My husband's family members were not keen on patient's treatment on persuasion they unwilling stated that the patient was lazy and he was feigning.”
Insight and cooperation from the patient toward treatment
This refers to the degree of insight into the psychiatric condition and the level of cooperation by the patient toward his/her treatment. Some patients may be highly cooperative for psychiatric treatment, and others may show physical/verbal aggression when told to take medications/go for psychiatric consultation. The latter may be because of a single or a combination of reasons, including (but not confined to) paranoia, general level of irritability, and lack of insight.
E.g.: Mr. R. says about his wife that “My wife was not keen on taking medication, when we persuaded her to take treatment, she would evade us or use abusive words.”
Therapeutic relationship with mental health professionals
The quality of the relationship with the treating team may have an influence on adherence. Poor therapeutic relationship would influence continuation of treatment adversely; for example, when patients do not feel that the mental health professionals are spending quality time with them or that they are not available on follow-ups etc., it could affect the quality of the therapeutic relationship [Figure 1].
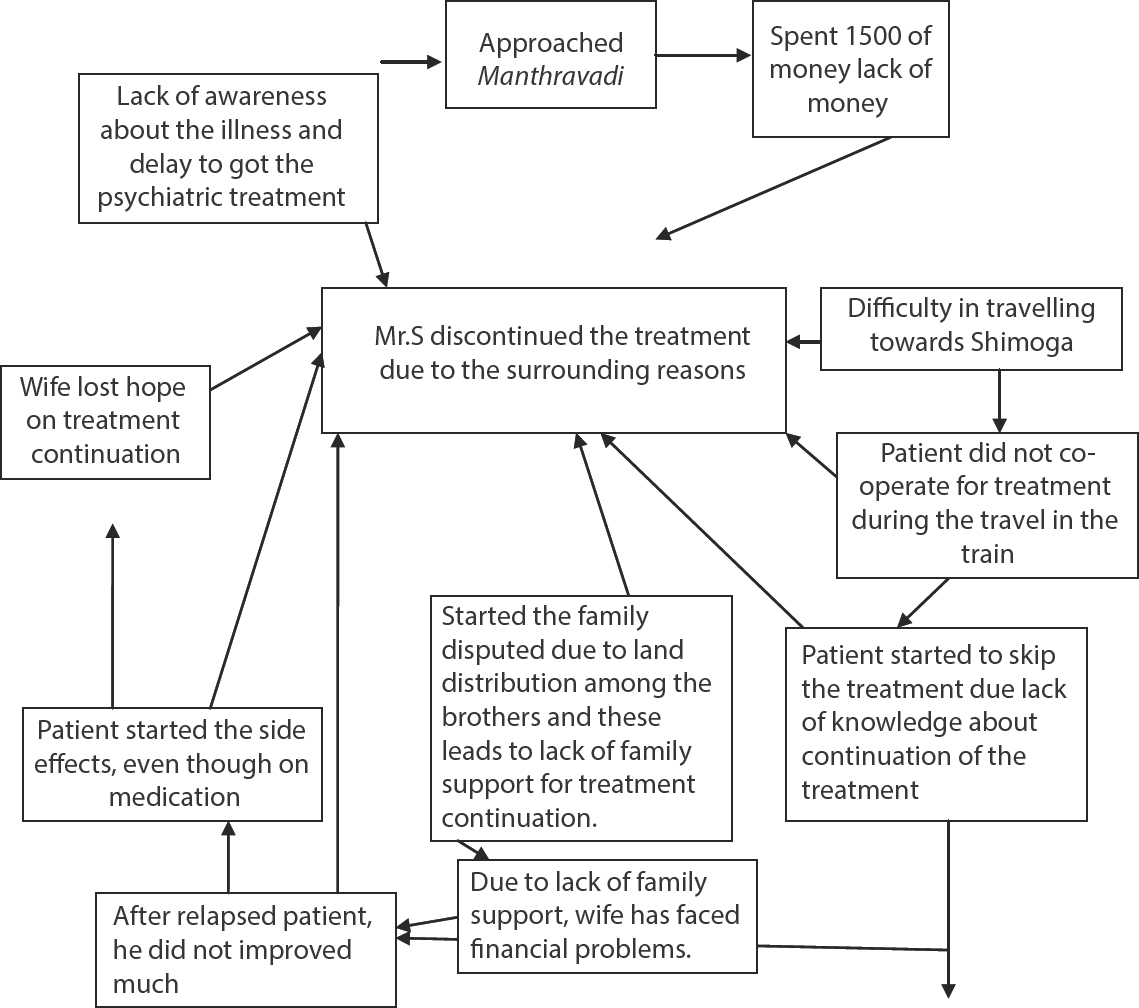
- The above figure shows the complex interplay of the reasons for discontinued the psychiatric treatment of Mr. S
E.g.: Mr. R. says about his brother that “The doctors insisted on the patient's presence at every follow up and if patient would not turn up then the doctor would assign last priority.”
Treatment-center-related issues
Some patients/family members would attribute treatment-center-related issues, including waiting period, inconvenience of the systems (e.g. being or not being open on holidays, when patient/family find it useful to attend), not having a single professional for successive visits, and unfriendly attitude of nonprofessional staff (problems related to professionals is rated elsewhere). The extent to which these issues have influenced discontinuation of treatment is detailed below.
Mr. K. says about his son that “my son was not keen on going to a hospital due to long waiting for a consultation, change in treating doctor.”
Mr. S. says about his daughter treatment that “We were apprehensive about the expenses entailed and also the possibility of giving bribe for obtaining treatment.”
Support/supervision from family/well-wishers
The extent to which caregivers help the patient in ensuring continued treatment include supervision of medications, accompanying him/her for consultation. Financial aspects of care are detailed under financial factors.
Mr. S. says about his brother that “We sought help of acquaintances when visiting the hospital but it was not possible on every subsequent visit.”
Mr. T. says about his brother that “We were preoccupied with more important issues like a property inheritance issue pending in the court and could not spare more money for obtaining treatment.”
Financial factors
Financial condition may influence continuation of the treatment in many ways such as the patient/family's expenses toward traveling, consultation, and the cost of medications.
Mr. K. says about his sister that “We are unable to spend money on her treatment due to lack of money and other family commitments, e.g. pending marriage of other siblings.”
Distance/transport-access to mental health center
Distance from the treatment center and transport-related issues may influence continuation of the treatment. These issues can be closely linked with financial difficulties. However, as it is related to distance/transport-related factors and not due to financial factors both factors were considered as different factors.
Mrs. M. says about her daughter that “The distance from home to hospital was more and it was not possible to travel often for seeking treatment or follow-ups.”
Logistic factors
A number of logistic factors could influence the continuation of treatment. These may be related to availability of prescribed medications, situations that prevented patients/family from traveling (e.g., floods, general strike,) [Factors, which could be better classified elsewhere, were not rated here: for instance, if the patient found it difficult to attend follow-up because she was a woman and it was inappropriate for her to travel alone, then it was mentioned under “gender of the patient.” If the problem was that of distance/travel, it was mentioned under “distance/travel.”].
Mrs. P. says about her husband that “I am daily wage worker in the hospital and find it inconvenient to seek my husband's treatment/follow-up on working days.”
Gender of the patient
In some situations, gender of the patient may influence continuation of the treatment. In general, factors that influence adherence (e.g., stigma) may have differential influence in males and females and the extent to which the gender issue has influenced continuation of the treatment is mentioned under this factor.
Age of the patient
Age of the patient may play an important role in influencing continuation of the treatment. This is particularly true in case of extremities in age. For instance, the family may be tolerant to symptoms and disability in patients who have crossed middle age due to their productivity. Alternatively, if the patient is teenager/young adult, the families may get concerned that medications may have adverse influence on their development.
Mr. R. says about his father: “My father is aged and unable to travel and he has gradually lost the ability to take important family decisions.”
Major life events
A number of social events, especially marriage, may cause patients/family to discontinue treatment. Other examples are harvest, functions in the family, death in the family, some other family member being sick, etc. The extent to which these factors influence treatment has been mentioned under this factor.
Mr. E. says about his wife: “if we want to come for regular follow up's of my wife's treatment we will not be able to carry out activities such as marriage of children, farming, attending social functions, attending death ceremonies, etc.”
Other medical conditions
Patients/families may be nonadherent in the context of comorbid medical conditions, for example, pregnancy, childbirth, accidents, serious medical illnesses. There may be situations when they could have continued treatment despite these conditions, but they may have been unaware of this. This “unawareness” has also been considered under this section.
Each of the families had more than one factor. Moreover, a complex interplay of these factors precluded them from accessing treatment. The frequencies of the most important factors.
DISCUSSION
In this study, we used a qualitative approach to understand factors that prevented patients from continuing medication treatment in a rural community of Karnataka. We found that a diverse set of factors drove patients toward discontinuation. Expectedly, each patient had more than one factor that prevented him/her from continuing psychiatric treatment. In fact, on an average, each patient and family had about four to five factors. In addition, there was a dynamic interplay of these factors rather than any single factor that determined medication discontinuation.
Several were well-known factors. These included lack of awareness about the illness, financial difficulties, distance, and transport. However, we identified many hitherto less-understood factors such as gender-related issues, treatment-center-related issues, frustration regarding long-term treatment, therapeutic relationship with mental health professionals. This was possible because of the qualitative narrative-based approach. This was in contrast to the checklist approach of earlier studies, in which the respondents are forced to choose from among a fixed list of factors. From the narratives of many patients and families, it was evident that these newly identified factors played a crucial role in preventing them from continuing psychiatric treatment. Thus, in some families, despite adequate awareness about the illness and reasonably comfortable financial situation, patients remained out of the treatment ambit.
Most important factors were lack of support and supervision by family members, lack of insight, and cooperation of the patient toward treatment. This finding is in contrast with many Western studies (Rosa et al. 2005, Buckley et al. 2007) in a manner that it highlights the importance of families in ensuring adherence. The important message to mental health professionals from our study is that mere prescription of antipsychotics will not ensure continuation of treatment.
Efforts toward increasing support of the family along with efforts to build the trust of the patient (working toward improving his/her insight) should be considered while prescribing medications. In most cases, patients who are symptom-free after recovering from acute psychosis episode may decide to stop medications as they believe that they have achieved premorbid states of functioning.
At this stage, families loosen their guard and provide less supervision. This could lead to relapse and exacerbation of psychiatric symptoms and further deterioration of insight. In this context, focusing on adherence management at the time that the patient is relatively well becomes crucial. The most important message from this study is the fact that nonadherence is multifactorial (E.g.,: Financial factors, distance, and treatment-center-related issue). It is obvious that for busy clinicians, as the family or patient may not provide details of all factors in a brief interview (in other words they may highlight the factor without revealing other less important factors), the clinician may end up addressing only one factor, not understanding the complex dynamics across the multiple factors. This may not be sufficient, as unless the complex web of factors is addressed, adherence may not be ensured.
Strengths of the study
Proactive steps were taken to include community-dwelling patients who had discontinued treatment from long time. Any hospital-based study would have missed such patients. Our study thus is a unique one.
Limitation of the study
We were able to interview only such patients, who were living with their family members. There were many patients in the community, who had no families. As they too have rights to optimal treatment, it is important to understand factors that prevent them from accessing treatment. In fact, many villagers expressed helplessness in getting them for treatment. Because of ethical issues related to consent, we were unable to recruit them.
CONCLUSIONS
A diverse set of interrelated factors contributes to medication discontinuation in persons with schizophrenia who live in rural communities. Clinicians need to be aware of this reality and address them comprehensively to retain patients under the treatment ambit.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The researchers would like to thank ASHA workers, health workers, and Primary health doctors in Turuvekere community, which helped in the identification of patients in the community.
REFERENCES
- Patients who discontinue day hospitalization – An analysis. Indian J Psychiatry. 1987;29:197-201.
- [Google Scholar]
- A profile of the follow up of the rural mentally ill. Indian J Psychiatry. 1981;2:139-41.
- [Google Scholar]
- Patter of Follow up Visits in a Rural Psychiatric Clinic. Indian J Psychiatry. 1987;29:189-95.
- [Google Scholar]
- Development of case Vignettes to assess the mental health training of primary care medical officers. Acta Psychiatr Scand. 1990;82:174-77.
- [Google Scholar]
- Evaluation of the factors interfering with drug treatment compliance among Brazilian patients with schizophrenia. Rev Bras Psiquiatr. 2005;27:2-11.
- [Google Scholar]
- Lack of Insight in Schizophrenia: Impact on Treatment Adherence. CNS Drugs. 2007;21:129-141.
- [Google Scholar]
- Brief report: Families of rural mentally ill and treatment adherence in district mental health programme. Int J Soc Psychiatry. 1996;42:68-72.
- [Google Scholar]
- Community outreach for untreated schizophrenia in rural India: A follow-up study of symptoms, disability, family burden and costs. Psychol Med. 2005;35:341-51.
- [Google Scholar]
- Reasons for schizophrenia patients remaining out of treatment: Results from a prospective study in a rural South Indian Community. Indian J Psychol Med. 2016;38:101-4.
- [Google Scholar]
- Factors affecting the reporting of mental disorder in others. J Soc Psychiatry Psychiatr Epidemiol. 1975;10:87-95.
- [Google Scholar]
- The mini-international neuropsychiatric interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22-33.
- [Google Scholar]
- The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261-76.
- [Google Scholar]
- Rehabilitation Committee of Indian Psychiatric Society: Indian Disability Evaluation and Assessment Scale: Assessment Scale: A Scale for Measuring and Quantifying Disability in Mental Disorders. Kolkata: Indian Psychiatric Society; 2002.
- 2007. 21:129-41. Available from: http://www.mohfw.nic.in/NRHM/asha.htm






